Test: Anatomy - 6 - NEET PG MCQ
25 Questions MCQ Test - Test: Anatomy - 6
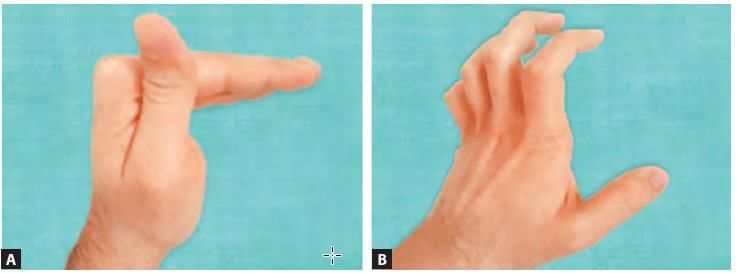
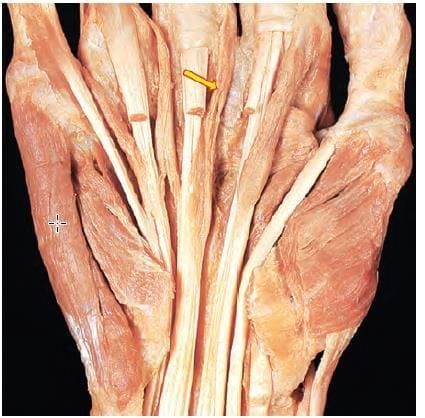
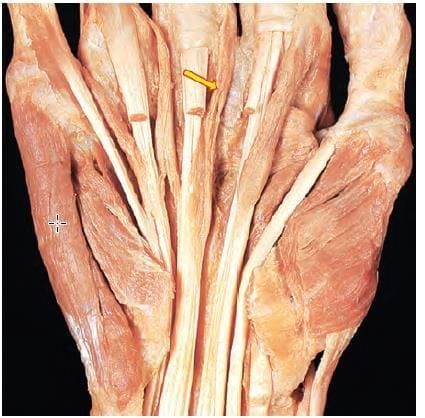
A 30 years female patient is presenting with wrist pain on lateral side. On examination the following test was positive. Tendon sheaths of which two muscle have been involved? (NEET-PG 2020p)


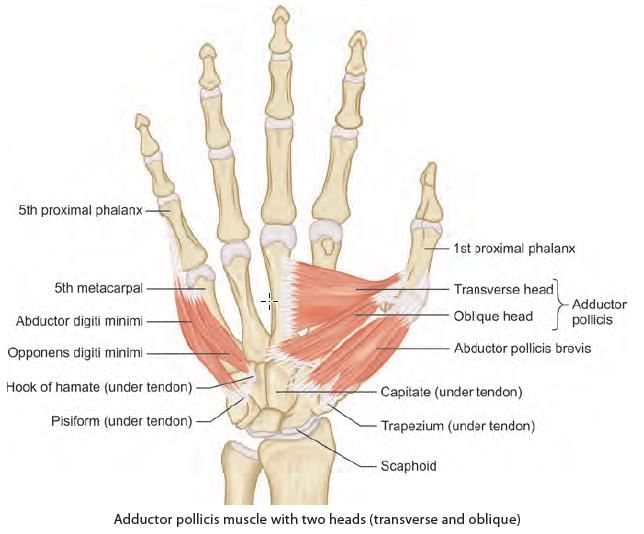
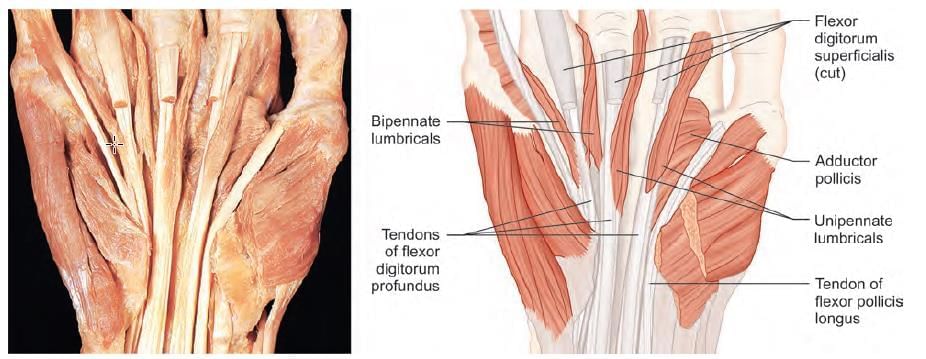
