Test: Anatomy - 7 - NEET PG MCQ
25 Questions MCQ Test - Test: Anatomy - 7
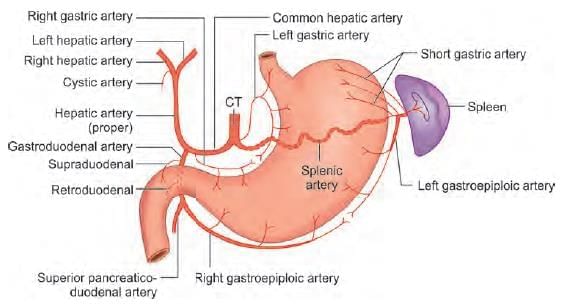
Ligation of the common hepatic artery will compromise blood flow in: (NEET-PG 2020p)
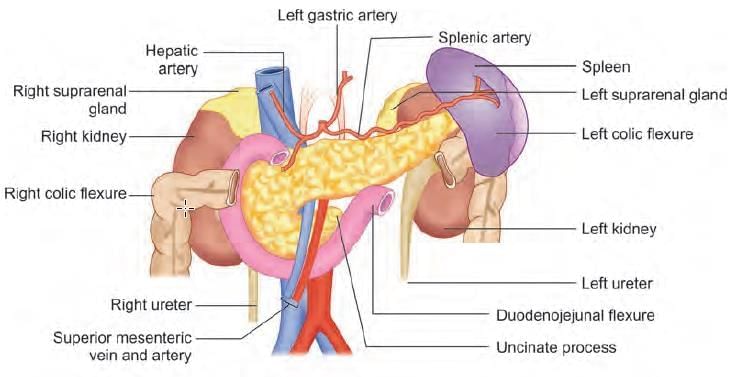
A 54-year-old man comes to a hospital with abdominal pain, jaundice, loss of appetite, and weight loss. On examination of his radiograms and CT scan, a physician finds a slowly growing tumor in the uncinate process of the pancreas. Which of the following structures is most likely compressed by this tumor? (NEET-PG 2020p)
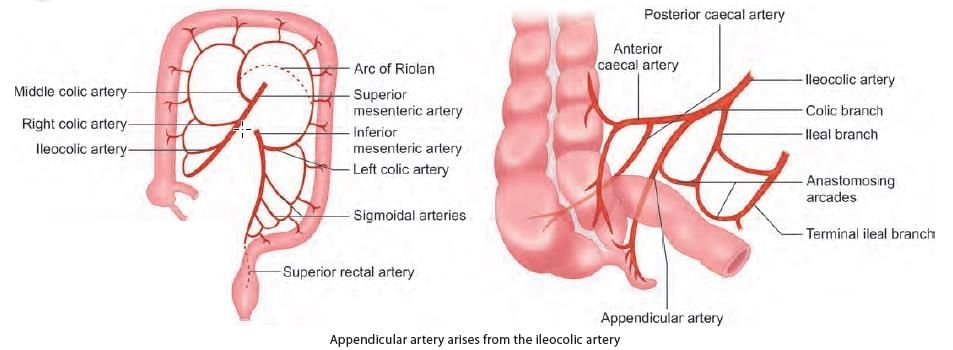
