Test: Anatomy - 1 - NEET PG MCQ
25 Questions MCQ Test - Test: Anatomy - 1
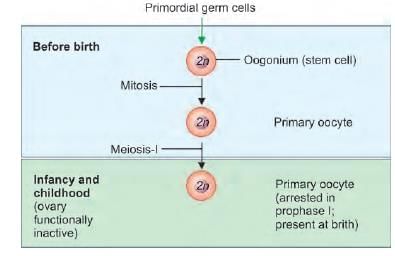
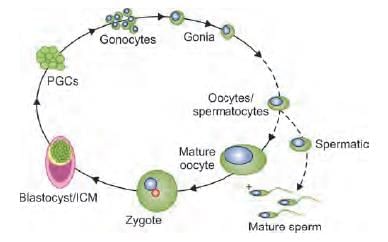
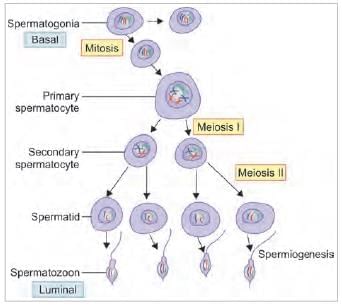
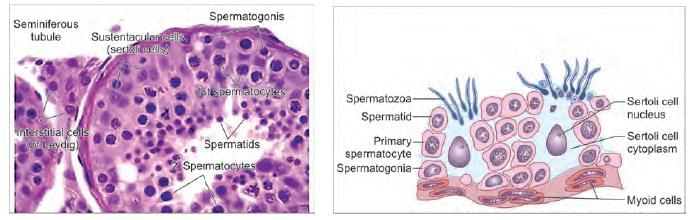
Arrange the steps of spermatogenesis in a sequence: (AIIMS May 2019)
1. Spermatid
2. Spermatocyte
3. Spermatogonium
4. Spermatozoa
1. Spermatid
