Classifying Psychological Disorders | Psychology and Sociology for MCAT PDF Download
It is important to understand the classification of psychological disorders in order to understand the symptoms and prevalence of each. Without classification, it would be impossible to know what the biological and genetic risk factors are, and which treatments work the best. The universal authority on the classification and diagnosis of psychological disorders is the Diagnostic and Statistical Manual of Mental Disorders (DSM).
The fifth edition of the DSM (the DSM-5) was published in May of 2013; each new edition of the DSM reflects changes in the current thinking and practice concerning certain psychological disorders. For example, in the 19 years since the publication of the fourth edition (the DSM-IV), research findings and clinical experience prompted the publishers of the DSM-5 to combine the four separate autism disorders into one, Autism Spectrum Disorder, and to change the symptom categories from three to two areas.
While the change caused some controversy in the autism community, the idea behind the change is that it reflected the most current research and practice on the disorder, and represented a better, more accurate means for diagnosis. Accurate diagnosis is critical; most insurance companies require a diagnosis based on DSM criteria before they will cover the cost of therapy.
Much of the criteria for categorizing psychological disorders was changed drastically between the DSM-IV and DSM-5; therefore, for the purposes of the MCAT, familiarize yourself with the broad general categories of disorders in Table 6 (note, this list is neither all-inclusive nor exhaustive, but represents some of the most common psychological disorders).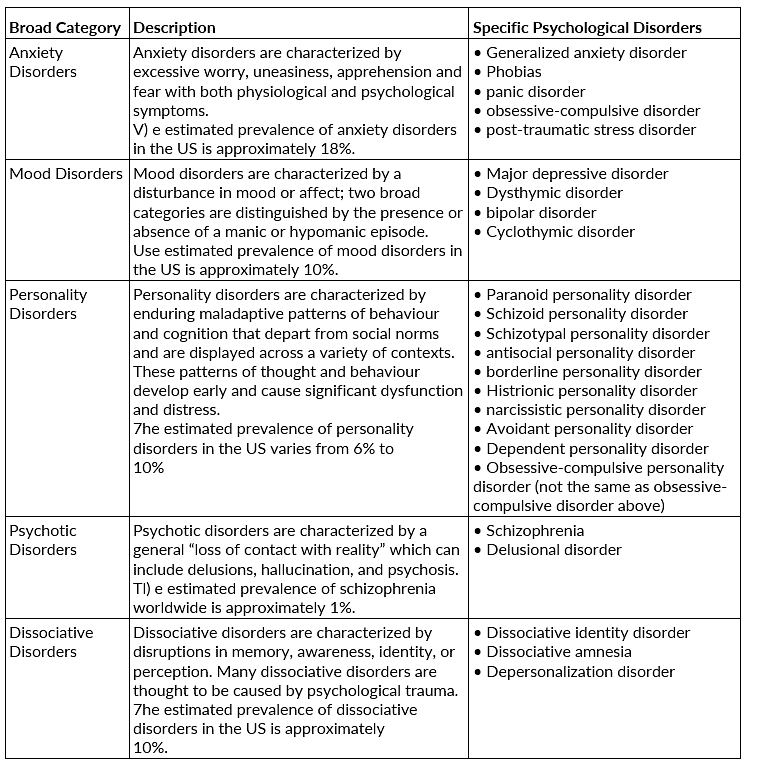
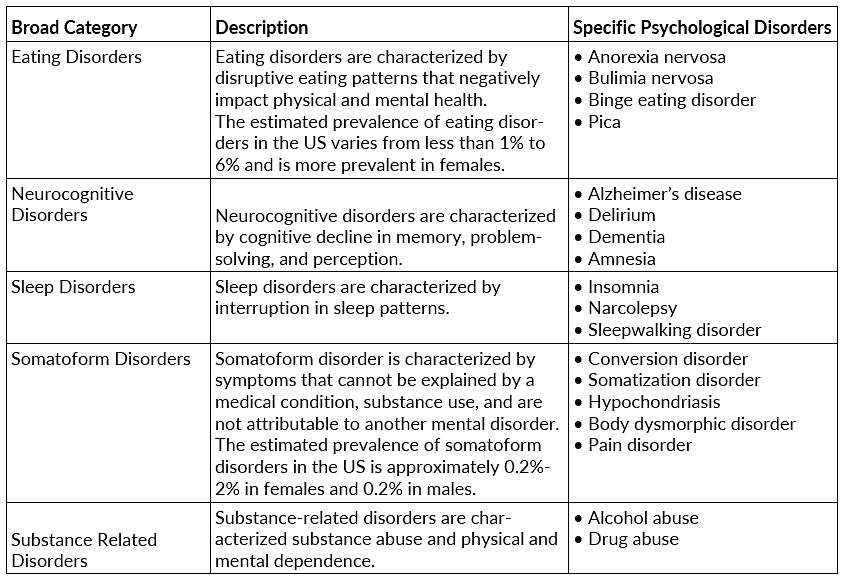
Table 6 Categories of Psychological Disorders
Types of Psychological Disorders
Six categories of psychological disorders are discussed in this section: anxiety disorders, somatoform disorders, mood disorders, schizophrenia, dissociative disorders, and personality disorders.
