Test: Anatomy - 2 - NEET PG MCQ
25 Questions MCQ Test - Test: Anatomy - 2
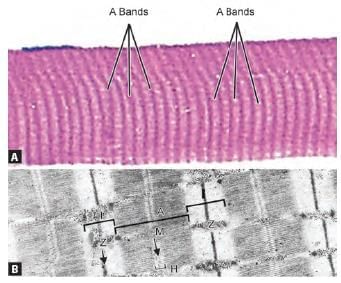
Arrange the parts of sarcomere from periphery to centre: (INI-CET May 2023)
1. Z line
2. A band
3. M line
4. H zone
1. Z line
2. A band
3. M line
4. H zone
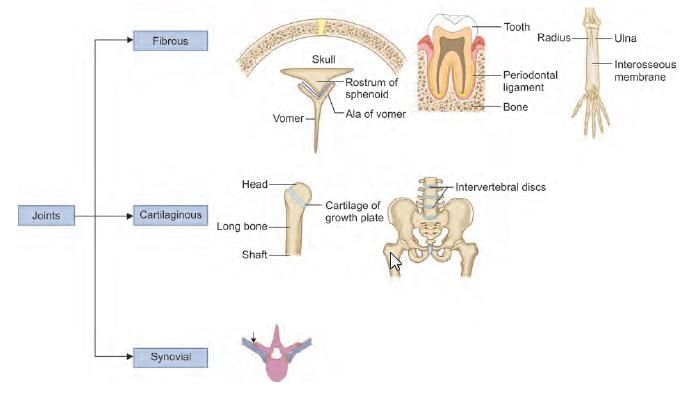
Type of joint present at middle radio-ulnar joint: (INI-CET Nov 2020)
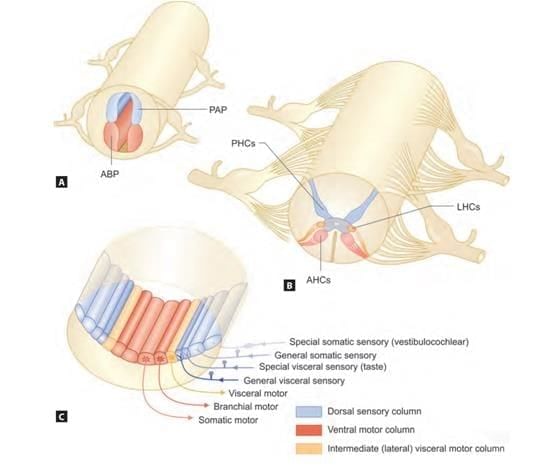
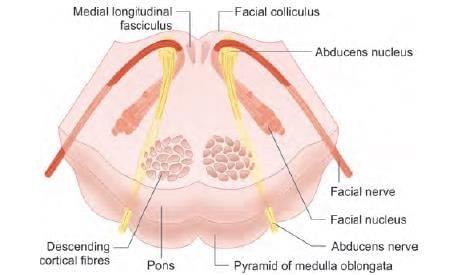
Arrange the following neural columns from medial to lateral at the floor of 4th ventricle:
1. General somatic afferent
2. General visceral afferent
