Test: Nephrotic Syndrome & Nephritic Syndrome and Hematuria - NEET PG MCQ
30 Questions MCQ Test - Test: Nephrotic Syndrome & Nephritic Syndrome and Hematuria
Most common nephropathy associated with malignancy? (AIIMS May 2015)
A 10-year-old child presents with oedema and decreased urine output. On evaluation, serum albumin is 2.5 g/dL, S. Creatinine is 0.5 mg/dl, Urine protein is 3+ with no RBC casts, Pathological change expected is? (AIIMS May 2015)
All are true about most common cause of nephrotic syndrome in children except? (Recent Question 2015-16)
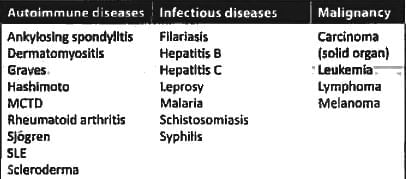
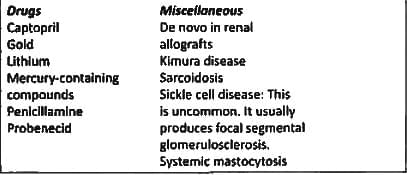
Membranous Glomerulopathy is seen in?
All are seen in Nephrotic syndrome except: (Recent Question 2015-16)
Type of glomerulopathy in HIV positive patient is: (Recent Question 2015-16)
Nephrotic syndrome patient after a bout of diarrhea presented with acute kidney injury and serum creatinine 4.5. All are possible reasons except? (AIIMS Nov 14)
Leprosy causes: (Recent Pattern 2014-15)
Non-selective proteinuria is seen in: (Recent Pattern 2014-15)
Membranous GN with reduced complement level is seen in? (Recent Pattern 2014-15)
Regarding complications of nephrotic syndrome incorrect is: (Recent Pattern 2014-15)
Renal vein thrombosis is associated with which underlying disease of kidney: (Recent Pattern 2014-15)
All of the following are decreased in Nephrotic syndrome except (Recent Pattern 2014-15)
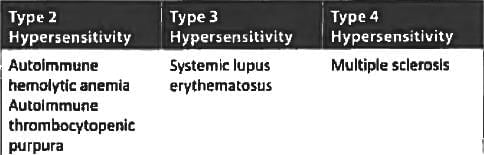
Which of the following immunological reactions occurs in Good-pasture syndrome? (UPSC 2015)
Chronic reflux nephropathy causes: (Recent Pattern 2014-15)
Henoch schonlein purpura is characterized by the following except: (APPG 2015 Medicine)
True statement regarding post streptococcal glomerulonephritis is? (JIPMER Nov 2014)
True statement regarding post streptococcal glomerulonephritis is? (JIPMER Nov 2014)
Feature of RPGN are A/E: (Recent Pattern 2014-15)
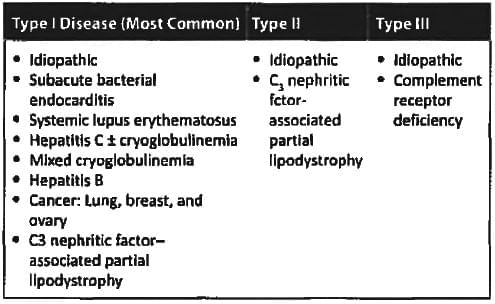
Type I membrano proliferative Glomerulo-nephritis is commonly associated with all except; (Recent Pattern 2014-15)
Characteristic finding in AGN;
RBC cast in the microscopic examination of the urine is an indicator of: (Recent Pattern 2014-15)
What is the minimum number of red blood cells per microliter of urine required for diagnosis of hematuria? (APPG2014)
Essential feature of nephritic syndrome is: (Recent Pattern 2014-15)
Manifestation of acute glomerulonephritis includes each of the following except: (Recent Pattern 2014-15)
A female patient presents with upper respiratory tract infection. Two days after, she develops hematuria. Probable diagnosis: (Recent Pattern 2014-15)
Triad of glomerulonephritis pulmonary hemorrhages and antibody to basement membrane is called: (Recent Pattern 2014-15)