Anxiety Disorders
- Anxiety is an emotional state of unpleasant physical and mental arousal—a preparation to fight or flee. In a person with an anxiety disorder, the anxiety is intense, frequent, irrational (out of proportion), and uncontrollable; it causes significant distress or impairment of normal functioning. Seven types of anxiety disorders are discussed here: panic disorder, generalized anxiety disorder, specific phobia, social phobia, posttraumatic stress disorder, acute stress disorder, and obsessive-compulsive disorder.
- Symptoms mimicking an anxiety disorder can also be caused by general medical conditions, alcohol, certain drugs, or medication use or withdrawal. If a person has a medical condition or uses substances that are likely to be causing the symptoms, the diagnosis is “anxiety disorder due to a general medical condition” or “substance-induced anxiety disorder.”
- Panic Disorder. A person with panic disorder has suffered at least one panic attack and is worried about having more of them. The panic attacks can be cued by certain situations, but they are more often uncued or “spontaneous,” occurring frequently and unexpectedly.
- During a panic attack, a person commonly experiences intense dread, along with shortness of breath, chest pain, a choking sensation, and cardiac symptoms such as a rapid heartbeat or palpitations. There may also be trembling, sweating, lightheadedness, or chills. Many fear they are dying of a heart attack or stroke during a panic attack.
- One danger of panic attacks is that they can mask other illnesses, such as heart attacks and mood disorders. Although panic attacks are brief (often less than 30 minutes), they can be excruciating, and people with panic disorder fear having more panic attacks. Panic disorder can be debilitating if left untreated, but people with this disorder do respond well to treatment.
- Generalized Anxiety Disorder. A person with generalized anxiety disorder (GAD) feels tense or anxious much of the time about many issues, but does not experience panic attacks. The source of this low-key, chronic nervousness can seem like a moving target, shifting from one situation to another, or there may be no identifiable source.
- The distress and impairment associated with GAD is not severe; it may include restlessness, tiring easily, poor concentration, irritability, muscle tension, and insomnia or restless sleep.
- Specific Phobia and Social Phobia. There are two types of phobias. In both, the sufferer feels a strong fear that he or she recognizes as unreasonable. He or she nevertheless almost always experiences either general anxiety or a full panic attack when confronted with the feared object or situation. People with phobias often go to great lengths to avoid the triggers they fear.
- Specific phobia is a persistent, strong, and unreasonable fear of a certain object or situation. Specific phobias are classified into four types depending on the types of triggers they involve.
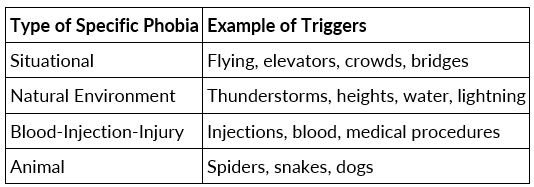 Types of Specific Phobias
Types of Specific Phobias
- Social phobia is an unreasonable, paralyzing fear of feeling embarrassed or humiliated while one is watched by others, even while performing routine activities such as eating in public or using a public restroom. Posttraumatic Stress Disorder and Acute Stress Disorder.
- Posttraumatic stress disorder (PTSD) can arise when a person feels intense fear, horror, or helplessness while experiencing, witnessing, or otherwise confronting an extremely traumatic event that involves actual or threatened death or serious injury to the self or others. It is estimated that most people (more than half) will experience at least one traumatic event in their lifetime, but only a minority will develop PTSD. Approximately 8% of men and 20% of women develop PTSD after a trauma. Rates of PTSD are higher in males who have served in active combat, estimated to be up to 20%.
- The traumatic event can be relived through dreams, flashbacks (which feel as though the event is currently happening), and intrusive, distressing thoughts and images. Some experience mental or physiological distress (for example, elevated heart rate or blood pressure) when reminded of the event.
- A person with PTSD tries to avoid people, places, feelings, thoughts, or conversations that are reminders of the event, or even avoids people and feelings in general. The person is also chronically physiologically hyperaroused, with symptoms such as an increased startle response, insomnia, angry outbursts, poor concentration, and vigilance.
- For a diagnosis of PTSD, these symptoms must have been present for more than a month. Acute stress disorder is similar to PTSD, but its symptoms are present for a month or less.
- Obsessive-Compulsive Disorder. A person with obsessive-compulsive disorder (OCD) have obsessions, compulsions, or both. Obsessions are repeated, intrusive, uncontrollable thoughts or impulses that cause distress or anxiety.
- The person knows the thoughts are irrational, and tries to disregard or suppress them, or to neutralize them through a compulsive behavior. Compulsions are repeated physical or mental behaviors (for example, counting or touching certain items in a specific manner) that are done in response to an obsession or in accordance with a set of strict rules, in order to reduce distress or prevent something dreaded from occurring.