Post appendicectomy, on exploration bleeding is noticed. Ligation of which artery is beneficial? (INI-CET Nov 2022)
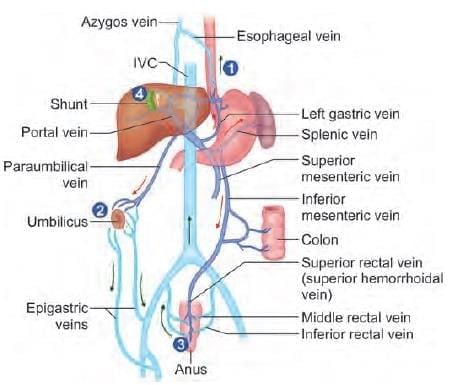
In a patient of liver cirrhosis anastomotic blood flow increases in: (NEET-PG 2023)
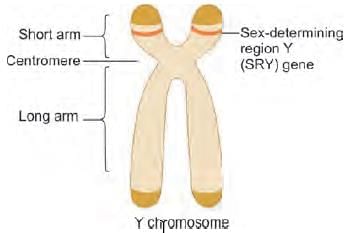
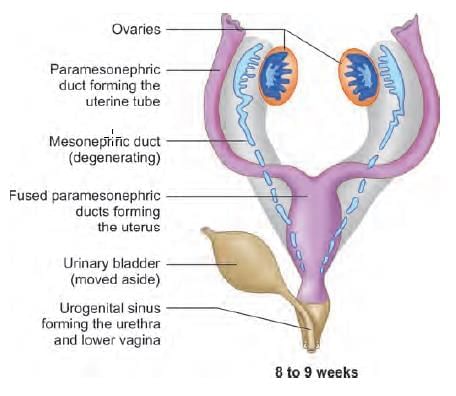
Remnants of Wolffian ducts in a female are found in: (NEET-PG 2020p)
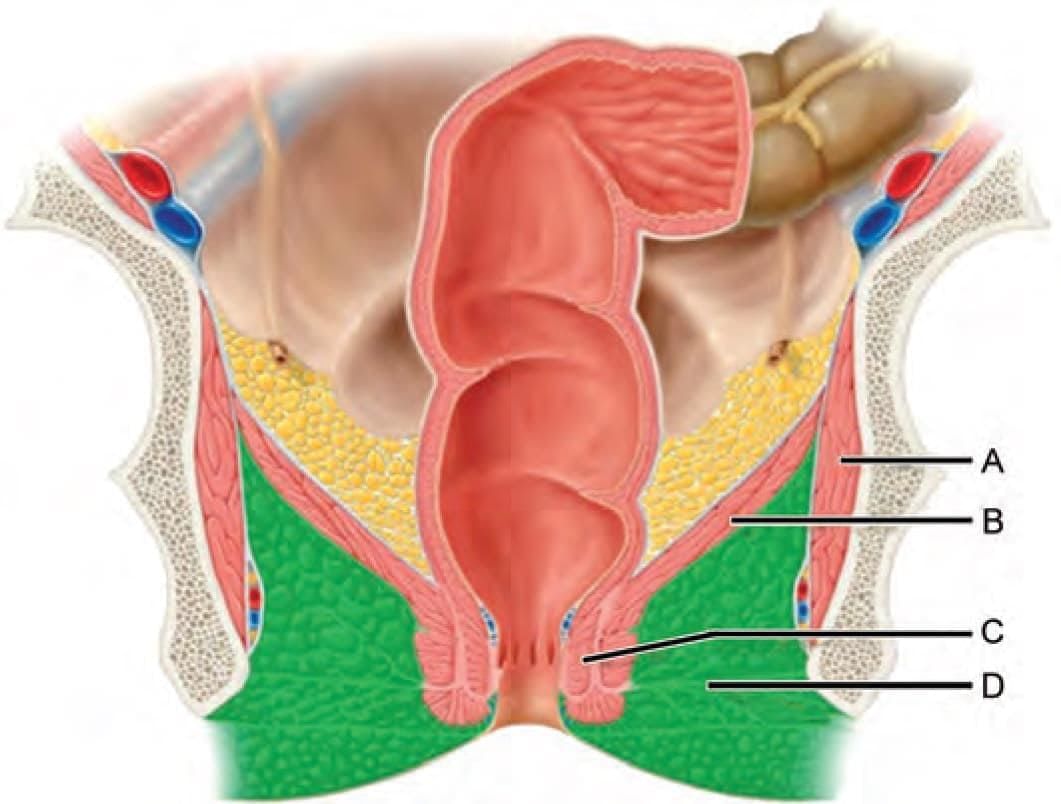
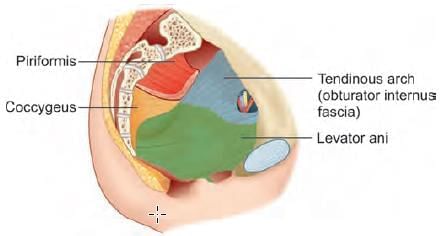
All of the following are true regarding levator ani, except: (AIIMS May 2019)
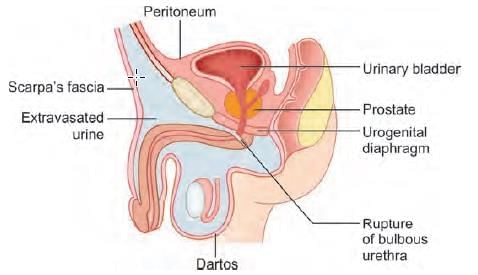
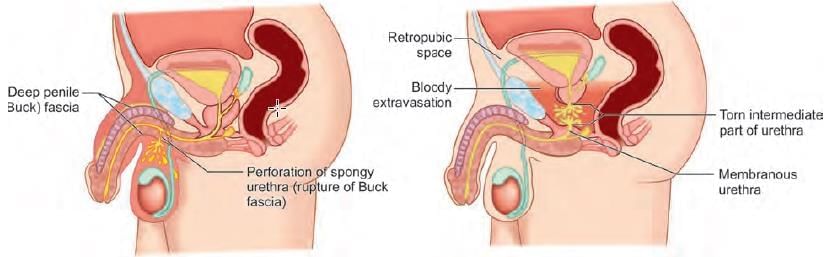
