Test: Anatomy - 3 - NEET PG MCQ
25 Questions MCQ Test - Test: Anatomy - 3
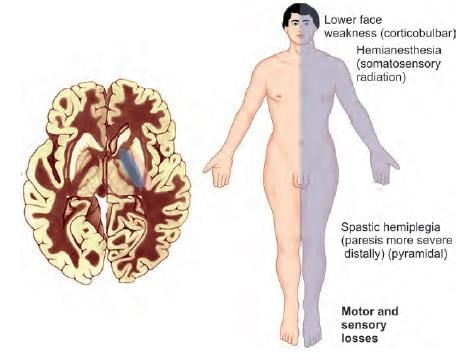
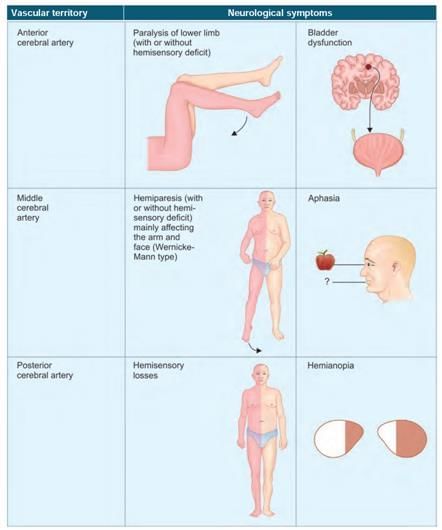
Ischemic stroke of which part of internal capsule leads to contralateral motor loss in upper and lower limb? (AIIMS June 2020)
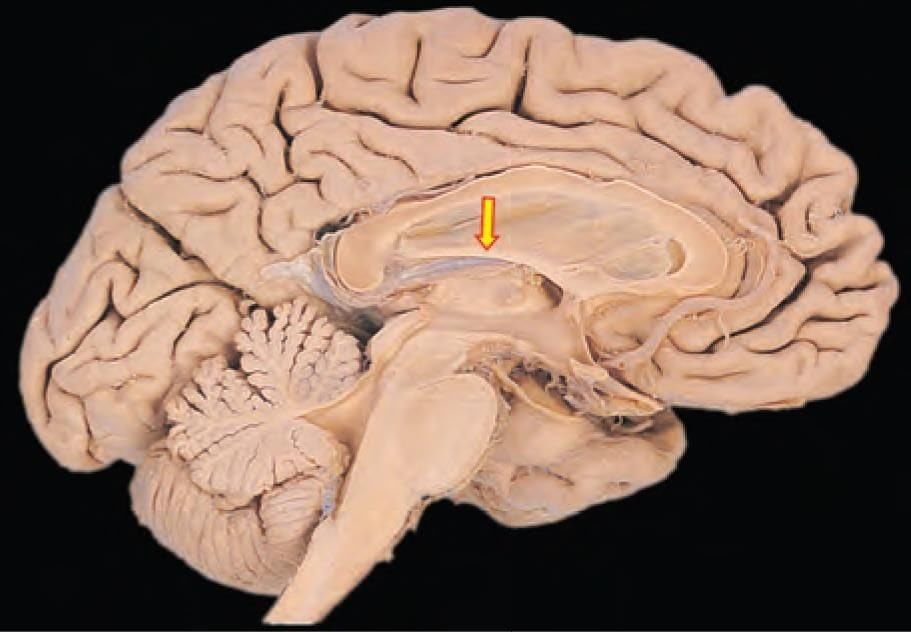
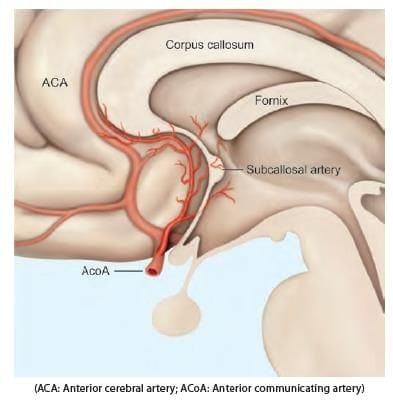
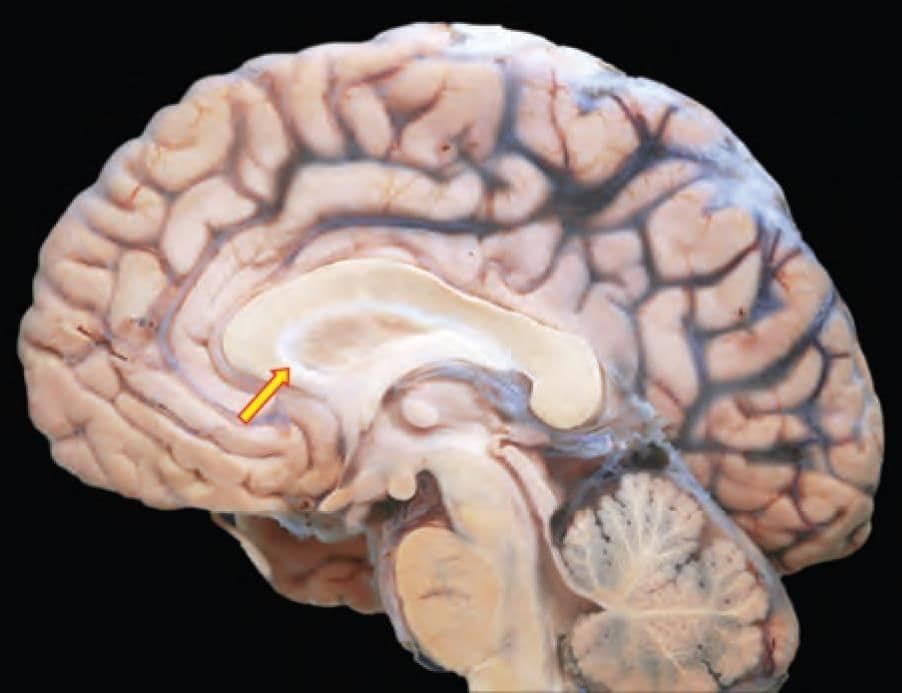
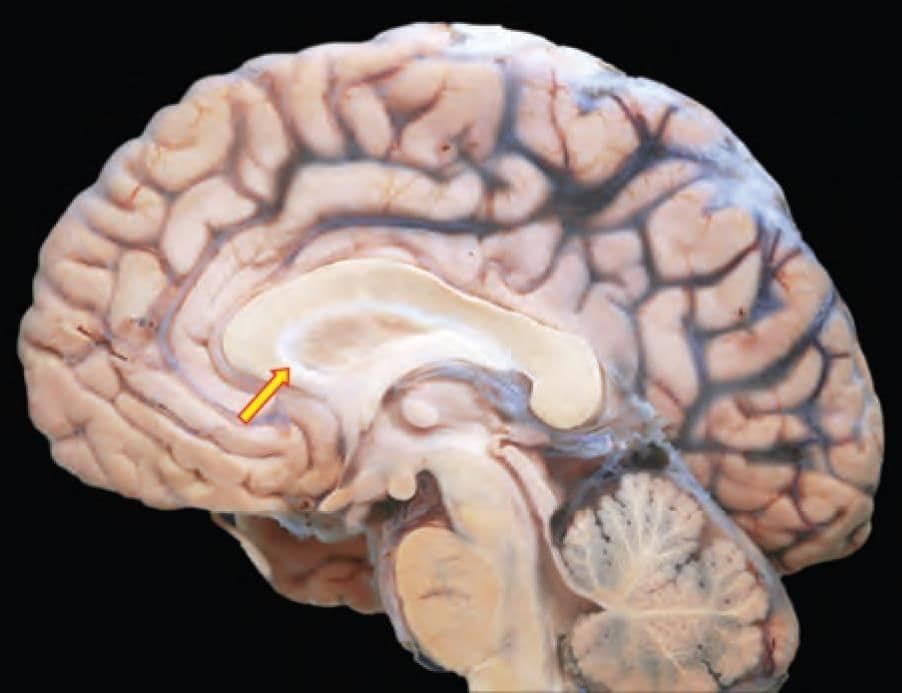
Mention the arterial supply of the marked structure: (INI-CET May 2022)
A patient presented with clinical features of ataxia and incoordination. It is most likely due to involvement of which artery among the following? (NEET-PG 2020)