2. Spermatocyte
3. Spermatogonium
4. Spermatozoa
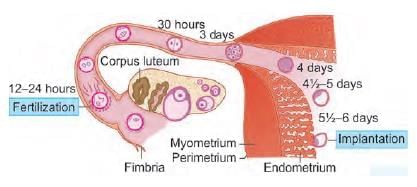
Meiosis Fertilization occurs in which part of the fallopian tube: (NEET-PG 2020)
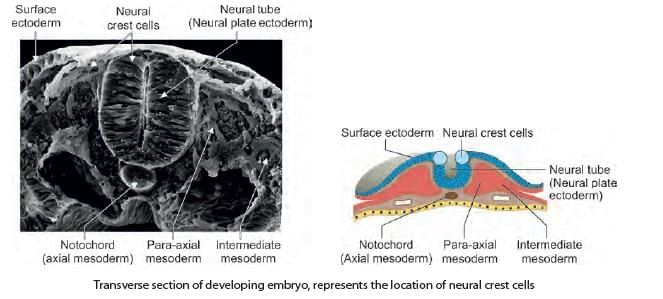
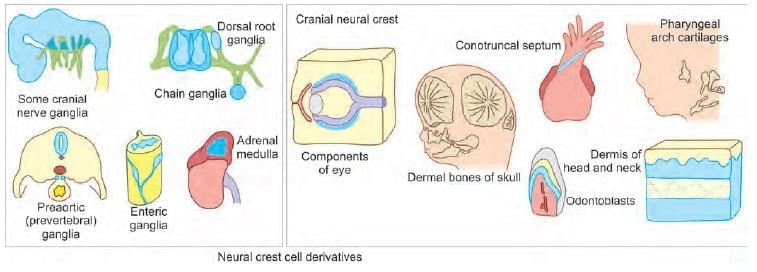
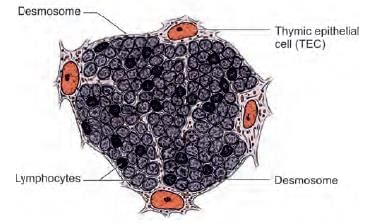
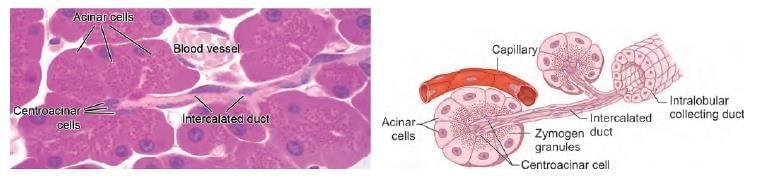
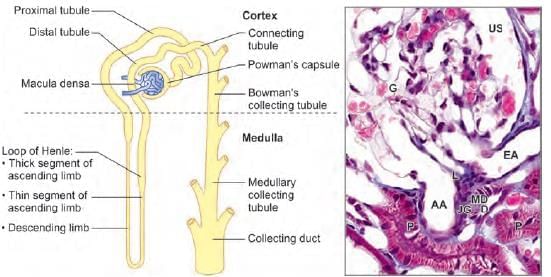