3. Special visceral afferent
4. Special somatic afferent
1. General somatic afferent
2. General visceral afferent
3. Special visceral afferent
4. Special somatic afferent
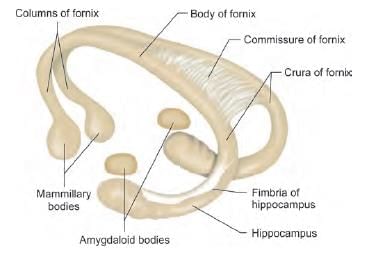
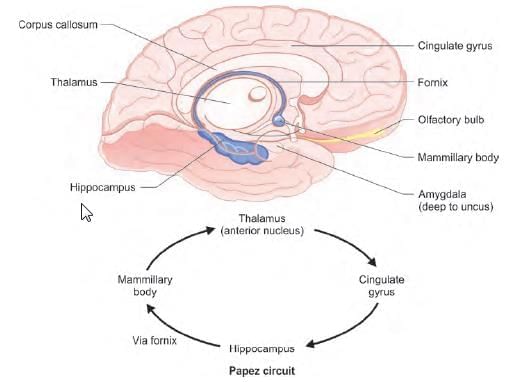
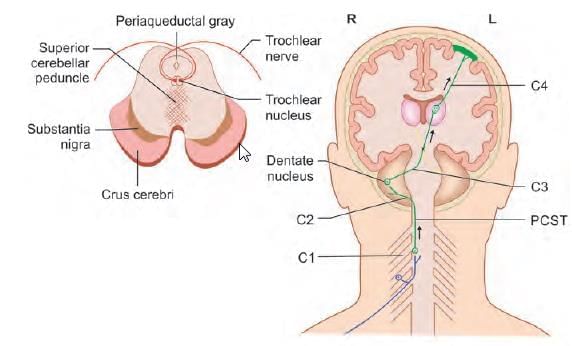
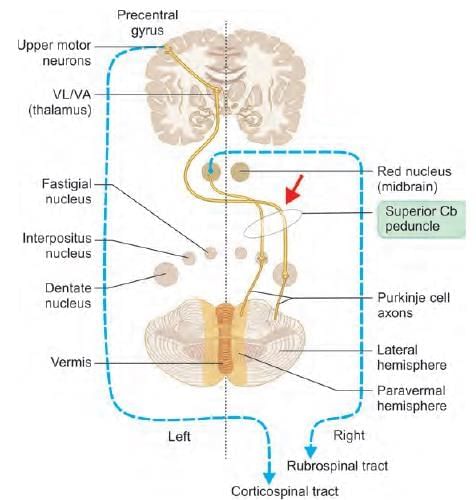
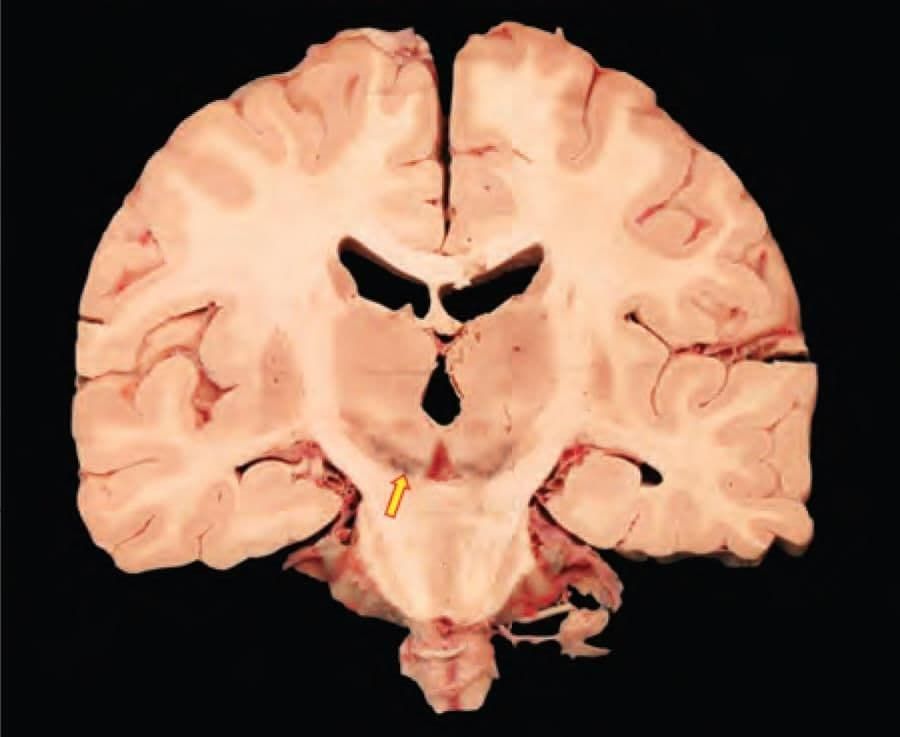
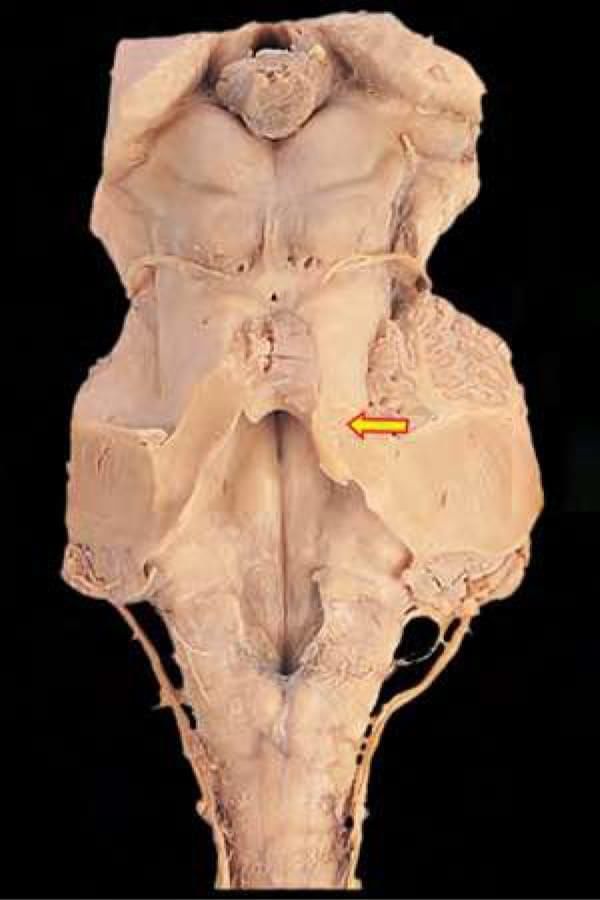
Fibres from the arrow marked structure in the following diagram, reach which nucleus of thalamus? (INI-CET Nov 2021)

Which of the following are components of limbic system? (INI-CET Nov 2022)
1. Thalamus
2. Subthalamus