Mention the nerve supply of the marked muscle: (INI-CET May 2022)
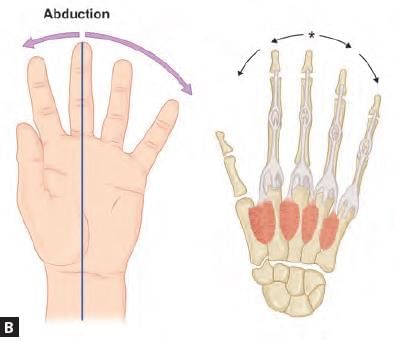
Hand deformity presenting as hyper-extension at the metacarpo-phalangeal joint and flexion at inter-phalangeal joint, occurs due to paralyzed: (NEET-PG 2020p)
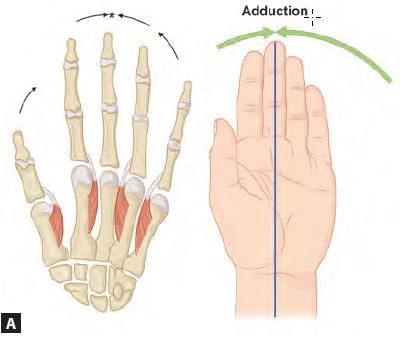
Which of the following finger has two dorsal interossei? (AIIMS May 2019)
Which of the structure does not contribute to the pointed structure? (AIIMS Nov 2019)

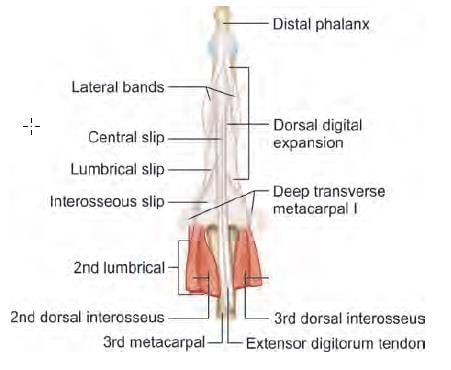