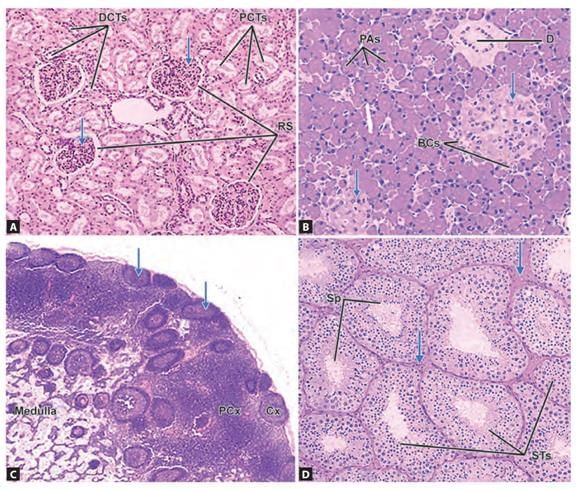
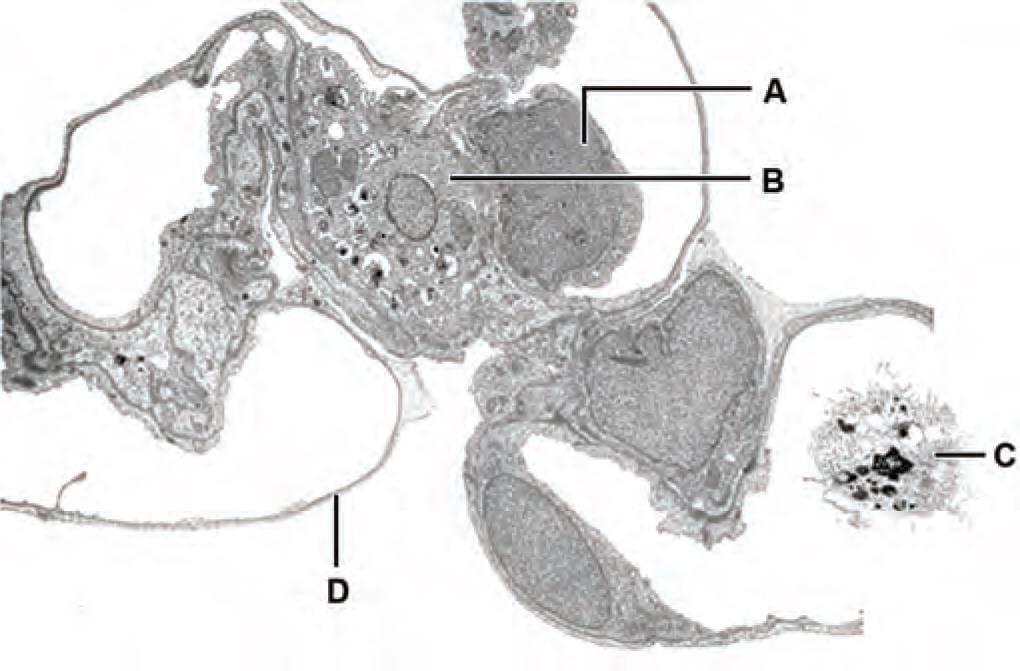
Which of the following are derived from the star marked region? (INI-CET Nov 2022)

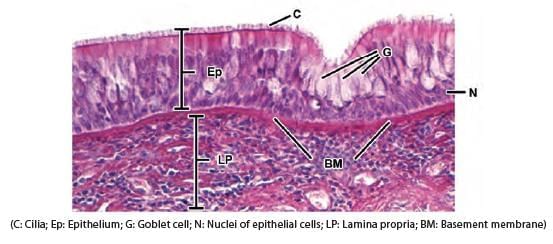
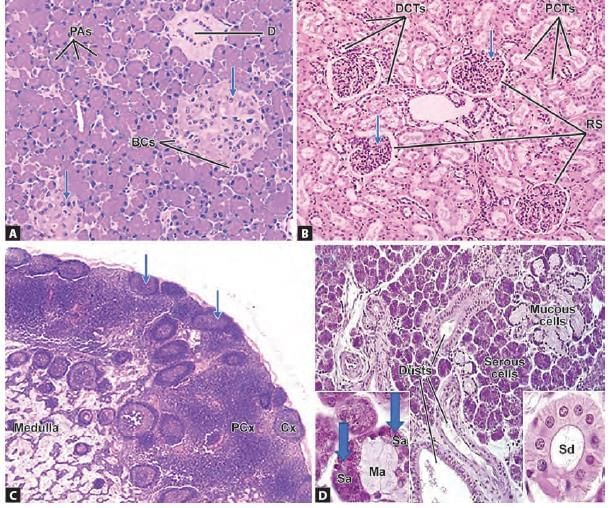
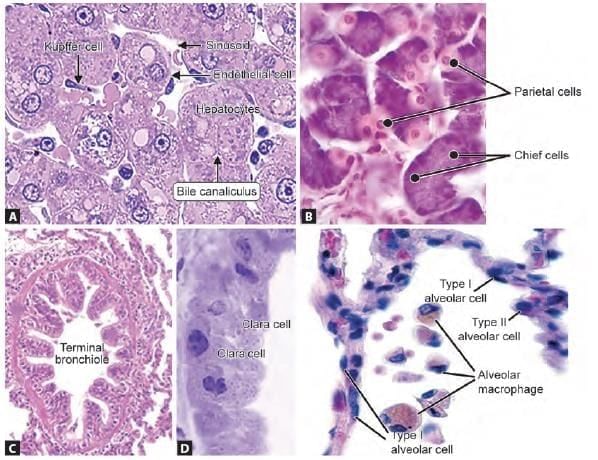
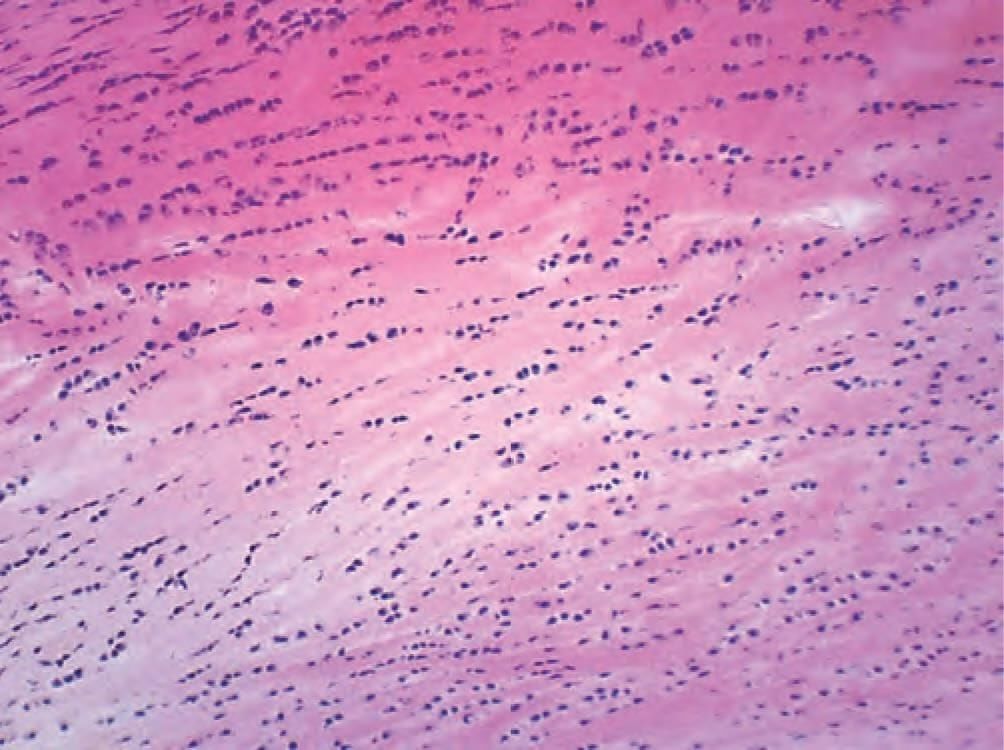
Which of the following pair is WRONGLY matched for the following microscopic picture? (INI-CET Nov 2021)