In bulbous rupture of urethra, urine extravasation occurs at all locations, except: (INI-CET Nov 2022)
A man was brought to the emergency after meeting with an accident and injured perineum. He feels an urge to micturate but is unable to pass urine. There is blood at the tip of the meatus with extensive swelling of the penis and scrotum. What is the possible site of the injury? (NEET-PG 2020p)
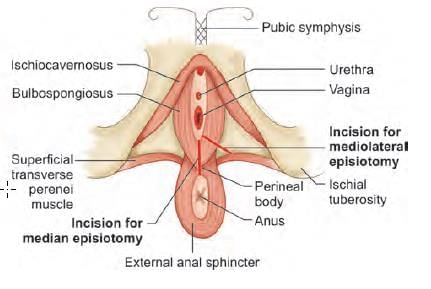
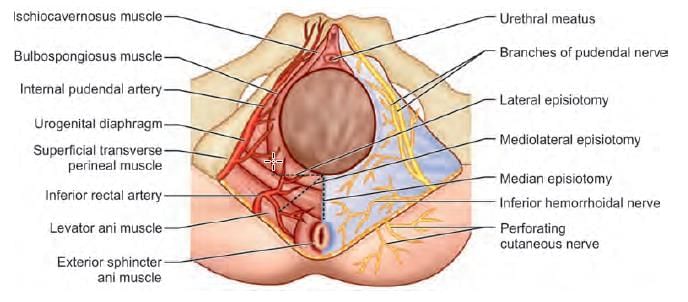
Episiotomy incision was extended posteriorly beyond perineal body injuring the structure immediately posterior to it. Which structure has been injured? (NEET-PG 2020p)
