Test: Arrhythmias and Emergency Medicine- 2 - NEET PG MCQ
20 Questions MCQ Test - Test: Arrhythmias and Emergency Medicine- 2
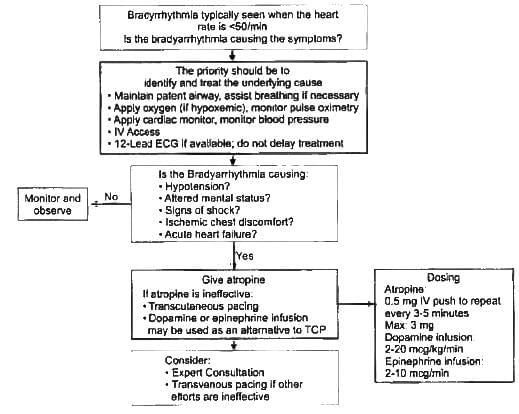
Which of the following is recommended for management of symptomatic bradycardia non responsive to 0.5mg iv atropine? (Recent Pattern Questions)
A 50-year-old patient presents with features of poor perfusion following MI. On examination heart rate is 40/min with BP of 60mmHg systolic. Atropine was given twice over 5 minutes, but the condition of patient is not improving. What is the next best step? (Recent Pattern Questions)
Which drugs are involved in bradycardia algorithm? (Recent Pattern Questions)
After determination of inadequate perfusion of organs in a patient with bradycardia, which of the following is the first step? (Recent Pattern Questions)

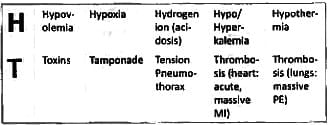
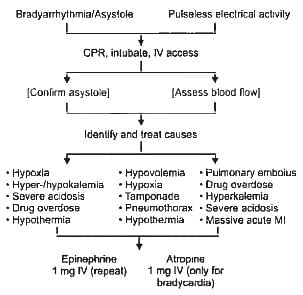
Which of the following is not a cause of PEA? (Recent Pattern Questions)
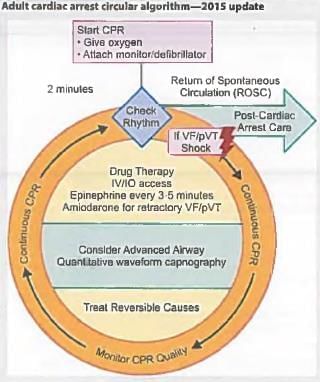
Which of the following drugs is used first line in management of PEA? (Recent Pattern Questions)
What is the cause of death in Commotio cordis? (Recent Pattern Questions)
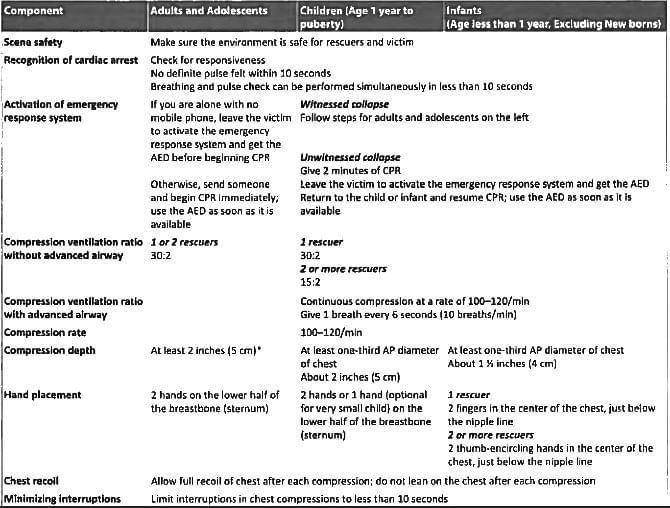