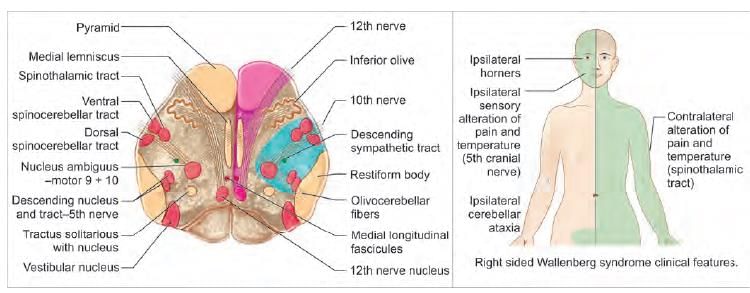
A patient presented with weakness of the right side of the face. There is associated ipsilateral loss of pain and temperature on face and contralateral body. The lesion is most likely located at: (NEET-PG 2020)
A patient presents with sudden onset of dysarthria, sensory loss of right side of face, right upper limb ataxia, tendency to fall on the right side. There is sensory loss on left side of body (with no motor symptoms). Which artery is involved? (AIIMS June 2020)
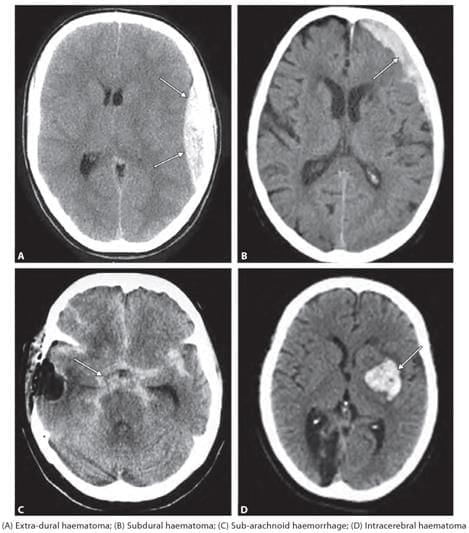