- The person realizes that the compulsive behavior is not reasonable, being either unrelated to the dreaded event, or related but clearly excessive. Nevertheless, if the person does not perform the behavior, he or she feels intense anxiety and a conviction that the terrible event will happen. Some common obsessions and compulsions are listed in Table.
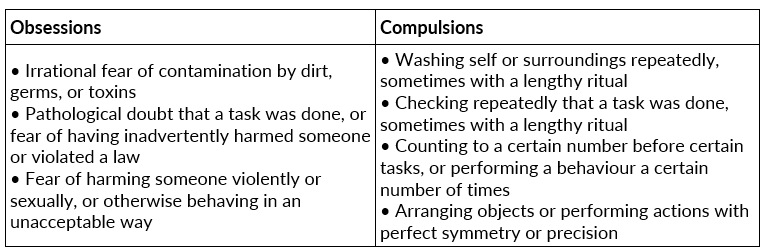 common Obsessions and Compulsions
common Obsessions and Compulsions
Somatoform Disorders
- A somatoform disorder is a psychological disorder characterized primarily by physical symptoms and concerns, which may mimic physical (somatic) disease. However, the symptoms are not explainable medically and do not improve with medical treatment. People with somatoform disorders genuinely experience their symptoms and believe that there is something physically wrong with them.
- A different disorder is diagnosed when a person consciously fakes symptoms either to achieve the role of a sick person or for material benefits. Five types of somatoform disorder are discussed in this section: conversion disorder, pain disorder, somatization disorder, body dysmorphic disorder, and hypochondriasis.
- Conversion Disorder. A person with conversion disorder experiences a change in sensory or motor function that has no discernible physical or physiological cause, and which seems to be significantly affected by psychological factors. The symptoms of conversion disorder begin or worsen after an emotional conflict or other stressor. The terminology suggests that the emotion or anxiety is converted into a physical symptom.
- The change in function is severe enough to warrant medical attention, or to cause significant distress or impairment in work, social, or personal functioning. For example, a person with conversion disorder may suddenly experience blindness for which doctors can find no physical cause, with the blink reflex intact. A different disorder is diagnosed when the problem is limited to pain or to sexual dysfunction.
- Pain Disorder. A person with pain disorder (previously called chronic pain syndrome) suffers clinically important pain whose onset or severity seems significantly affected by psychological factors. The pain causes significant distress or impairment in work, social, or personal functioning. A different disorder is diagnosed when the pain is limited to sexual intercourse, or when it is better explained by another psychological disorder. Somatization Disorder.
- A person with somatization disorder experiences a variety of physical symptoms over an extended time period. A person with somatization disorder has had at least eight of the following physical symptoms that began before age 30, occurred over several years, and were not fully explained by any physical or physiological cause
- pain in at least four areas of the body,
- at least two gastrointestinal symptoms (not including pain),
- at least one sexual symptom, and
- at least one pseudoneurological symptoms (for example, poor balance or double vision).
- The symptoms have caused significant impairment in work, social, or personal functioning, or prompted the person to seek medical treatment.
- Body Dysmorphic Disorder. A person with body dysmorphic disorder is preoccupied with a slight physical anomaly or imagined defect in appearance, often involving the face, hair, breasts, or genitalia. The preoccupation causes significant distress or impairment in work, social, or personal functioning, and it is not better explained by another psychological disorder. Hypochondriasis.
- A person with hypochondriasis has been preoccupied with fears of having a serious illness for at least six months. The fears are based on a misinterpretation of bodily symptoms, and they are not relieved when medical investigation reveals no illness. A different disorder is diagnosed if the ideas are delusional or better explained by a mood, anxiety, or other somatoform disorder.
Schizophrenia
Schizophrenia is a chronic, incapacitating disorder by which a person is out of touch with reality (psychotic) and suffers material impairment in social, occupational, or personal functioning. A person with schizophrenia has suffered at least two clear symptoms of psychosis for a significant portion of one month, along with less extreme symptoms for at least six months.
Symptoms of psychosis are classified as positive, meaning something has been added, or negative, meaning something has been taken away. The positive symptoms of psychosis include delusions, hallucinations, disorganized speech, and disorganized or catatonic behavior (if the delusion or hallucination is bizarre, schizophrenia can be diagnosed with just that one symptom of psychosis).
The negative symptoms of psychosis include reduced or absent emotional expression (flat or blunted affect), reduced quantity or fluency of speech, and reduced initiative or will to do things (avolition). Many people incorrectly use the term schizophrenia to mean having multiple personalities or identities (that condition is actually called dissociative identity disorder; see below).
Although schizophrenia literally means “split mind,” it refers to a split in mental functions, or a split from reality; it does not indicate a split in identity. There are five main types of schizophrenia, distinguished by the type of psychosis the person experiences.
Schizophrenia, Paranoid Type. In a person with paranoid-type schizophrenia, the
|
339 videos|20 docs|42 tests
|















