Test: PUD and ZES - NEET PG MCQ
30 Questions MCQ Test - Test: PUD and ZES
Which is the best investigation for Metastatic Gastrinoma? (Recent Question 2016-17)
What is the treatment of choice for Menetrier's disease? (Recent Question 2016-17)
Which of the following features are related to Zollinger Ellison syndrome?
A. Aggressive and refractory peptic ulceration
B. Unregulated gastrin release
C. Bela islet cell tumor of pancreas
D. Diarrhea present in uplo 50% cases
Select the correct answer using the code given below: (UPSC 2015)
A. Aggressive and refractory peptic ulceration
B. Unregulated gastrin release
C. Bela islet cell tumor of pancreas
D. Diarrhea present in uplo 50% cases
Select the correct answer using the code given below: (UPSC 2015)
Consider the following statements with regard lo duodenal ulcers?
a. They occur most often in the second part of duodenum.
b. Infection with H. pylori and NSAID-induced injury account for the majority of duodenal ulcers.
c. Malignant duodenal ulcers are extremely rare.
d. Eradication of H. pylori has greatly reduced the recurrence rates in duodenal ulcers.
Which of the above statements is/are correct? (UPSC 2015)
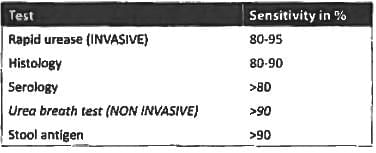
Most sensitive test for diagnosis of H pylori? (JIPMER Nov 2014)
Bleeding from lesser curvature in gastric ulcer, source of bleeding is? (JIPMER 2014)
Helicobacter pylori is associated with following except: (Recent Pattern 2014-15)
Eradication of infection by anti-H. pylori antibiotics is best determined by (Recent Pattern 2014-15)
A 60 year old male had a sudden fall in the toilet, his BP was 90/60 mm Hg and pulse was 100 per minute. His relatives reported that his stool was black/dark in color. Further careful history revealed that he is a known case of hypertension and coronary artery disease and was regularly taking aspirin, atenolol and sorbitrate. The most likely diagnosis is? (AIMS May 2012)
A 70-year-old male patient presented to the emergency department with pain in epigastrium and difficulty in breathing for 6 hours. On examination, his heart rate was 56 per minute and the blood pressure was 106/60 mm Hg. Chest examination was normal. The patient has been taking omeprazole for gastroesophageal reflux disease for last 6 months. What should be the initial investigation: (Recent Pattern 2014-15)
Which drug is not effective against H. pylori? (Recent Pattern 2014-15)
All of the following are indications for surgery in a case of duodenal ulcer except: (Recent Pattern 2014-15)
True about dumping syndrome is all except: (Recent Pattern 2014-15)
Which of the following statements about peptic ulcer disease is true? (Recent Pattern 2014-15)
Consider the following feature with reference to Zollinger Ellison syndrome:
- Intractable peptic ulceration
- Secretory diarrhea
- Most common site is pancreas
Which of these features are present in Zollinger-Ellison Syndrome (Recent Pattern 2014-15)
All of the following are true regarding a patient with acid peptic disease except: (Recent Pattern 2014-15)
Disabling paraumbilical pain within 10 minutes of eating food with history of weight loss. Past history is positive for Myocardial infarction in last year indicates. (New pattern)
The most common complication of vagotomy is: (Recent Pattern 2014-15)
MC age of presentation of gastric ulcer is: (Recent Pattern 2014-15)
Which of the following have hypergastrinemia with decrease acid output? (Recent Pattern 2014-15)
Which one of the following is best for localization of Zollinger Ellison syndrome? (Recent Pattern 2014-15)
Not true in type A fundal gastritis is: (Recent Pattern 2014-15)
Dumping syndrome is due to all except: (Recent Pattern 2014-15)