Which of the following structure is NOT cut in mediolateral episiotomy? (AIIMS June 2020)
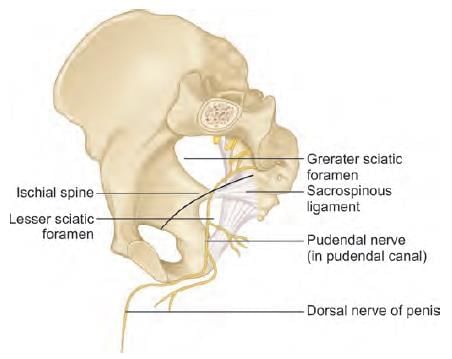
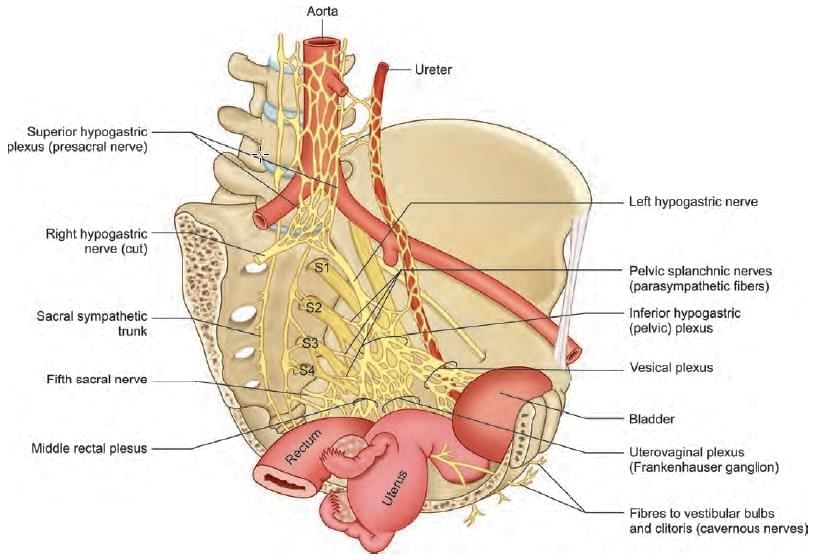
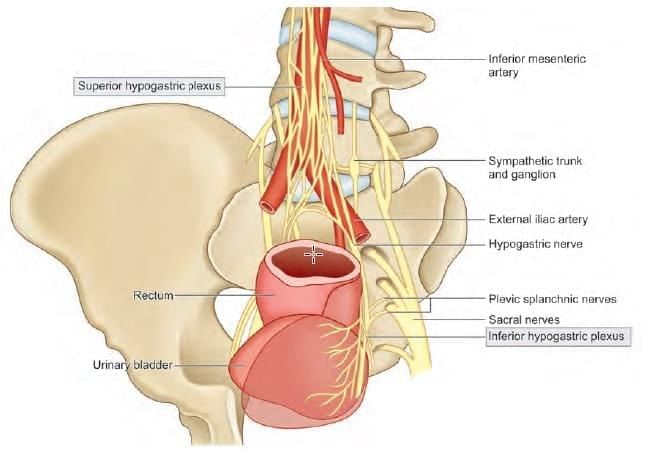
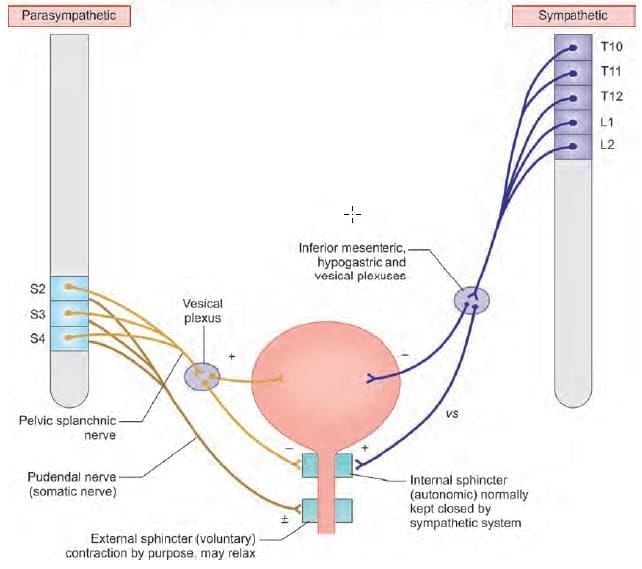
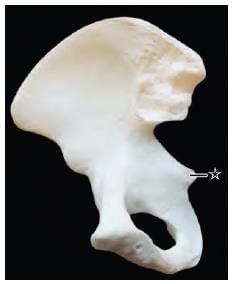
Which of the following nerves are related with the marked structure? (AIIMS Nov 2019)
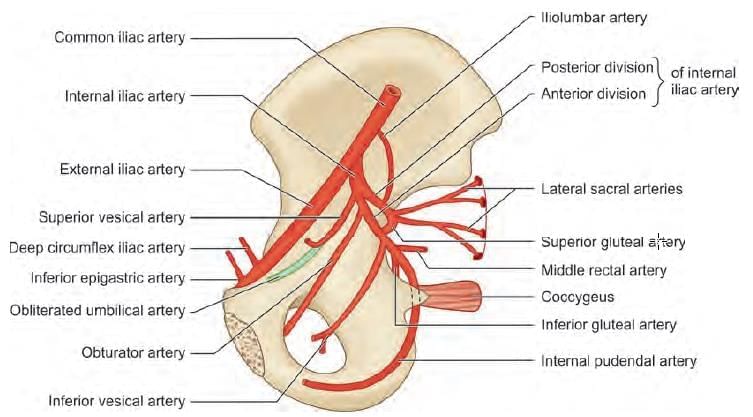
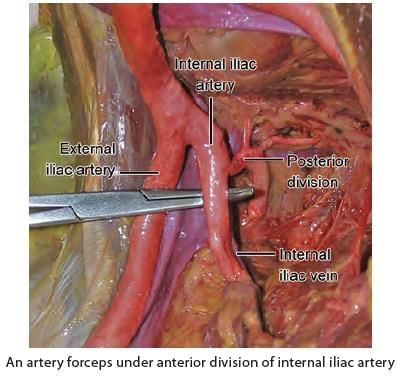
Branches from anterior division of internal iliac artery are: (INI-CET July 2021)
- Superior gluteal artery