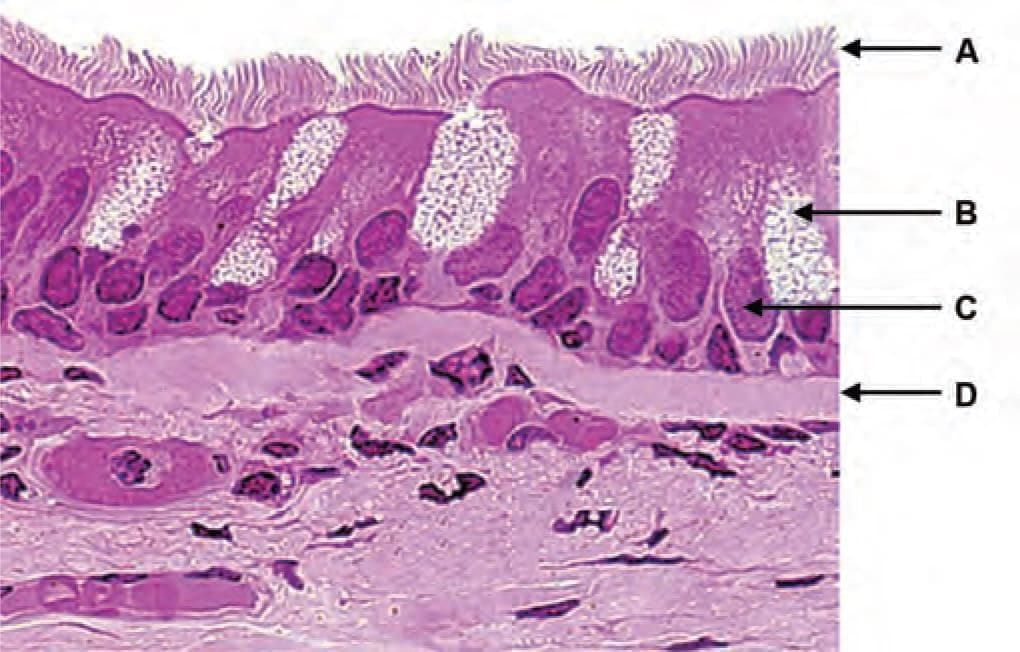
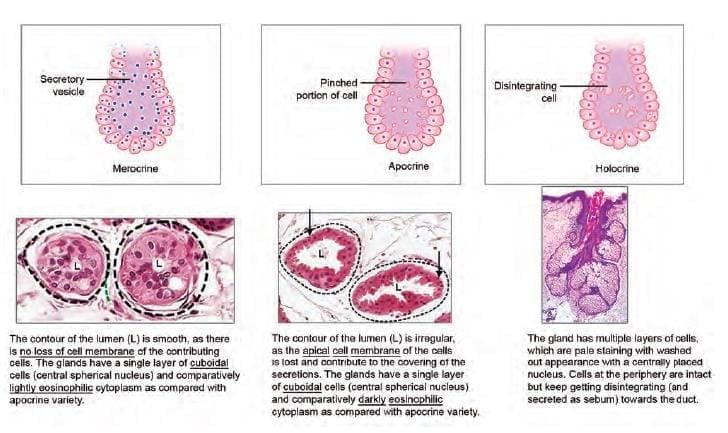
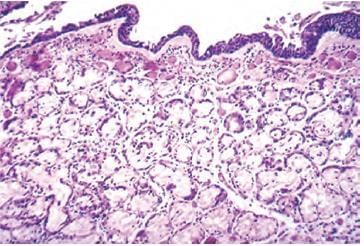
Which of the following marked structures represent merocrine gland? (INI-CET May 2022)
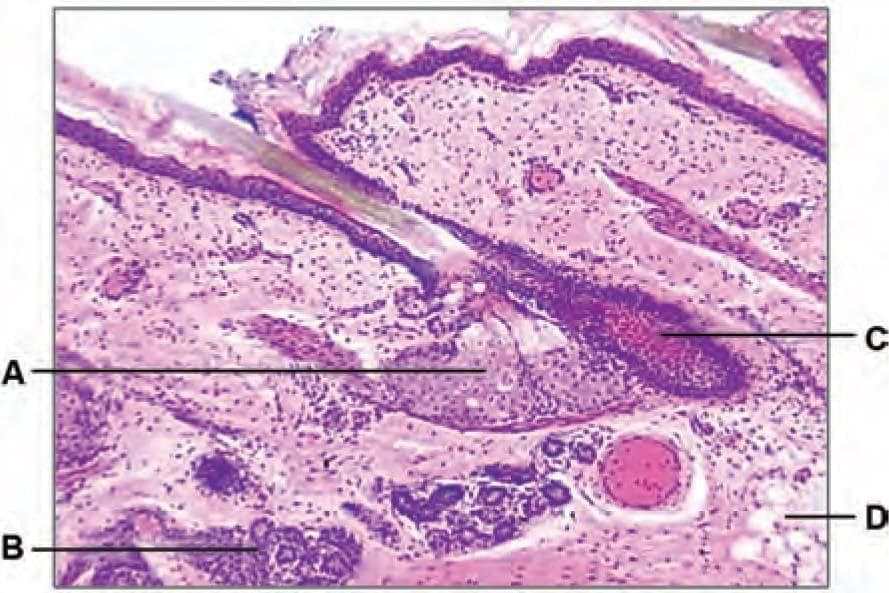
Identify the structure in the given microscopic picture: (NEET-PG 2022)
