Test: Spirometry, DLco, Alveolar-Arteriolar Gradient & Types of Respiratory Failure- 2 - NEET PG MCQ
15 Questions MCQ Test - Test: Spirometry, DLco, Alveolar-Arteriolar Gradient & Types of Respiratory Failure- 2
A 17-year-old boy presents with complaints of difficulty in breathing. There was venous congestion of face and neck. A clinical diagnosis of SVC syndrome was made. The X-ray showed mediastinal widening. What is the next step?
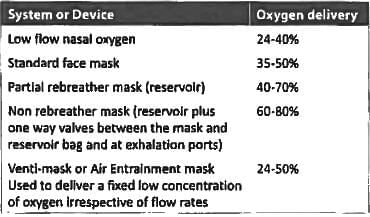
Maximum oxygen concentration can be delivered by? (AIIMS Nov 2017)
Which of the following is not an etiology for peripheral cyanosis? (Recent Pattern Questions)
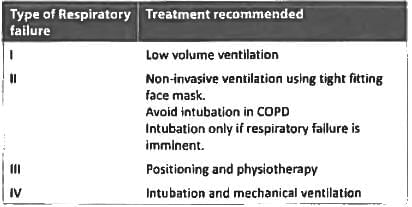
A 55 year old female with morbid obesity presents to the ER with increased breathlessness, cough and orthopnea for 2 days. She has pulse rate of 96/minute, BP = 136/90 mmHg, RR = 30/min and spO₂ = 76%. ABG report shows pO₂ = 76 mm Hg, PCO₂ = 24 mmHg and pH = 7.28, The next step is? (AIIMS May 2016)
Which is the best treatment of type 4 Respiratory failure? (Recent Question 2016-17)
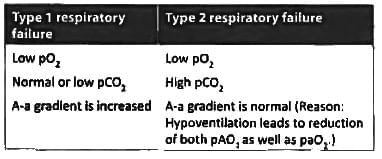
In type II respiratory failure there is: (Recent Pattern 2014-15)
All of the following are true about type I respiratory failure except: (Recent Pattern 2014-15)