- Inferior gluteal artery
- Superior vesical artery
- Inferior vesical artery
- Vaginal artery
- Middle rectal artery
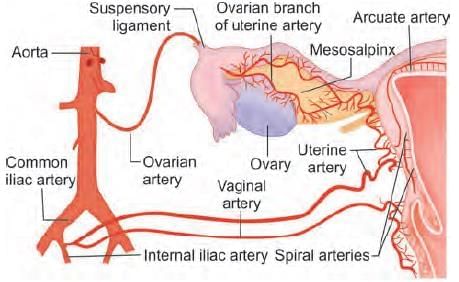
A 25 years old primigravida female after giving birth to a child have continuous bleed from uterus. The patient was taken to OT and planned for uterine devascularization. Which of the following is the correct order of devascularization? (NEET-PG 2021)
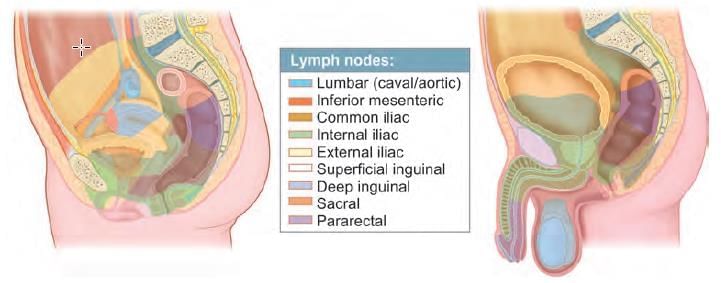
Painless cancerous lesion with inguinal lymph node involvement is due to carcinoma: (NEET-PG 2020p)
Which of the following statement is INCORRECT regarding labour pain? (INI-CET May 2022)