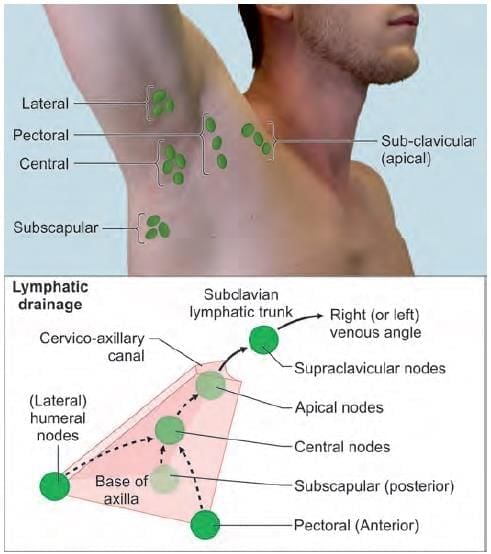
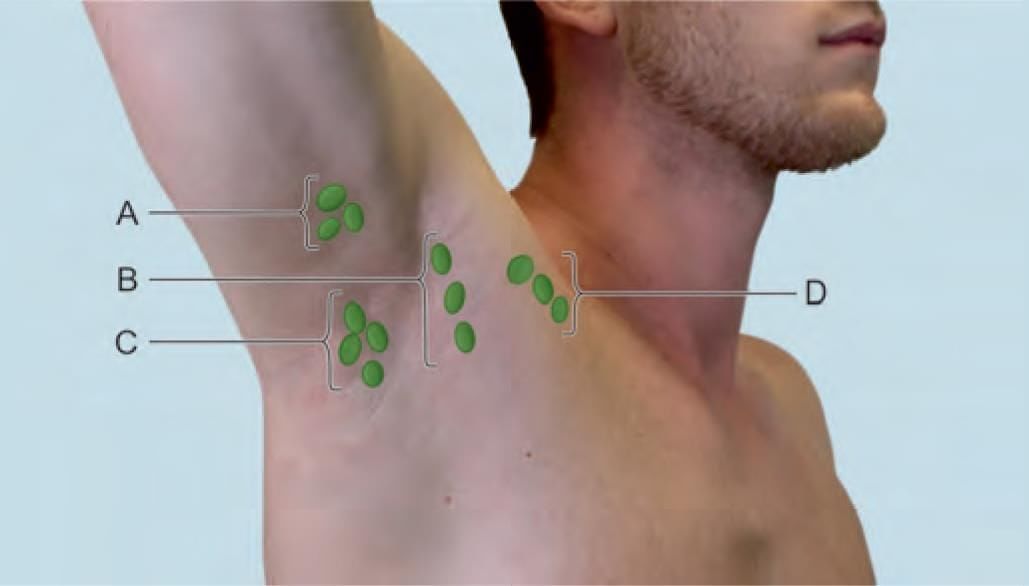
Choose the CORRECT matching pair for axillary lymph nodes in the given diagram: (INI-CET Nov 2022)
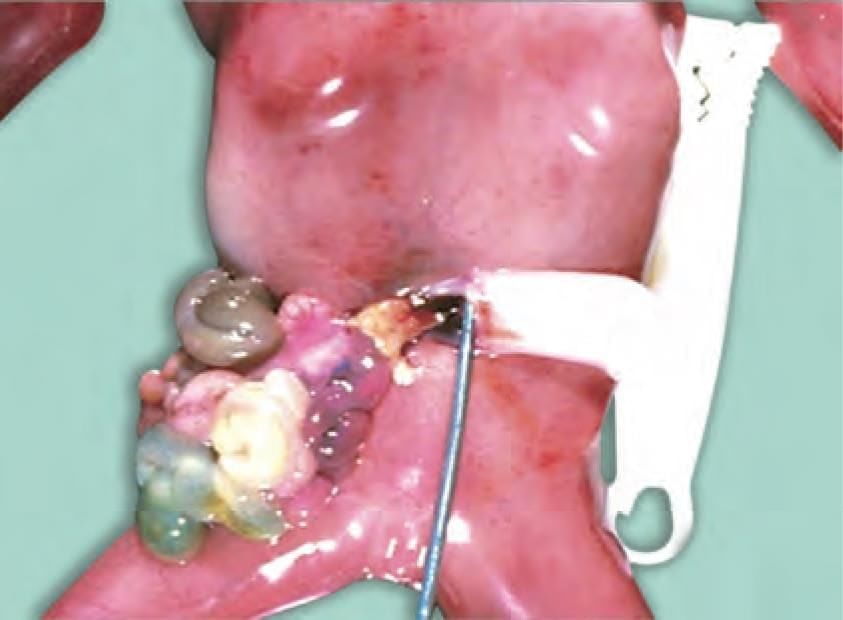
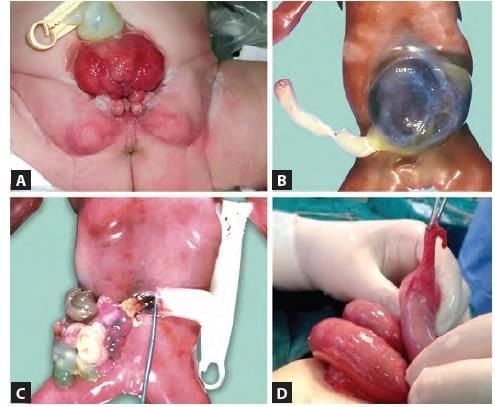
Identify the congenital anomaly shown in the newborn baby: (NEET-PG 2022)

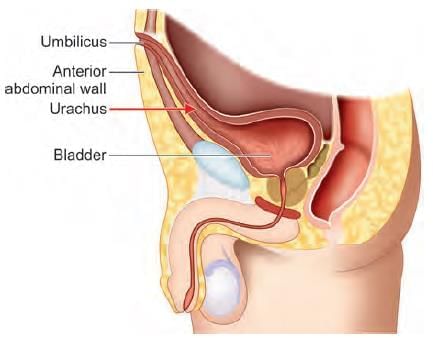
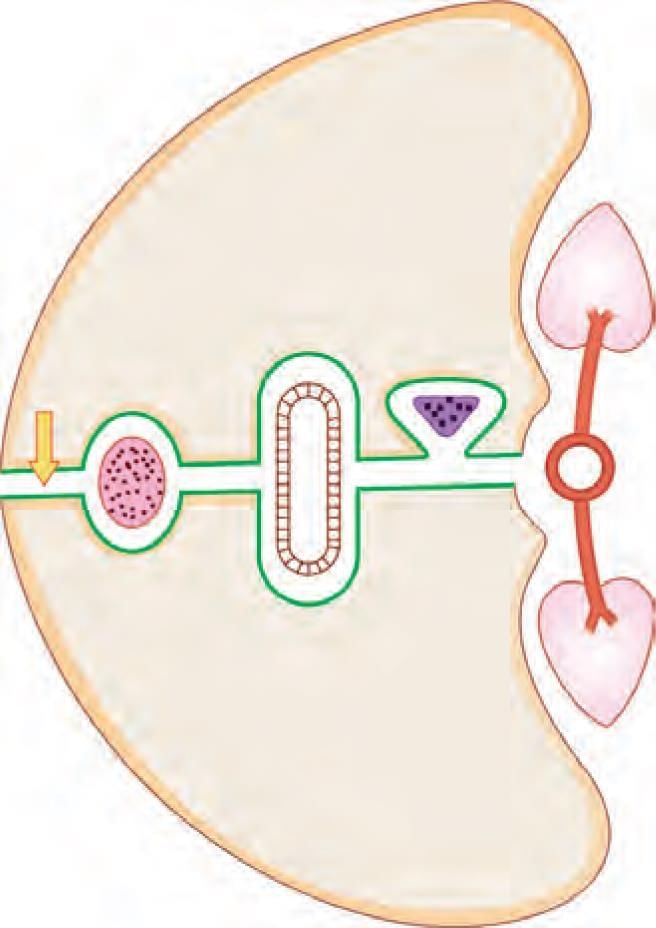
Adult derivative of the arrow marked structure in the following diagram is: (NEET-PG 2023)
