Test: Hemodialysis & Kidney Transplantation - NEET PG MCQ
30 Questions MCQ Test - Test: Hemodialysis & Kidney Transplantation
Which of the following is an absolute indication for hemodialysis? (Recent Question 2015-16)
Which of the following Microorganism is incriminated in infection after Hemodialysis? (Recent Question 2015-16)
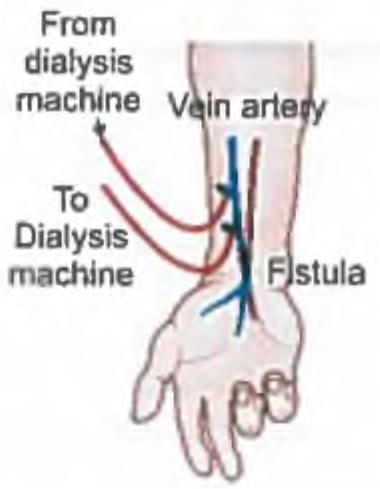
Hemodialysis can be performed for long periods from the same site because? (Recent Question 2015-16)
Chronic hemodialysis in ESRD patient is done: (Recent Question 2015-16)
A patient of ESRD is undergoing hemodialysis. Central dialysis catheter is placed at which site?

The patient is scheduled for haemodialysis. The A-V fistula is known as? (Recent Question 2015-16)
The following are the complications of haemodialysis except: (Recent Pattern 2014-15)
Most common acute complication of dialysis is: (Recent Pattern 2014-15)
Amyloidosis protein associated with hemodialysis? (Recent Pattern 2014-15)
The absolute indications for dialysis include the following except: (Recent Pattern 2014-15)
All of the following uremic manifestations improve with dialysis except: (Recent Pattern 2014-15)
Following are absolute indication for hemo-dialysis except: (Recent Pattern 2014-15)
Post kidney transplantation a patient presents with diarrhoea. The motility of the worms is shown in the figure. Correct statement about the organism is? (AIIMS Nov 2018)

Which is the best test for detection of recent CMV infection?
Nephrotic syndrome associated with malaria is due to infection of? (Recent Pattern 2014-15)
The most common ocular infection after renal transplantation is by: (Recent Pattern 2014-15)
Category 4 donation after cardiac death (DCD) is defined as? (Recent Question 2016-17)
Most common cancer after kidney transplantation? (Recent Pattern 2014-15)
Life expectancy after living donor kidney transplantation is ? (Recent Question 2016-17)
Select the FALSE statement regarding Kidney Transplantation? (APPG 2016)
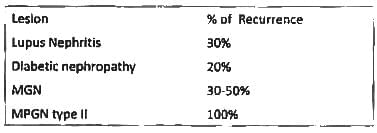
A renal transplant recurrence of the disease occurs mostly with: (Recent Pattern 2014-15)
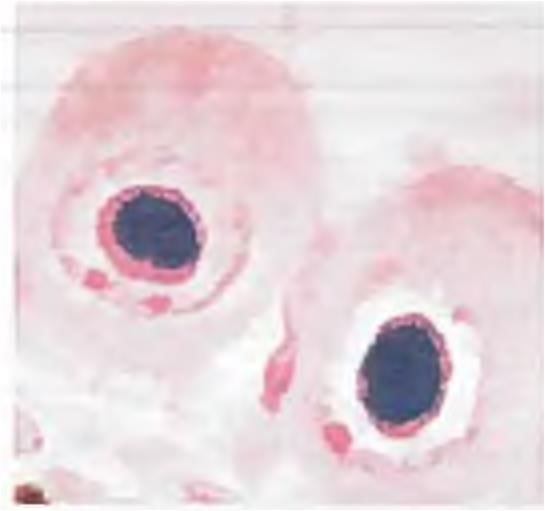
True about Light microscopic changes in Minimal Change Glo m erulonephritis is: (AI 95)
A 7-year-old boy presented with generalized edema. Urine examination revealed marked albuminuria. Serum biochemical examinations showed hypoalbuminaemia with hyperlipidemia. Kidney biopsy was undertaken. On light microscopic examination, the kidney appeared normal. Electron microscopic examination is most likely to reveal (Recent Pattern 2014-15) (AIIMS Nov-03)