Test: ABO System, Blood Transfusions and Blood Components - NEET PG MCQ
30 Questions MCQ Test - Test: ABO System, Blood Transfusions and Blood Components
A patient on warfarin presents with major bleeding and is found to have INR of 15. How much fresh frozen plasma (FFP) is required to treat this situation? (JIPMER May 2018)
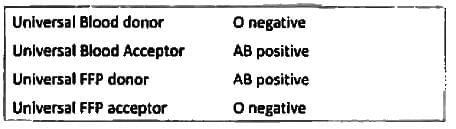
A trauma patient presents at emergency department. There is no time for cross matching. FFP of which group can be transfused safely? (AIIMS Nov 2018)
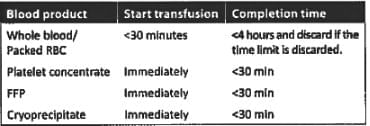
Following an RTA, A young man is brought into ER. Due to massive blood loss, 2 units of PRBC and 4 units of platelet concentrate is obtained from blood bank. Only one IV line is accessible. What will you do? (AIIMS Nov 2018)
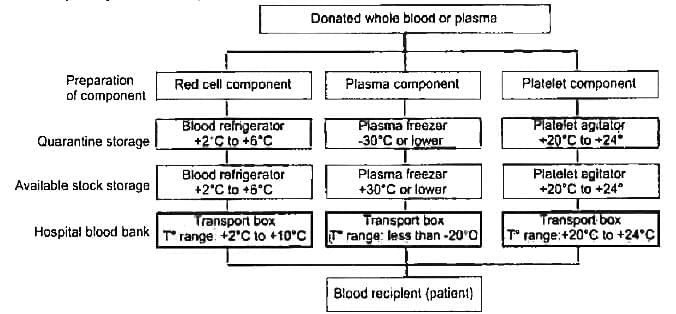
Which of the following is correct about storage temperature of RBC, Platelets and FFP? (AIIMS May 2018)
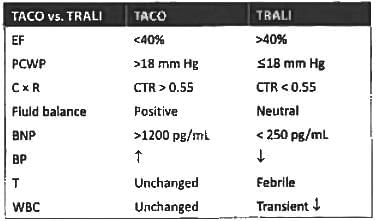
A patient in ICU was given blood transfusion. 3 hours later SpO₂ is reduced to 75% with respiratory difficulty. CVP is 15 cm water and PCWP is 25 mm Hg. CXR is shown below. What is the diagnosis? (Recent Pattern 2018)

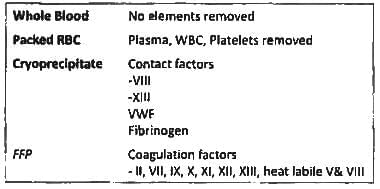
Which of the following is correct about Packed RBC transfusion? (AIIMS May 2016)
The storage temperature of RBC in blood bank is? (AIIMS May 2016)
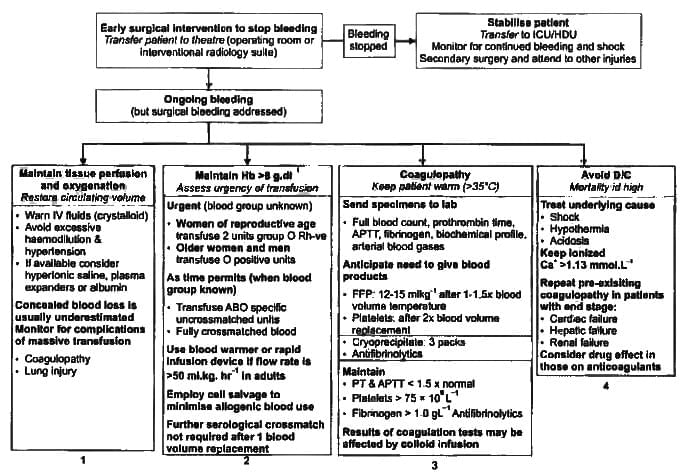
The following are major complications of massive transfusion except? (APPG 2016)
Which blood product is best to be given in multiple clotting factor deficiency and active bleeding? (AIIMS May 2015)
Carbohydrate related to blood grouping? (JIPMER Nov 2015)
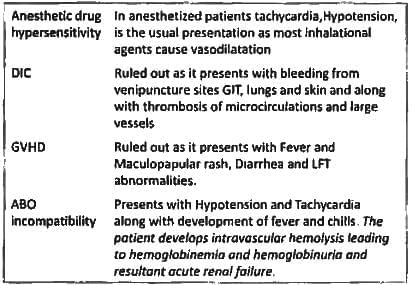
A 30 years old male was given blood transfusion in the O.T. following which he develops tachycardia hypotension BP-70/40 mm of Hg and hematuria within 10 minutes of starting the transfusion. The most probable cause is? (JIPMER Nov 2014)
Cryoprecipitate does not contain? (Recent Pattern 2014-15)
Which one of the following is the cause of non-cardiogenic pulmonary oedema seen in immunologic blood transfusion reaction: (Recent Pattern 2014-15)
Complication of blood transfusion can be all except: (Recent Pattern 2014-15)
Most common complication of blood transfusion: (Recent Pattern 2014-15)
Hypochromic microcytic anemia is seen in all, except: (Recent Pattern 2014-15)
There are more than 400 blood groups, we consider only ABO blood group, because: (Recent Pattern 2014-15)