Test: Raised ICP- 2 - NEET PG MCQ
25 Questions MCQ Test - Test: Raised ICP- 2
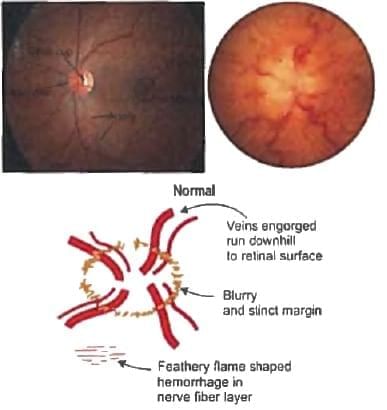
Increased intra-cranial tension is related to: (Recent Question 2015-16)
A road traffic accident patient in the casualty is comatose with unilaterally dilated pupil. The NCCT of the patient shows a Lesion peripherally present with concavo - convex border. What is the probable diagnosis? (Recent Question 2015-16)
Extradural hemorrhage on NCCT Head is seen as: (Recent Question 2015-16)
Which of the following is a sign of brainstem death? (AIIMS Nov 2012)
A 65 yr old male fainted in the bathroom. His relatives informed that his stool was black in colour. He is hypertensive and has got history of coronary artery disease. He was on long term treatment with atenolol, aspirin and sorbitrate. His BP = 80/50 and HR 150/min. Most probable diagnosis: (AIIMS May 2011)
In Glasgow coma scale, withdrawal to pain comes under which score? (AIMS Nov 2012)
DOC for idiopathic intra-cranial hypertension: (I.I.H) (Recent Pattern 2014/15)
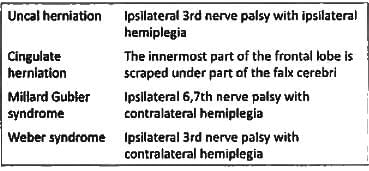
Ipsilateral 3rd nerve palsy with ipsilateral hemiplegia is seen with: (Recent Pattern 2014/15)
Pseudo-Tumour Cerebri is caused by all except: (Recent Pattern 2014/15)
You are a doctor in C.H.C. when a patient of acute head injury comes with worsening of GCS leading to coma. Patient has unilateral dilatation of pupil and hemiplegia. You decide to do burr hole at? (AIIMS Nov 2014)
Dilated ventricles with normal CSF pressure is seen in: (Recent Pattern 2014/15)