3. Amygdala
4. Hippocampus
5. Hypothalamus
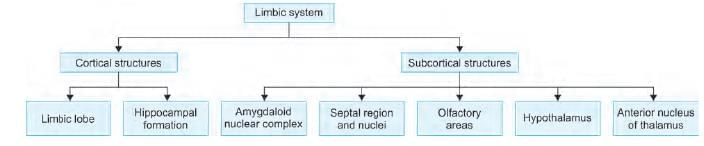
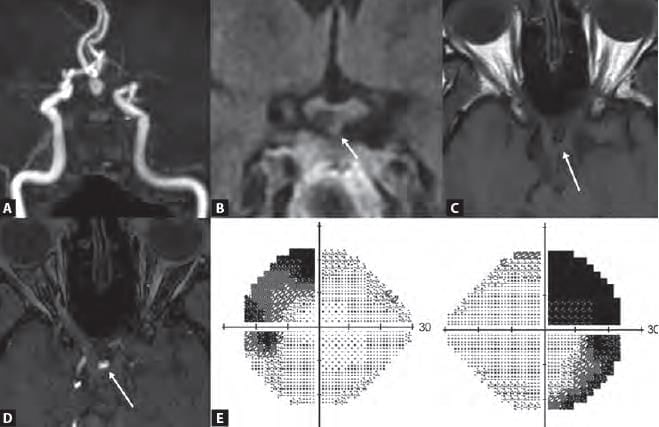
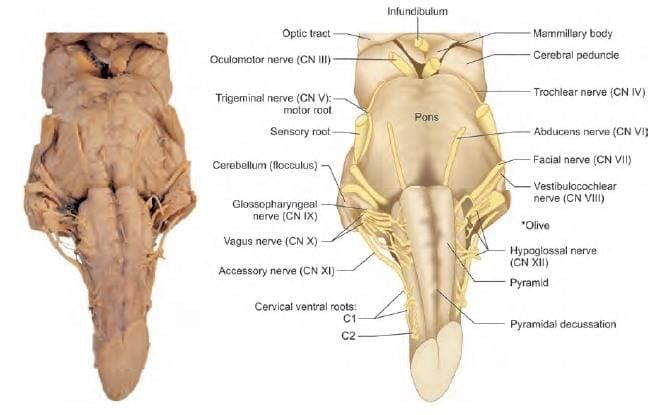
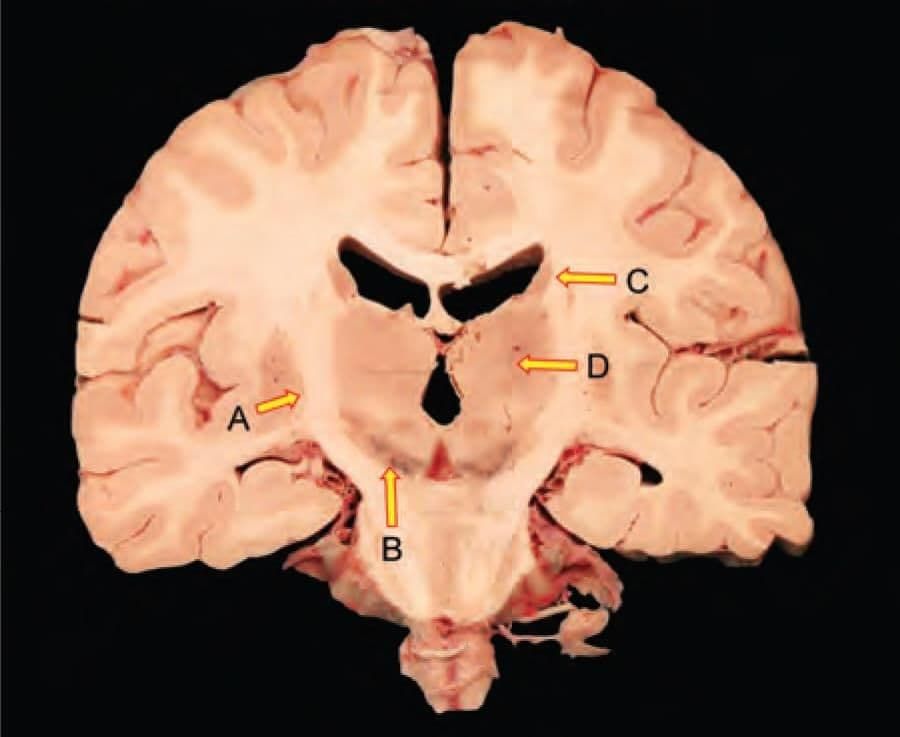
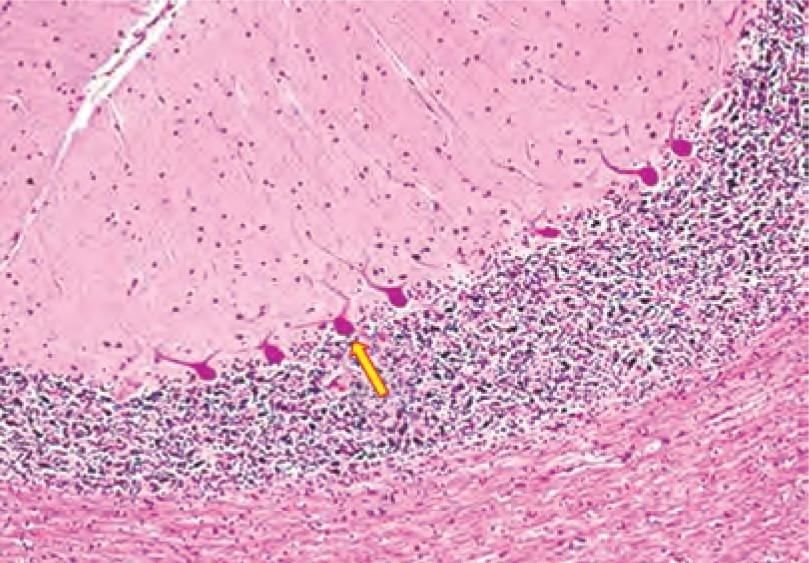
Which cranial nerve fibres are found at point at arrow marked region? (INI-CET Nov 2021)

60-year-old patient complains of pain on touching cold water from tap upto shoulder on right side. No motor deficit is observed upon examination. Which of the following structure is involved? (INI-CET July 2021)
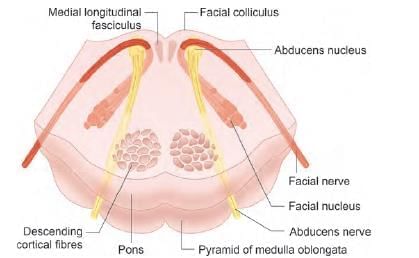