Receptor responsible for tactile discrimination is: (INI-CET July 2021)
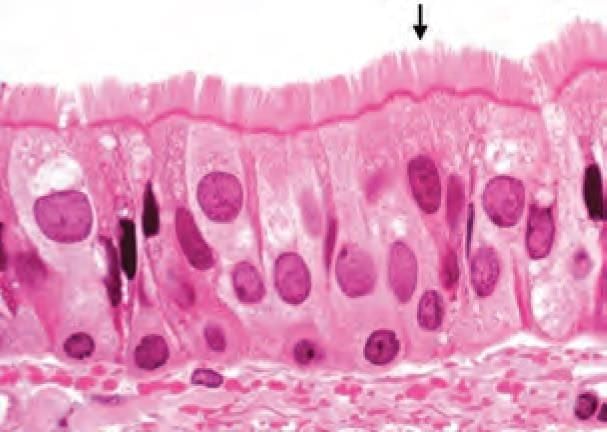
A 45-year-old chronic smoker presented with the complaints of cough. A biopsy was taken after the preliminary examination. What is cellular change visible on the biopsy? (NEET-PG 2020p)
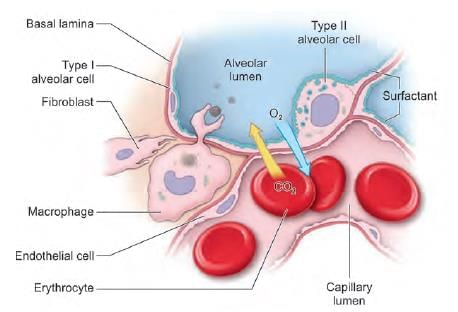
Which of the marked cells in the following picture is involved in respiratory distress syndrome: (INI-CET Nov 2021)
