Test: Jaundice, Reye Syndrome, & Budd-Chiari Syndrome - NEET PG MCQ
25 Questions MCQ Test - Test: Jaundice, Reye Syndrome, & Budd-Chiari Syndrome
A patient presents with serum bilirubin values of > 40 mg % and obstructive jaundice. This indicates? (AIIMS Nov 2016)
An 8th month primigravida presented with severe pruritis. Examination revealed mild icterus, Her serum bilirubin was 3mg/dl. She has elevated AST ALT and Alkaline phosphatase. Her RFT and coagulation profile were within normal limits. She could probably be having? (AP PG 2016)
In a child surgery was done for EHBO with hepatojejunal anastomosis. Post-operatively bilirubin level after 2 weeks was 6 mg/dl from a pre-operative level 12mg/dl. The reason for this could be? (AIIMS May 2015)
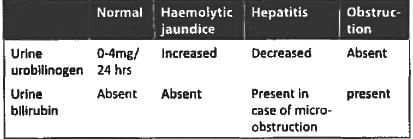
Patient presents with icterus, urine urobilinogen is absent. This indicates? (AIIMS Nov 2015)
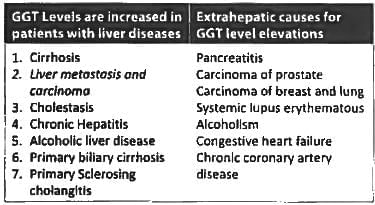
Which of the following is true regarding gamma glutamyl transferase? (JIPMER Nov 2014)
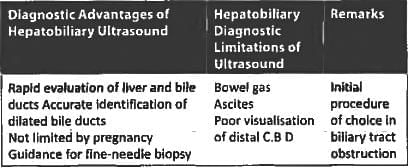
Obstructive jaundice is best detected by: (Recent Pattern 2014-15)
A defect in which of the following processes give rise to bilirubinuria? (Recent Pattern 2014-15)
Following is test marker of alcohol induced liver injury: (Recent Pattern 2014-15)
Palmar erythema is seen in: (Recent Pattern 2014-15)
Initial investigation of choice in obstructive jaundice is: (Recent Pattern 2014-15)
All of the following are true of Reye’s syndrome except: (Recent Pattern 2014-15)
Microvascular steatosis is seen in all except: (Recent Pattern 2014-15)
Micro-vesicular fatty liver in Reye's syndrome is? (AIIMS Nov 14)
The following is the least likely manifestation of acute Budd-Chiari syndrome: (Recent Pattern 2014-15)
A patient presenting with jaundice is found to have 20 mg % of bilirubin, of which 9.3 is direct reacting & 85 U/L of alkaline phosphatase, the likely diagnosis is: (Recent Pattern 2014-15)
In Budd-Chiari syndrome there is obstruction to: (Recent Pattern 2014-15)