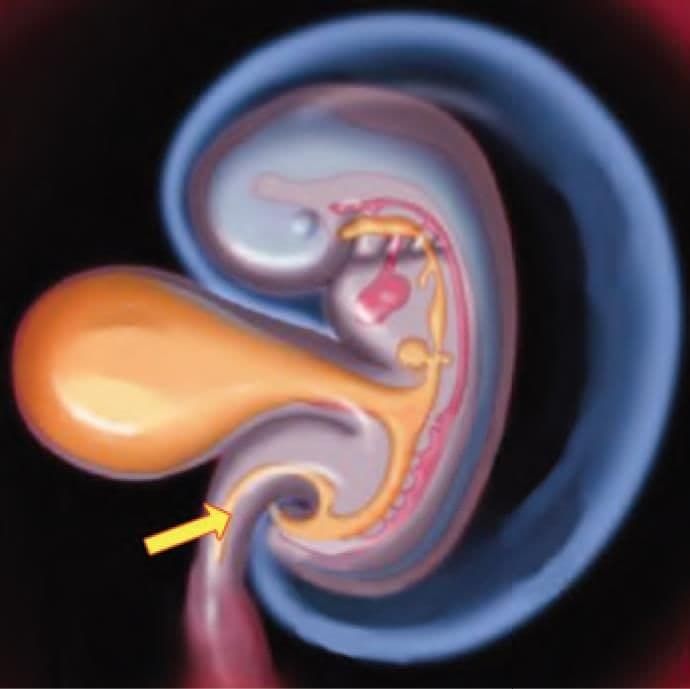
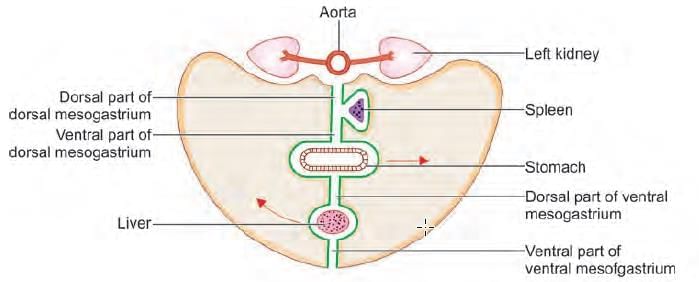
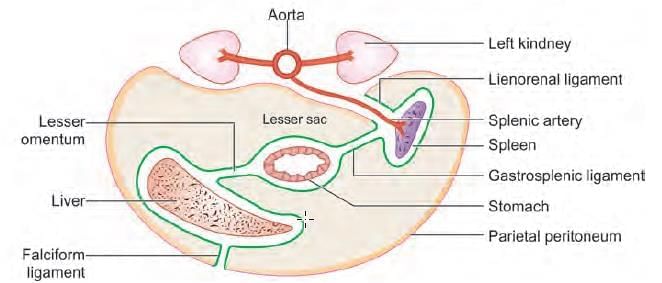
Which of the following ligament develop in the arrow marked structure? (NEET-PG 2022)
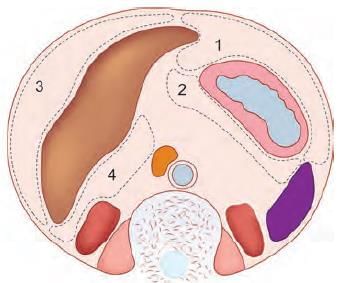
Which of the following is most common site for intraperitoneal abscess in relation to liver? (NEET-PG 2022)
The anatomical structure at the arrow marked location is a defect in: (NEET-PG 2023)

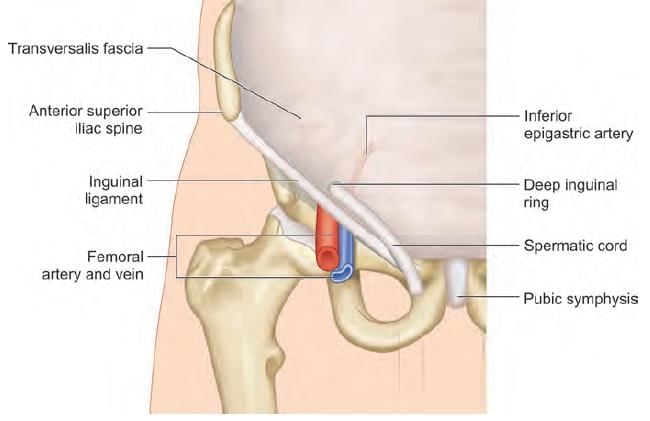