Arrange the following structures in direct pathway of basal ganglia: (INI-CET May 2022)
1. Striaum
2. Substantia nigra
3. Globus pallidus
4. Thalamus
5. Cerebral cortex
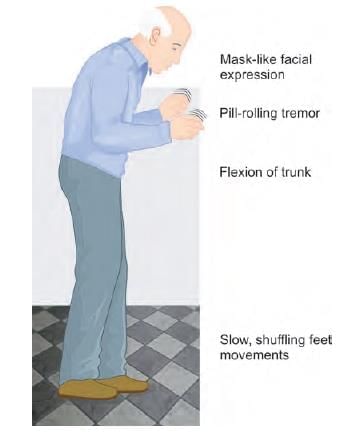
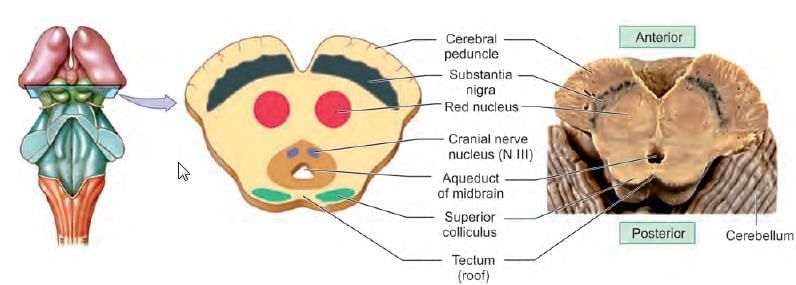
A 75-year-old female has presented with inability to express feelings, bradykinesia, rigidity and resting tremors. The structure most likely involved is: (NEET-PG 2023)
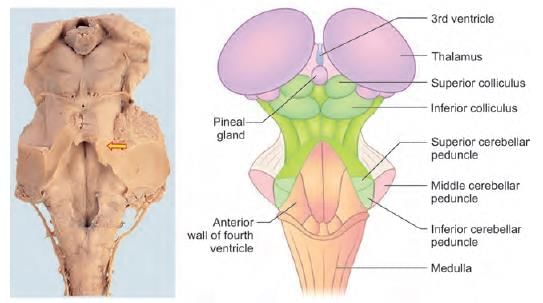
Decussation of superior cerebellar peduncle occurs at: (AIIMS June 2020)
Lesion of the structure producing the elevation marked leads to paralysis of which of the following muscle: (INI-CET May 2022)