The most common complication of major vessel ligation in abdomino-perineal resection of carcinoma rectum is: (NEET-PG 2023)
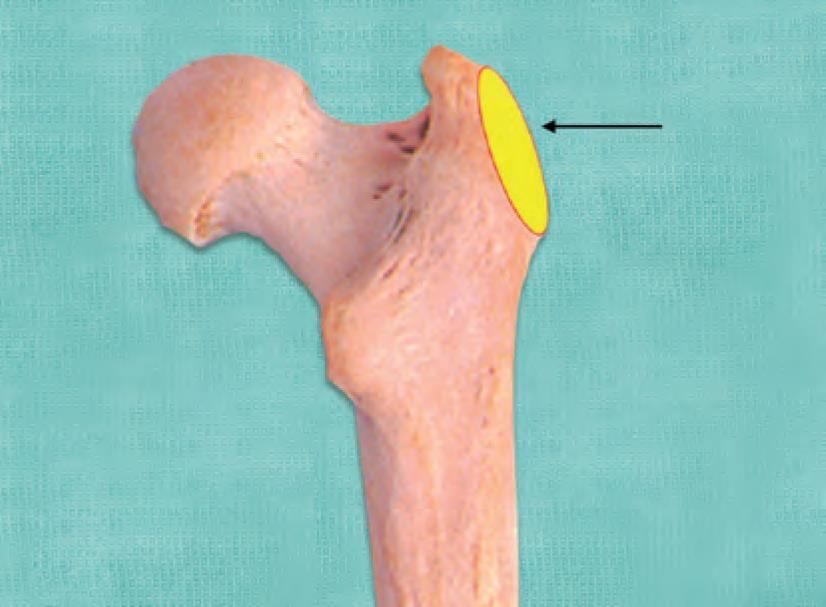
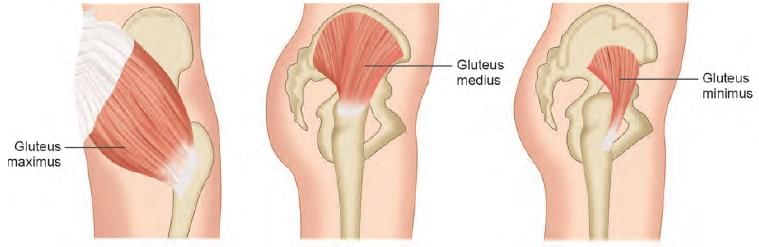
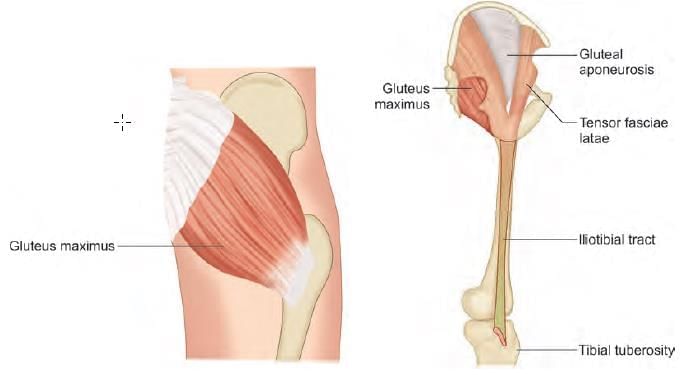
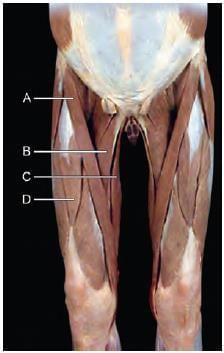
Mention the action of the muscle on hip joint as marked in the diagram below: (AIIMS June 2020)
Mention action of the muscle on hip joint, whose attachment is marked in the diagram: (INI-CET Nov 2020)
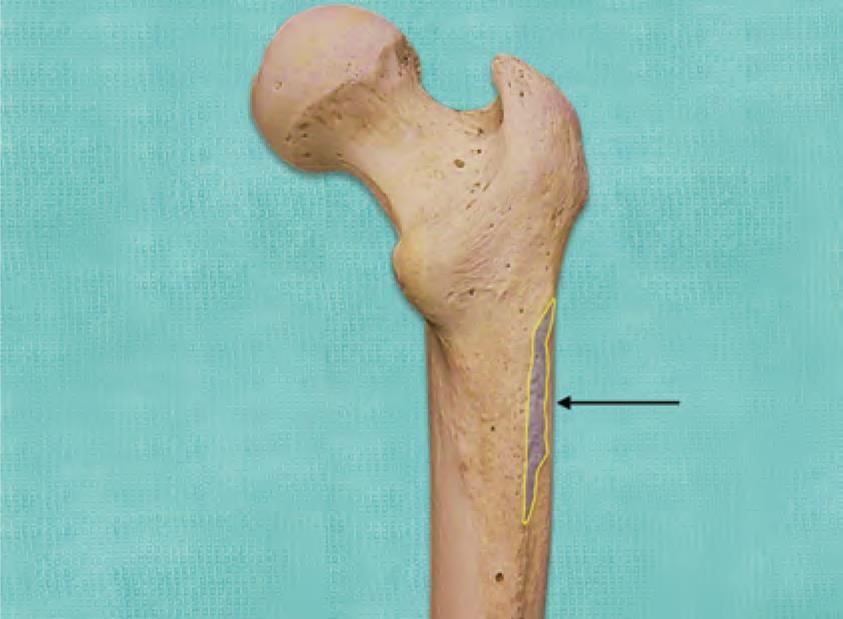
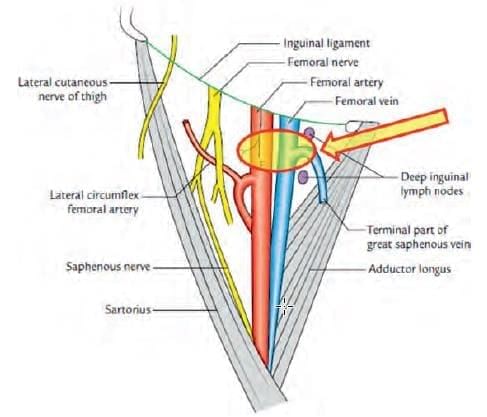
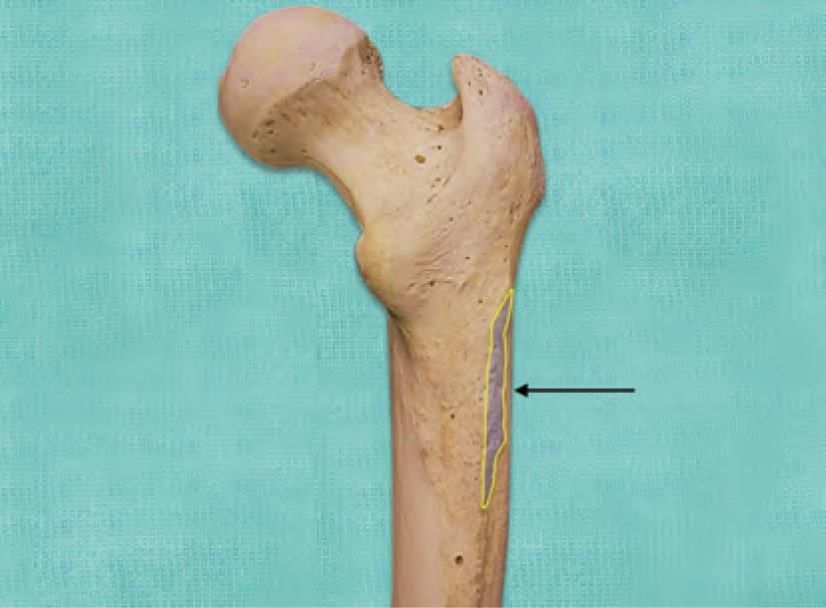
A patient with fall from a height was treated with a cast. After removal of cast he was not able to walk properly, unable to lift the leg and was dragging his right leg while walking. Which of the following marked structure is involved? (INI-CET Nov 2021)
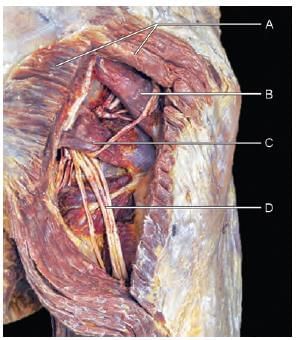
Which of the following muscle cause flexion, abduction and lateral rotation at hip joint? (INI-CET Nov 2022)
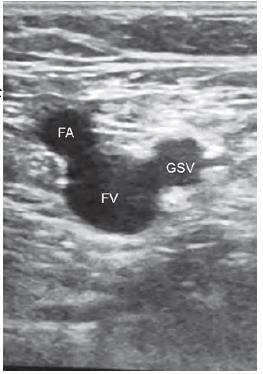
The sign seen on USG while locating the long saphenous vein and common femoral vein lying medial to the common femoral artery is called as: (NEET-PG 2020p)