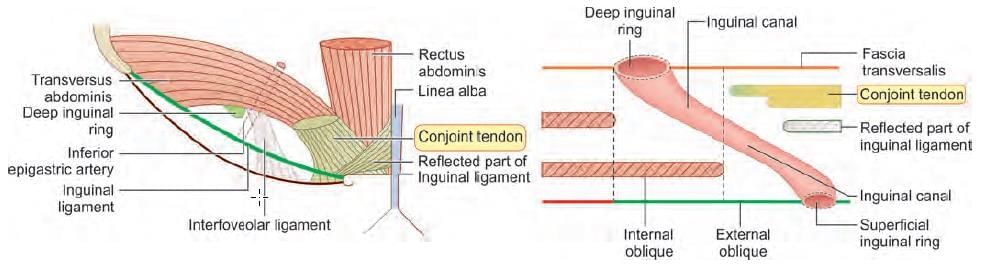
Hernia lying medial to inferior epigastric artery and superior to pubic tubercle, occurs due to weakness in: (NEET-PG 2023)
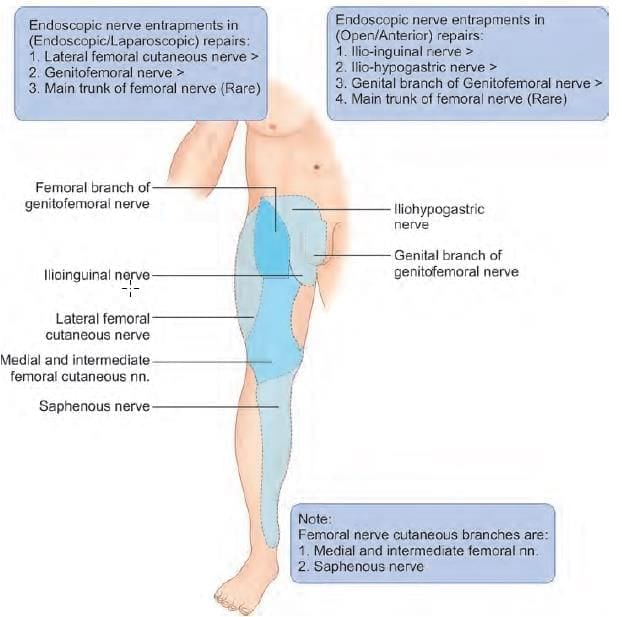
A patient has presented with pain in the right leg region for past 3 months. There is a surgical history of undergoing laparoscopic bilateral inguinal hernia repair. The nerve involved is: (NEET-PG 2023)
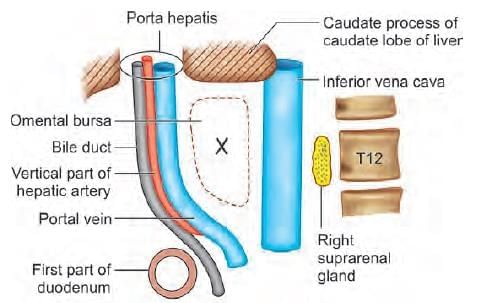
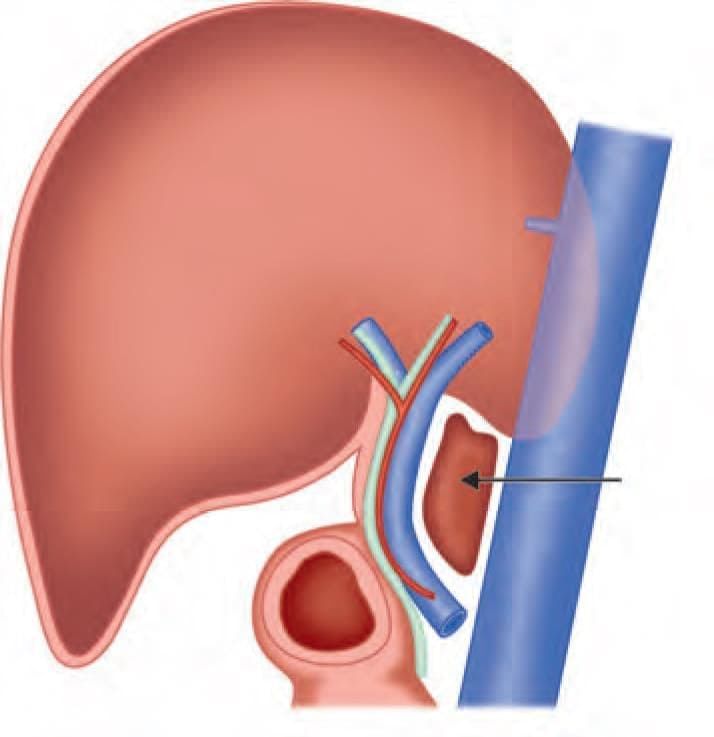