A 55-year-old patient presented with headache and confusion. There is a history of fall one week back. He also has personal history of chronic alcoholism. NCCT findings as shown below, point towards: (NEET-PG 2023)

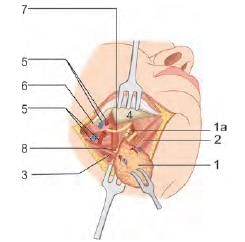
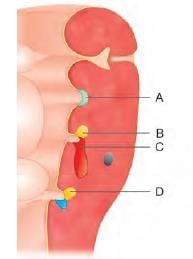
A newborn baby has presented with a pharyngeal pouch developmental anomaly. Facial twitching observed is due to involvement of which of the following marked region? (INI-CET July 2021)
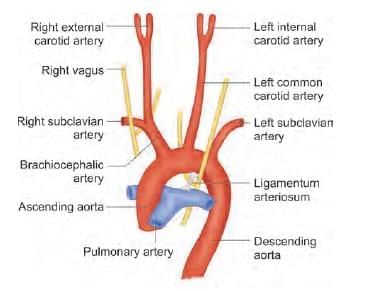
Congenital anomaly shown in the following diagram relates to which of the following pharyngeal arch artery? (NEET-PG 2023)
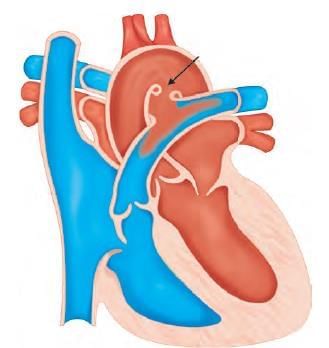