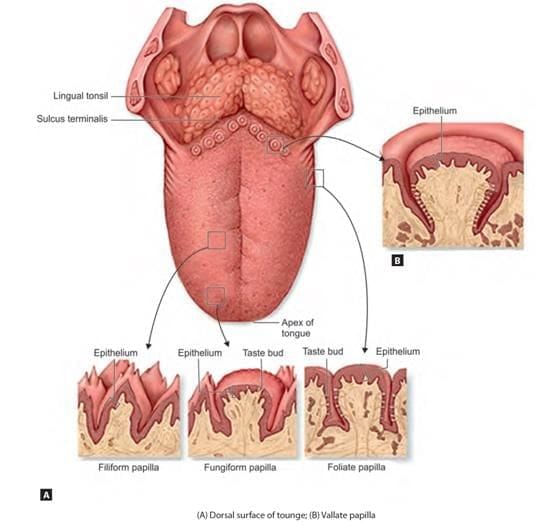
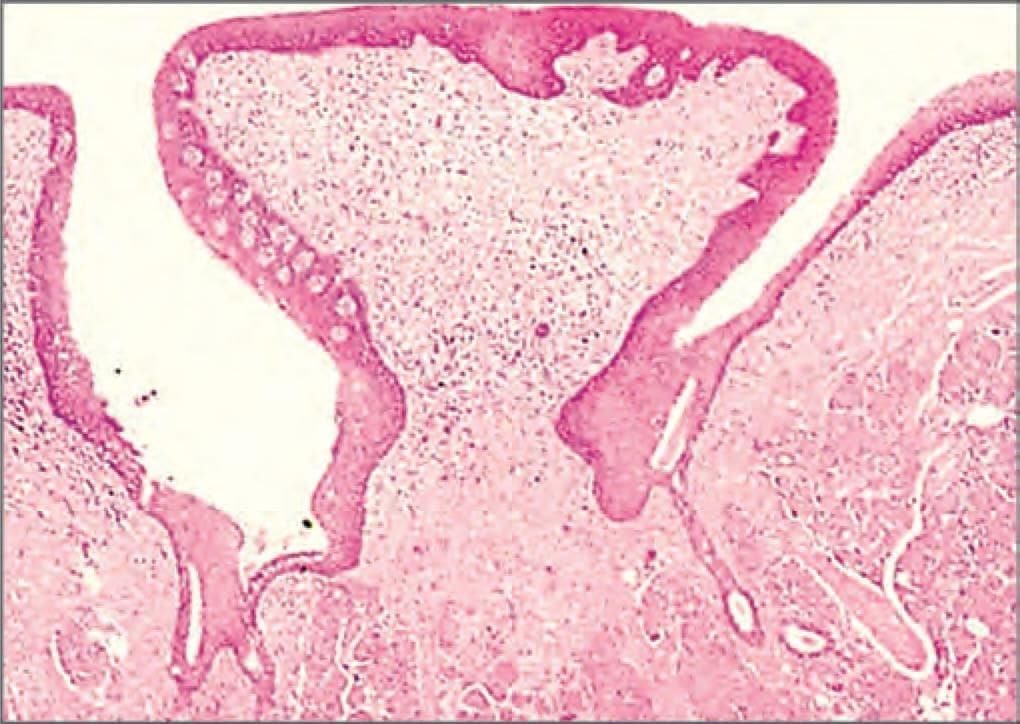
Identify the type of papillae shown in the microscopic picture of tongue: (NEET-PG 2021)
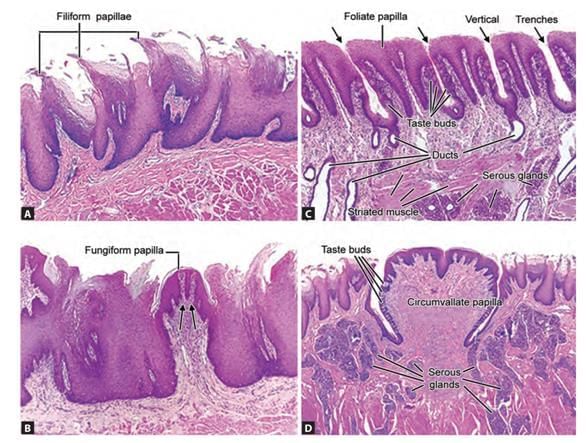
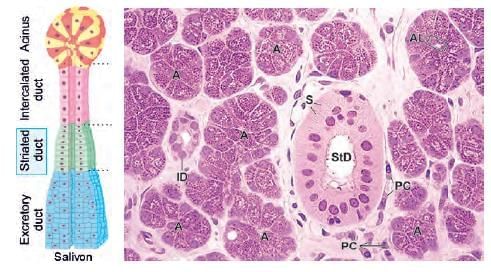
Exocrine pancreas differs from parotid gland histologically by: (AIIMS June 2020)
