Test: Epilepsy- 1 - NEET PG MCQ
20 Questions MCQ Test - Test: Epilepsy- 1
A 16-year-old girl was on anti-epileptic for treatment of focal seizure episodes while asleep. She has had no seizure for last 6 months, NCCT and EEG is normal. What is the further management? (AIIMS Nov 2018)
A man falls In front of a liquor shop and becomes unconscious. On admission he has fast pulse, feeble respiratory events and slurring of speech. He is kept in observation overnight and when he wakes up he is normal but could not recall the events of the previous night. What is the likely explanation? (AIIMS May 2017)
A 25 year old epileptic patient is on levetiracetam 1000 mg twice daily for last 2 years. He started to develop anger and aggressive behaviour as an intolerable side effect which is affecting his quality of life. What is the next step in management of the patient? (AIIMS May 2017)
A known case of GTCS is on Valproate for last 1 year. He has been seizure free for last 1 year. Recent EEG is normal. Anti-epileptics withdrawl should be initiated ___ years of initiation? (Recent Pattern Questions)
Lennox Gastaut Syndrome is characterized by? (Recent Question 2016-17)
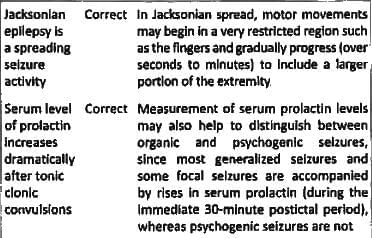
The following statement are true regarding epilepsy except: (AP PG 2015)
Patient presents with history of lip smacking and staring for 3minutes. Past history of Headache for 6 months. He was unaware of event. MRI shows a mass in temporal lobe showing hyper-intensity on T2 weighted image Diagnosis is? (JIPMER Nov 2015)
7-year old girl is easily distracted in class and exhibits poor scholastic performance. Seizures are precipitated by hyperventilation. Diagnosis is? (AIIMS May 2014)
Person suffers seizure on platform while waiting for train. He has a band showing him to be epileptic and the medicines he takes are in his pocket. So what should you do? (AIIMS Nov 14)
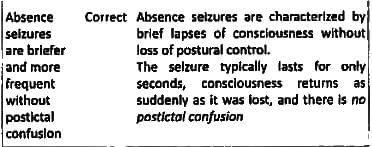
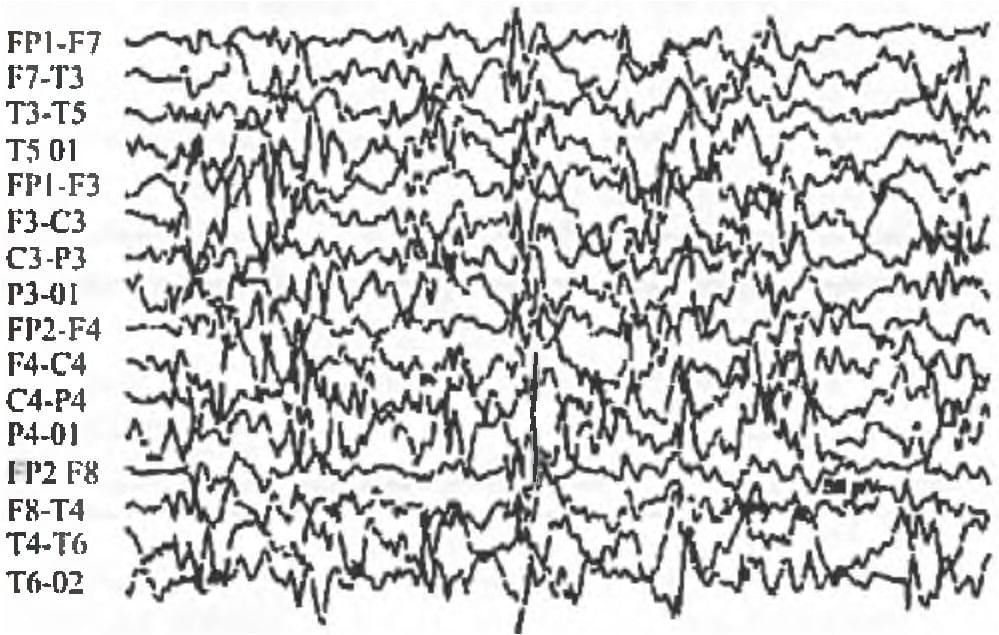
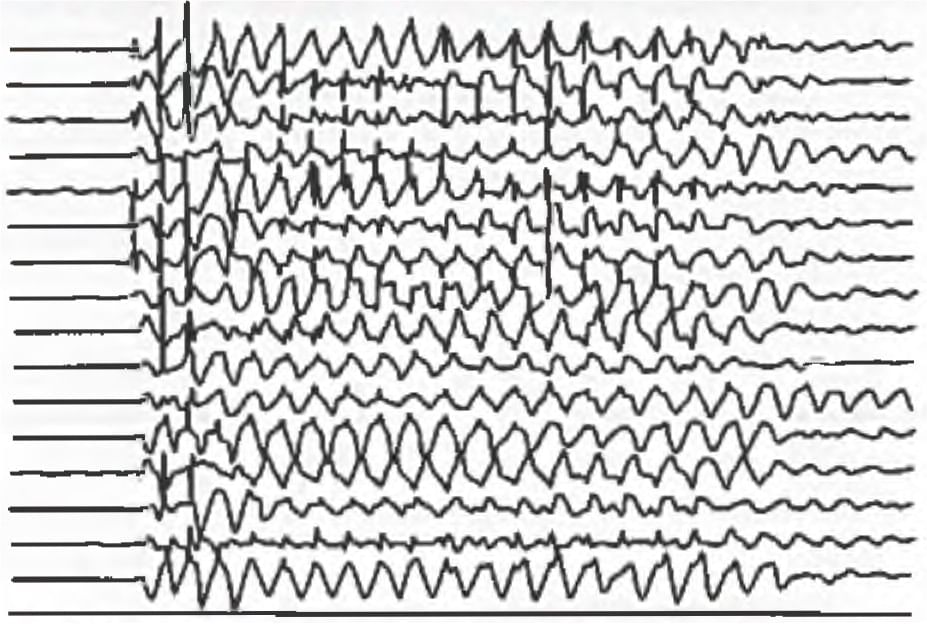
In EEG which type of waves seen in metabolic encephalopathy: (Recent Pattern 2014/15)