Test: Congenital Heart Disease - NEET PG MCQ
25 Questions MCQ Test - Test: Congenital Heart Disease
In coarctation of aorta, site of rib notching is? (Recent Question 2015-16)
A neonate presents with anoxic spells and single S2. CXR shows all except:


Lithium use in pregnancy leads to which effect on the baby? (AIMS Nov 2018)
Which of the following is compatible with tet spells in a 4 month old child with TOF? (AIIMS May 2016)
Pulmonary blood flow increases in all except? (PGI Chandigarh May 2015)
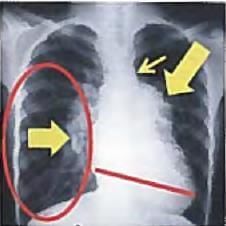
A 5-year old child with episodes of recurrent pneumonia was found to have a mid-diastolic murmur. CXR was performed. All are correct about the image shown except?

Most common cause of heart block in infants is? (Recent Pattern 2015-16)
A Preterm baby with PDA will have all except: (AIMS Nov. 2012)
Which of the following is not given it of cyanotic spell? (IS Nov. 2013)
Extremely bad prognosis is seen in which heart disease in pregnancy? (Recent Pattern 2014-15)
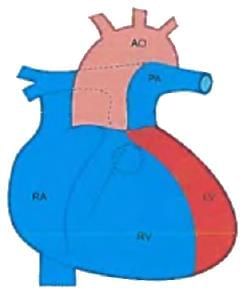
A 6-hour old child with cyanosis. On examination, S2 is loud and single. CXR was done. All arc true about this condition except?

![]()
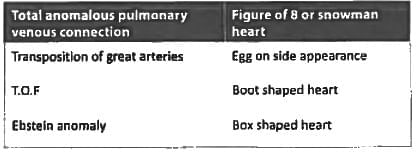
Snow man appearance or figure of 8 appearance is seen in? (Recent Question 2015-16)