Left recurrent laryngeal nerve has a comparatively longer course due to the persistence of which pharyngeal arch artery? (NEET-PG 2020)
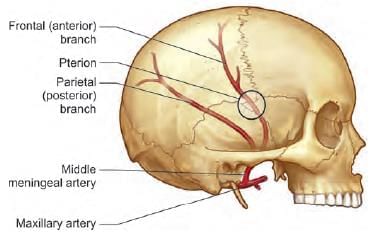
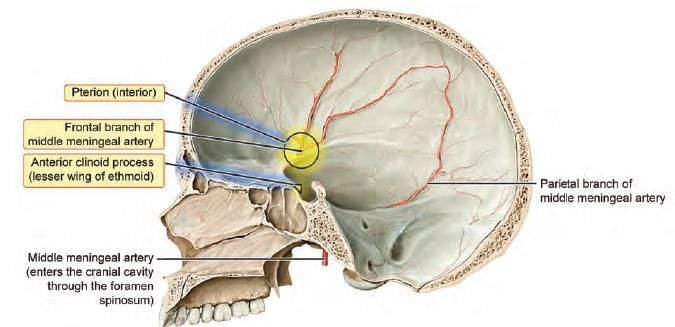
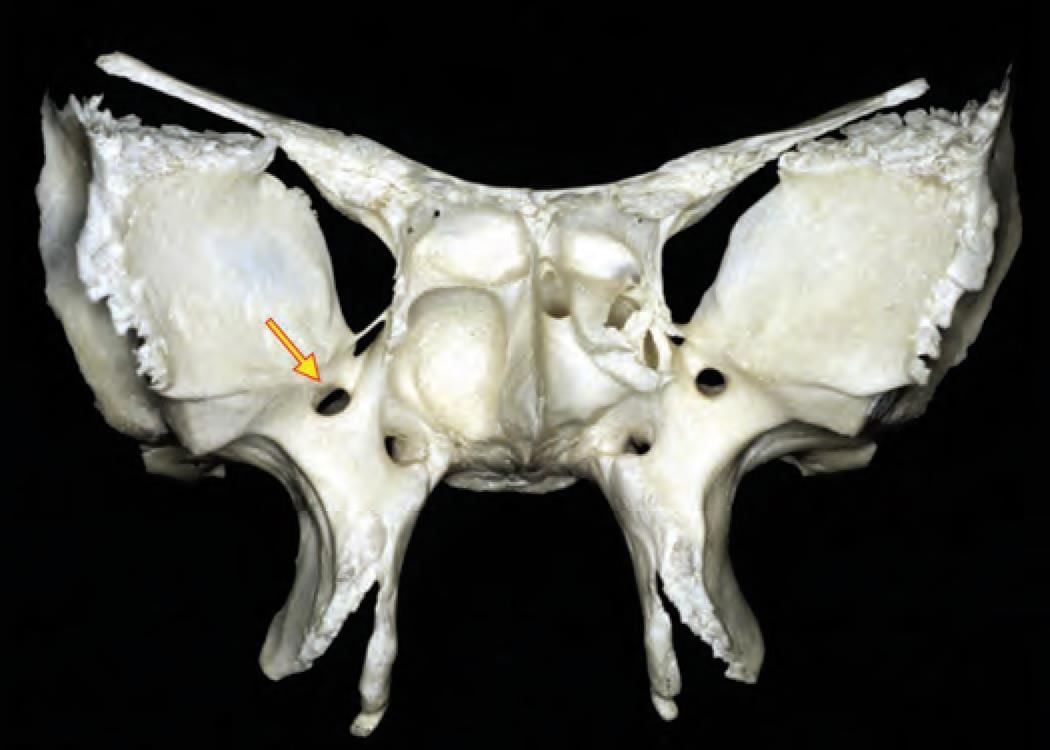
A fracture at the marked arrow (pterion) leads to bleeding of which artery? (AIIMS June 2020)

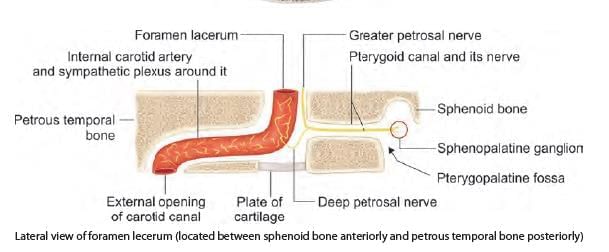
Which structure is deeply related to the arrow marked area? (INI-CET Nov 2020)

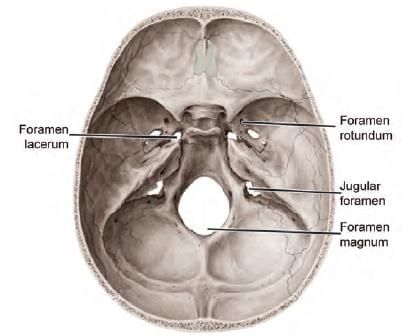
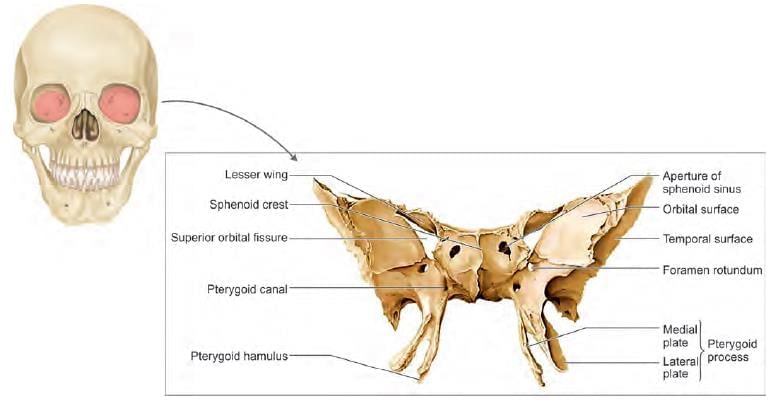
Which of the following foramen is located between three bones? (INI-CET May 2022)
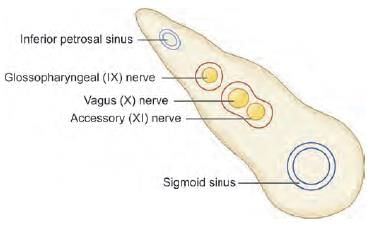