Superior boundary of the arrow marked structure is: (INI-CET July 2021)
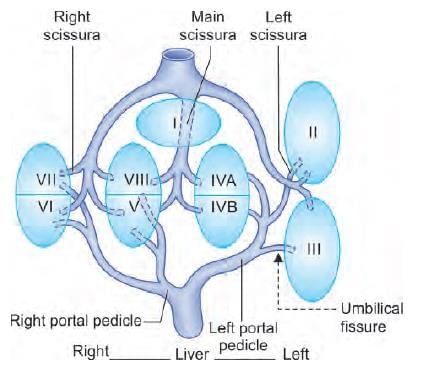
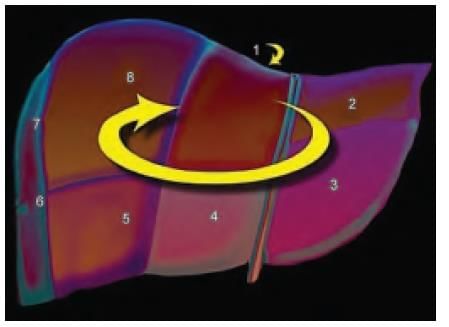
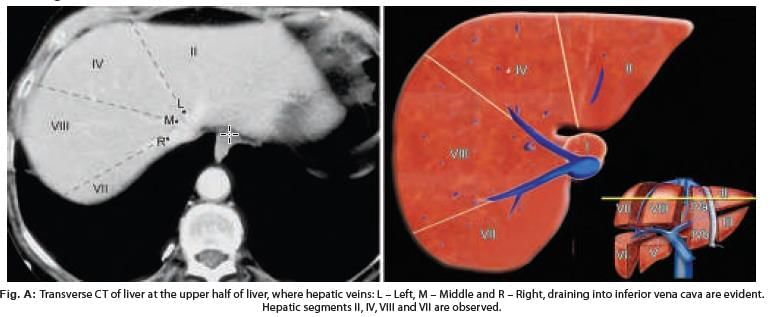
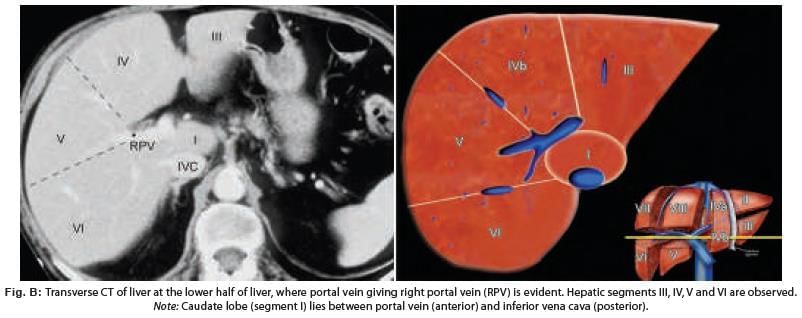
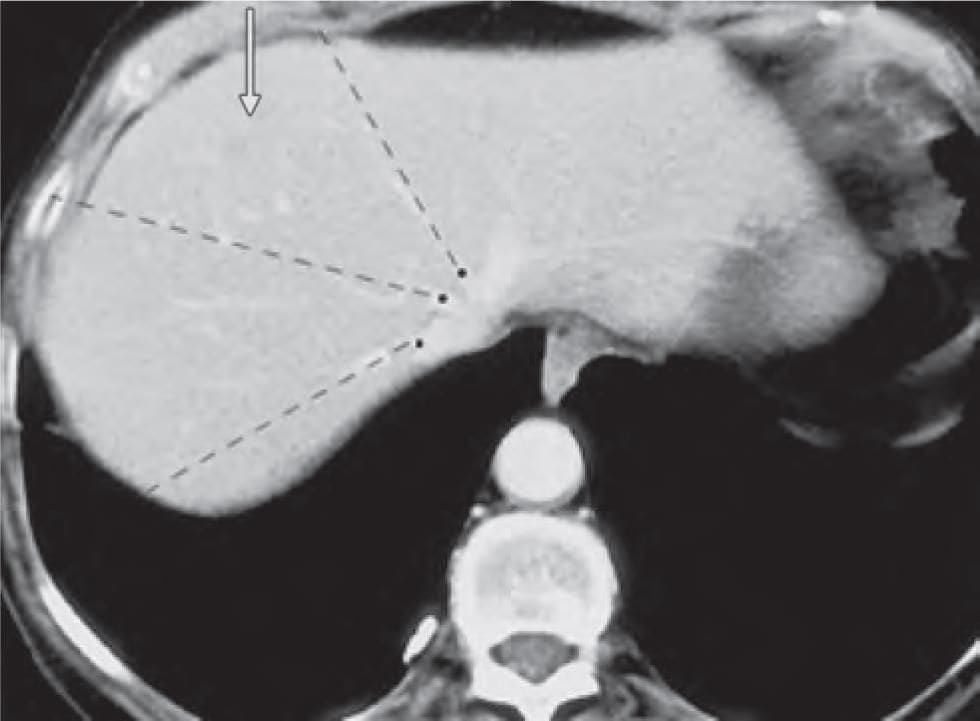
Liver is divided into eight segments according to Couinaud’s classification based upon. (AIIMS May 2019)
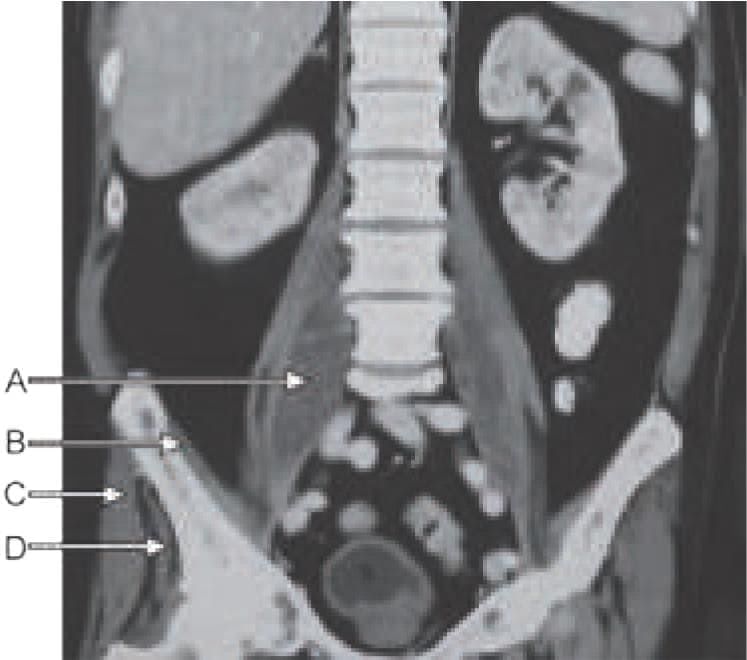
In CT scan of liver, identify the arrow marked segment: (INI-CET Nov 2022)
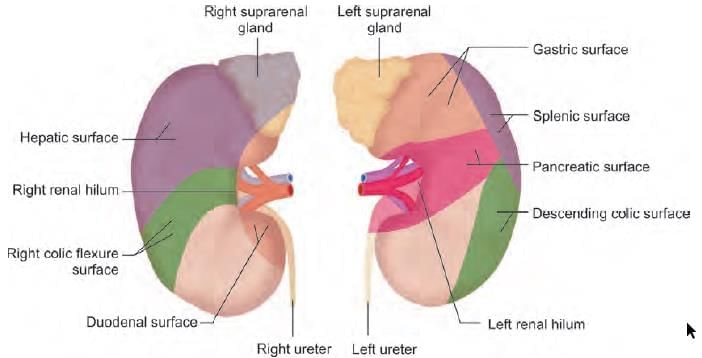