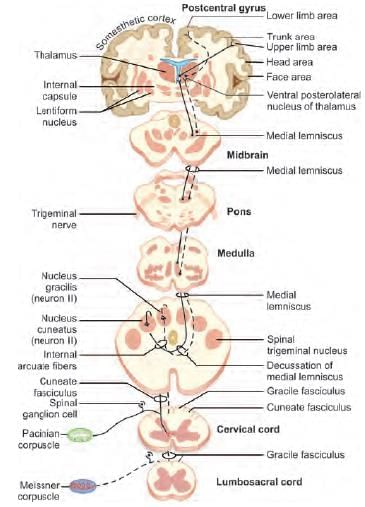
Fibres carried by the marked structure terminate in: (INI-CET July 2021)
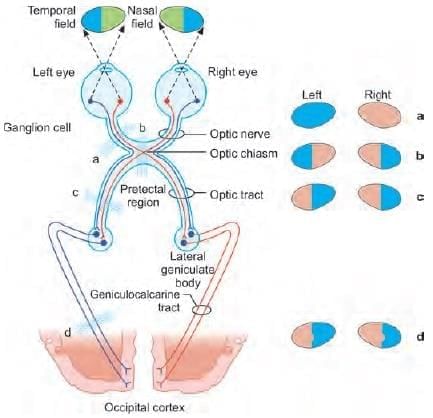
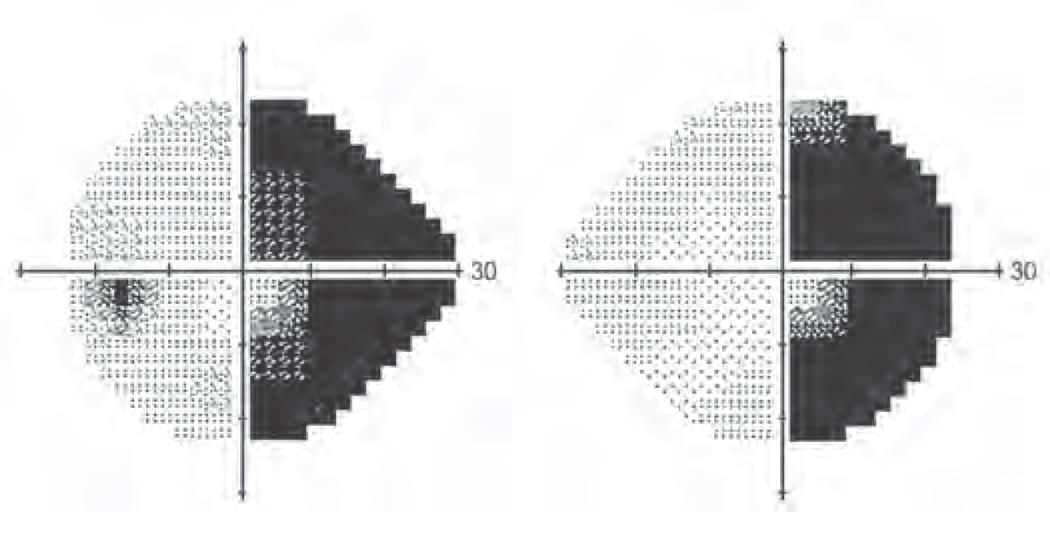
A 23-year-old patient has presented with visual defect as shown in the following diagram. Identify the most likely level of lesion: (INI-CET July 2021, NEET-PG 2021, NEET-PG 2023)
A patient presented with history of vision loss. On investigation an aneurysm was identified causing compression on the optic chiasma. Which is the following artery is most likely involved? (NEET-PG 2021)
The nerve supplying the marked muscle originates at the level of: (INI-CET July 2021)