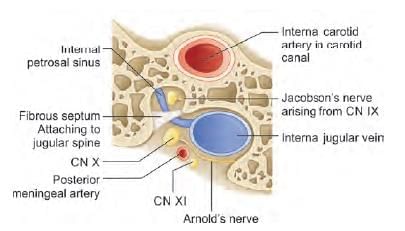
Which of the following structure passing through jugular foramen has separate canal? (INI-CET May 2022)
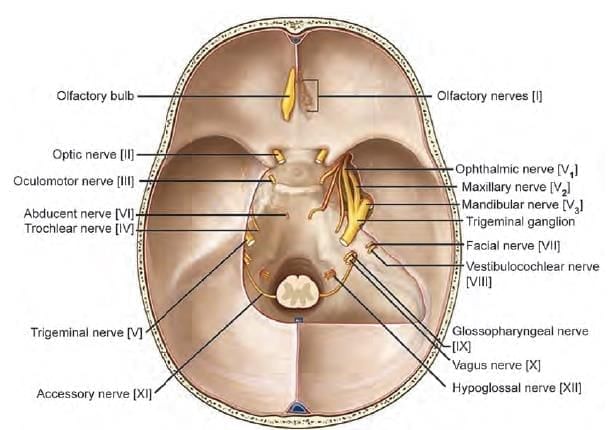
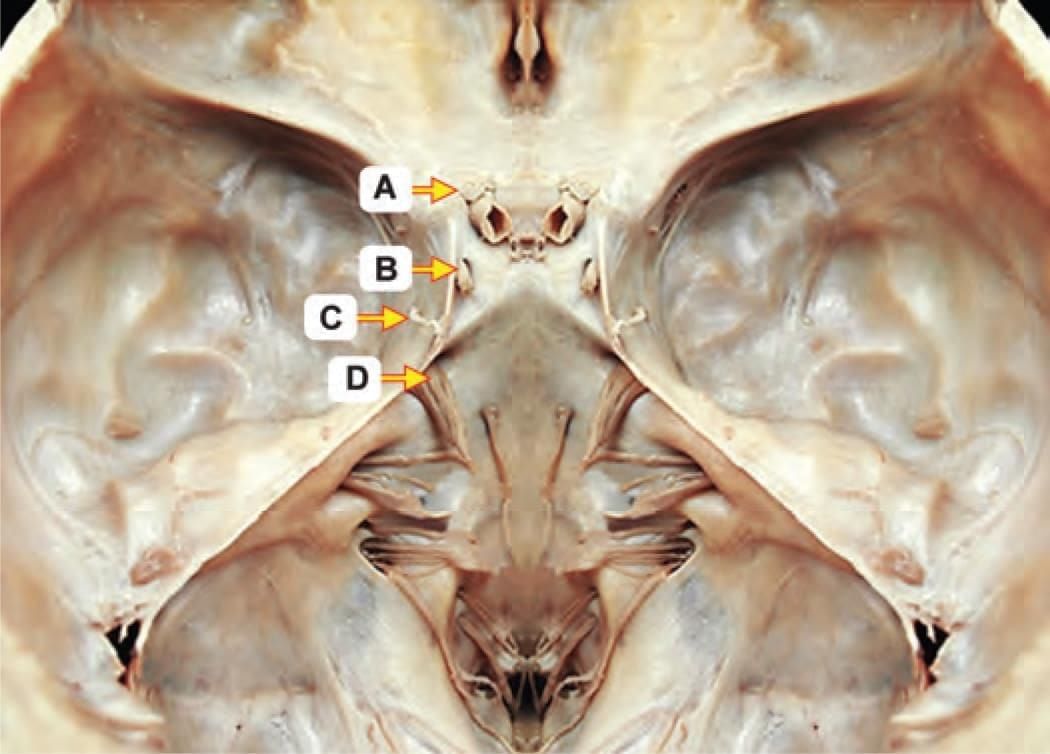
Which of the following marked nerves are associated with ocular movements? (INI-CET Nov 2020)
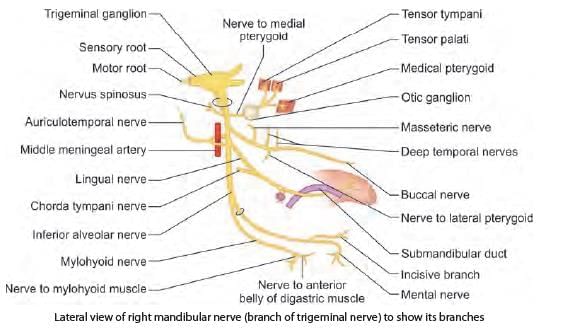
Which of the following is a CORRECT statement regarding mandibular nerve? (INI-CET Nov 2022)
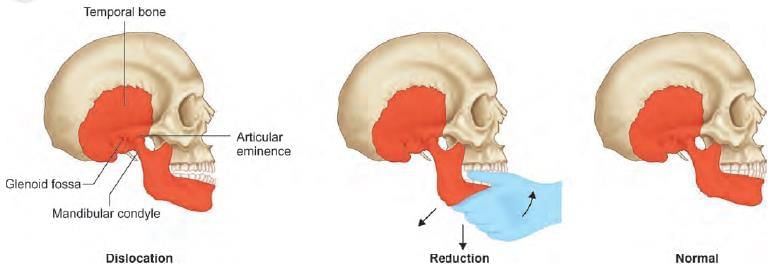
A child has presented with stuck open mouth, which resulted during yawning in the class, as per the given history. Which of the following muscle, attached to articular disc is under spasmodic contraction? (NEET-PG 2023)