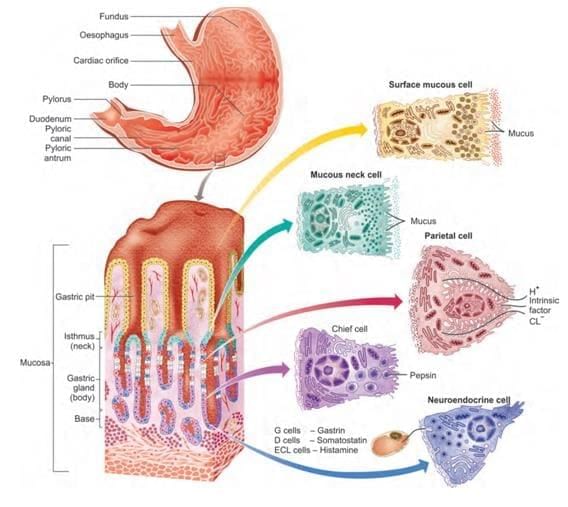
Predominant cells present at isthmus of gastric pit: (AIIMS June 2020)
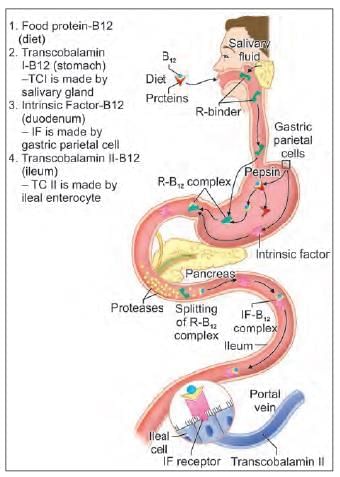
A young male met with a motor bike accident and had severe injury to ileum and jejunum. Therefore, the entire ileum and partial jejunum was resected. Which of the following would the patient suffer from? (NEET-PG 2020)