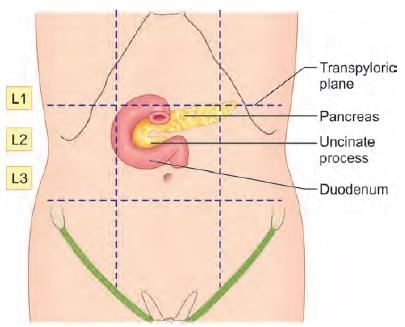
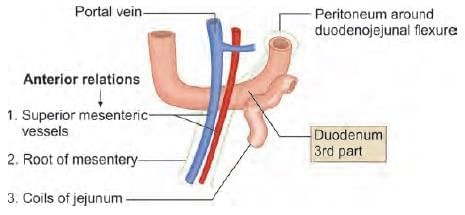
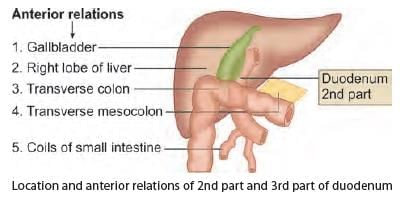
Anterior relations of third part of duodenum are all, except: (INI-CET May 2023)
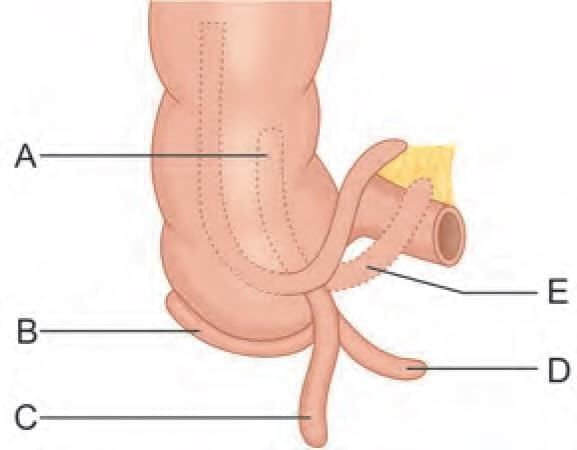
Match the location of vermiform appendix with the labelling given in the diagram: (INI-CET May 2023)
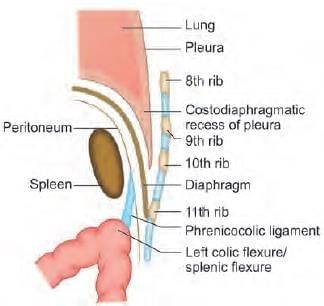
A 25-year-old male presents to emergency with left upper quadrant pain, upon examination spleen was measured to 20 cm and further extending to the mid umbilicus. The extension of the spleen to left lower quadrant was prevented by: (NEET-PG 2021)
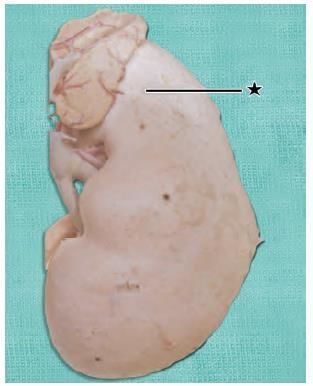
A child was brought to the hospital by his father with complaint of fever, low backache and persistent flexion of the hip joint. He had a history of Spine TB in the past. On examination child has an inguinal swelling. Identify the marked muscle responsible to be involved in this pathology: (NEET-PG 2021)