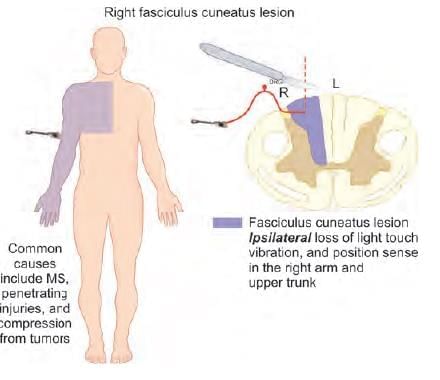
An injury to the lateral part of dorsal column at the cervical region results in loss of proprioception in: (NEET-PG 2023)
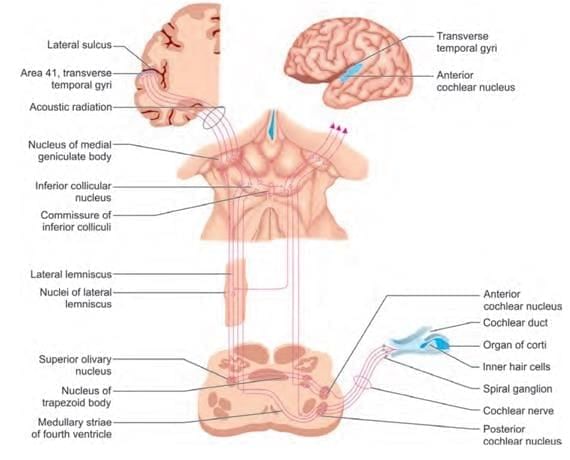
Arrange the following components of auditory pathway in peripheral to central order: (INI-CET May 2023)
1. Inferior colliculus
2. Cochlear nucleus
3. Lateral lemniscus
4. Medial geniculate body
5. Spiral ganglion
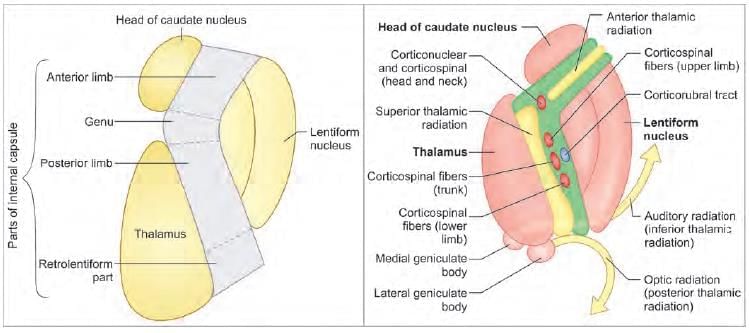
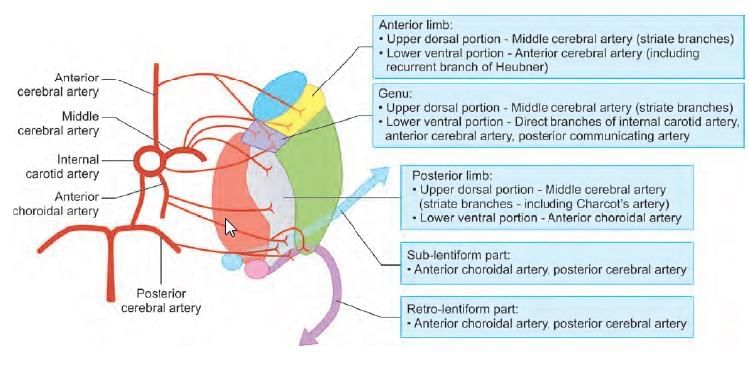
Which of the following statement is FALSE regarding internal capsule? (INI-CET Nov 2022)