An unresponsive patient is brought to the emergency department with no proper history. What will be your next step? (AIIMS Nov 2016)
The ratio of chest compression to rescue breath ratio for a lone rescuer in CPR for all ages is? (AIIMS Nov 2016)
Which of the following statements is true about atropine and its role in cardiac arrest protocol? (Recent Question 2016-17)
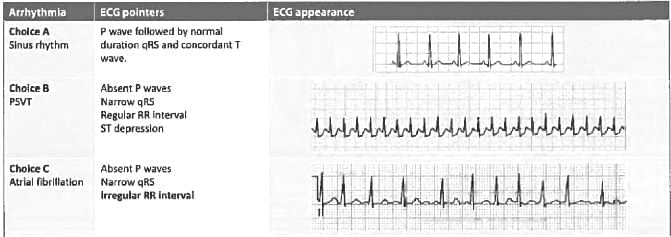
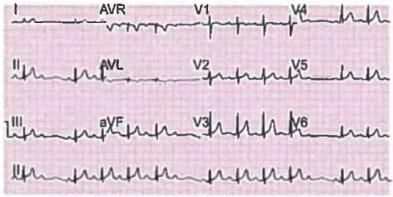
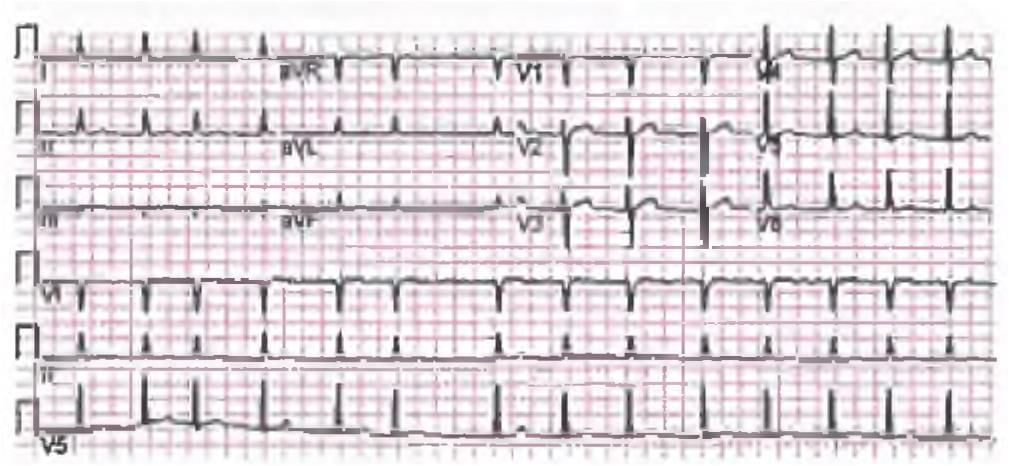
A 30-year-old man presents with recurrent attacks of feeling dizzy. ECG was done. What is the diagnosis? (Recent Question 2016-17)
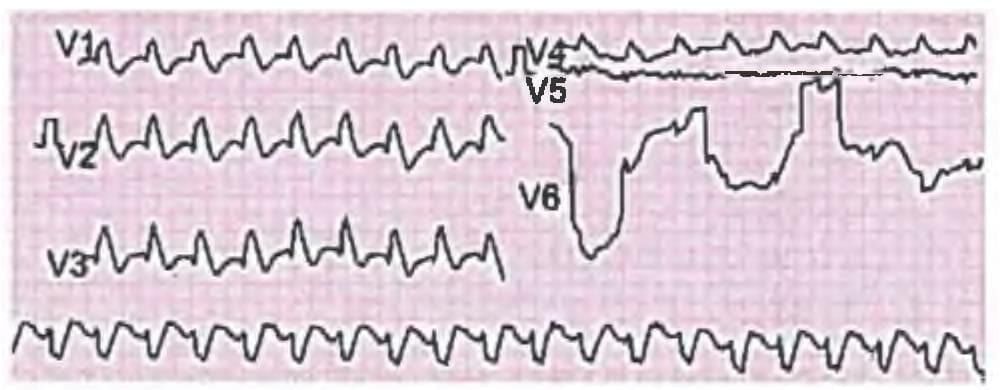
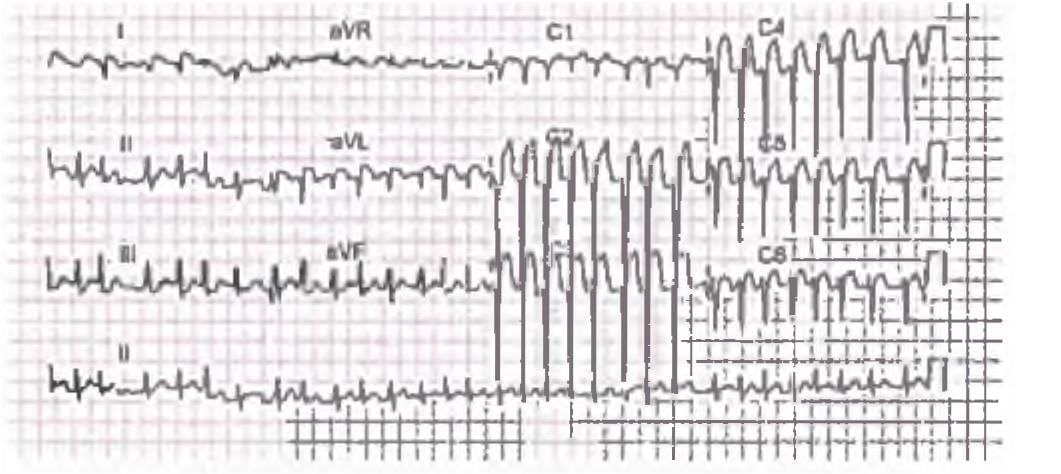
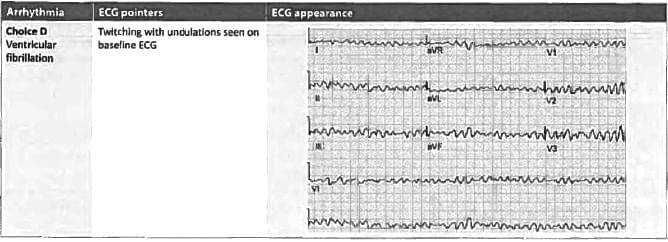
Identify the ECG given in the figure below? (AIIMS Nov 15)
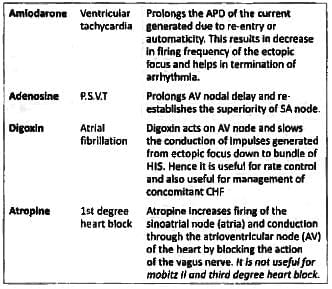
Match List I with List II and select the correct answer using the code given below the lists: (UPSC 2015)
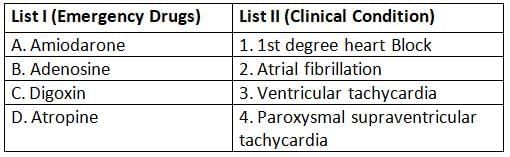
Codes:
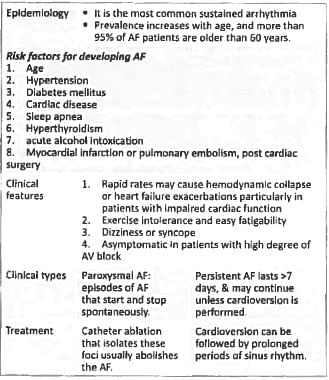
Which of the auscultatory sign is absent in mitral stenosis in the presence of atrial fibrillation? (UPSC 2015)
What is the drug of choice to control sudden onset supraventricular tachycardia? (Bihar PG 15)