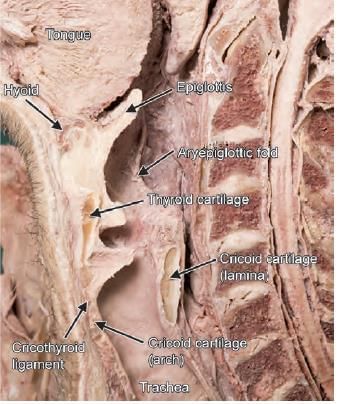
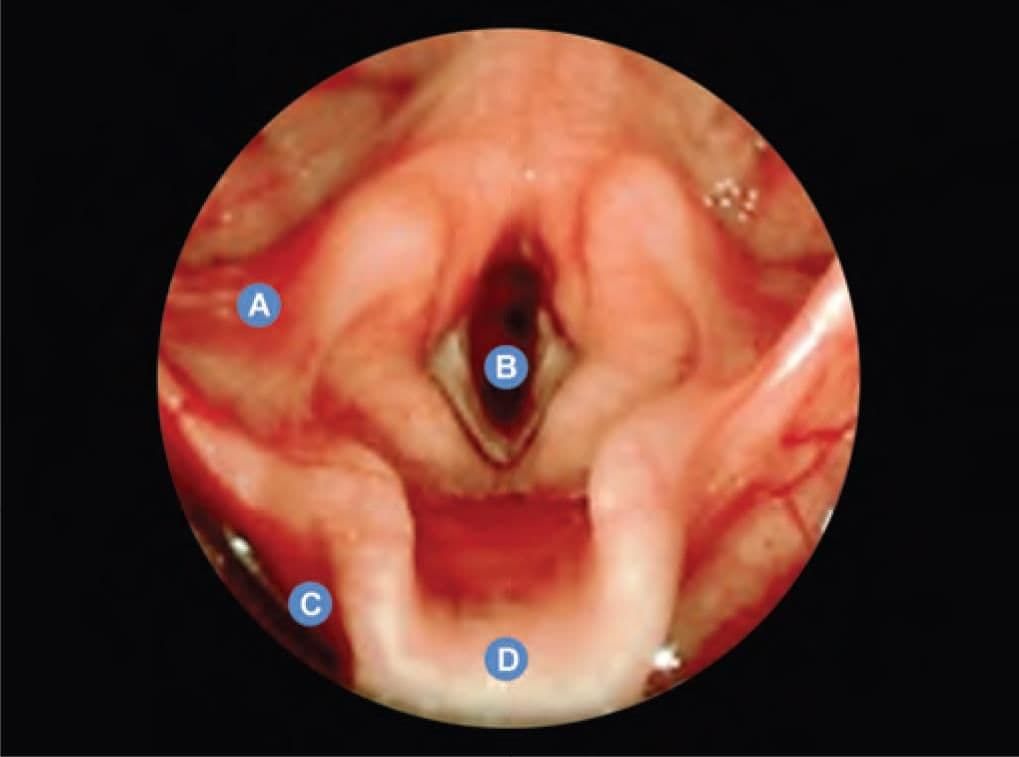
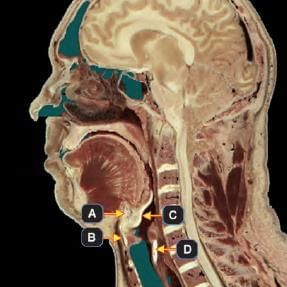
Which of the following marked structures does NOT constitute skeletal framework of larynx? (INI-CET Nov 2020)
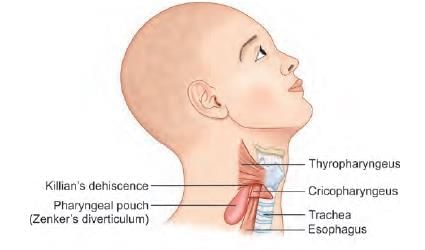
A 70-year-old patient presented with history of fever, halitosis, night cough and regurgitation of food in the mouth. On examination there is a pulsatile swelling on left side of neck which produces gurgling sound on compression. What is the most likely diagnosis, by looking at the given barium swallow study of the patient? (NEET-PG 2020)