Arrange the following cells in basal to luminal side order: (INI-CET May 2022)
1. Spermatogonium
2. Spermatozoa
3. Primary spermatocyte
4. Spermatid
5. Myofibroblast
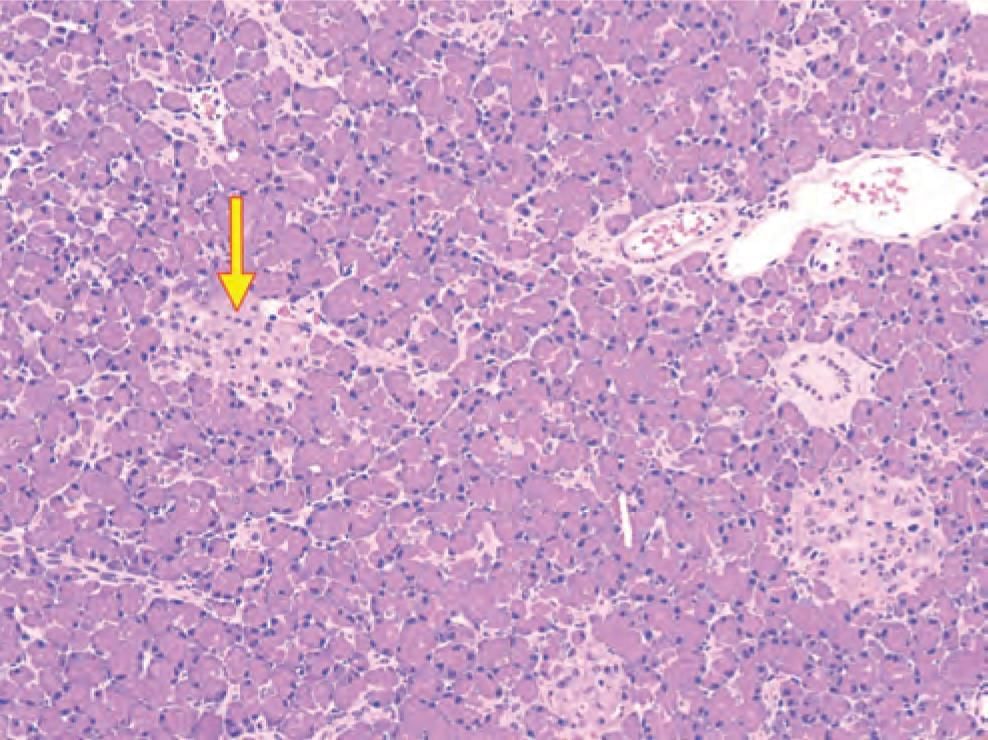
Identify the arrow marked structure in the microscopic picture: (NEET-PG 2023)
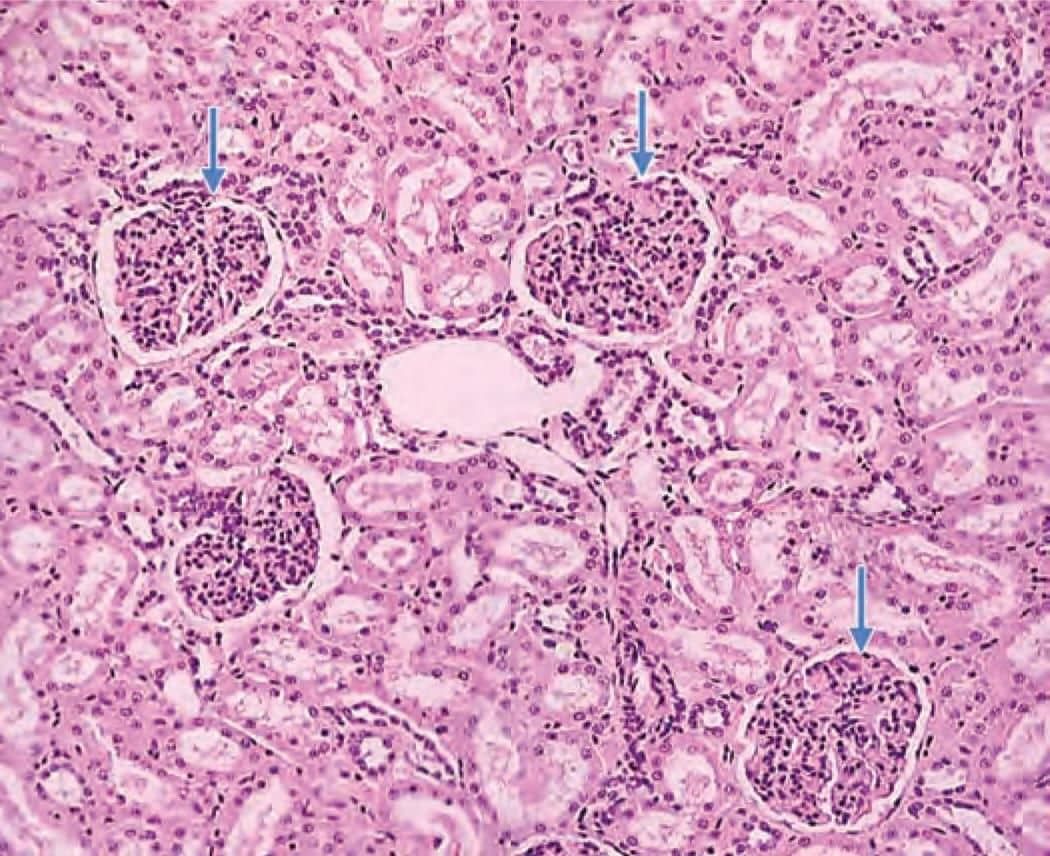
Identify the arrow marked structure in the given microscopic picture: (NEET-PG 2022)