A 9-year-old male baby was brought to emergency by the mother with difficulty in swallowing for past few hours and a history of playing unsupervised. X-ray was taken. Identify the location of foreign body. (NEET-PG 2021)

A patient has undergone submandibular gland excision and the Wharton’s duct was ligated in the process. Which of the following nerve is most likely to be damaged during the process of ligating the duct? (NEET-PG 2021)
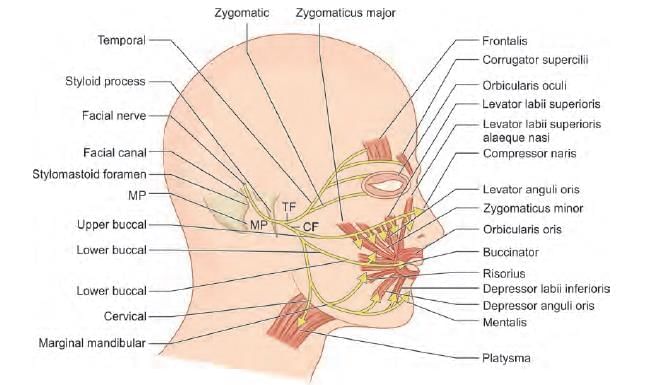
A patient on awakening after parotid surgery, noticed weakness of lower lip movement. Which of the following nerve is most likely injured? (AIIMS June 2020)