Test: Anatomy - 4 - NEET PG MCQ
25 Questions MCQ Test - Test: Anatomy - 4
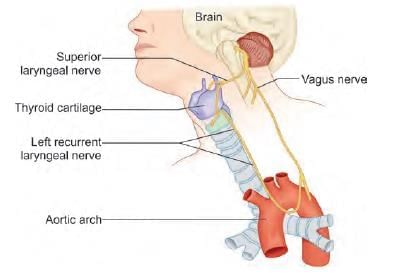
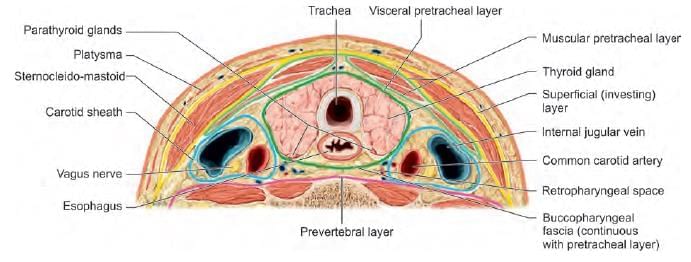
Which of the following nerve is least injured in thyroid surgery? (AIIMS June 2020)
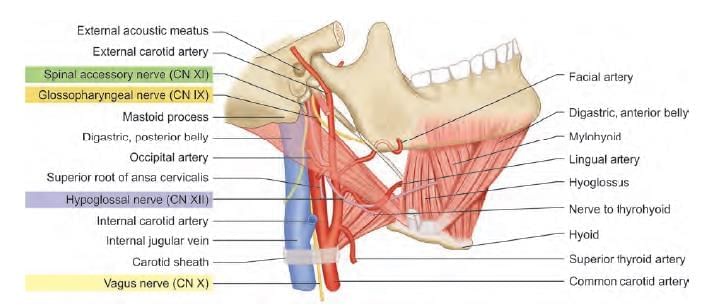
Patient undergoing surgery at the lateral part of skull. Postoperatively patient had aspirations without voice change. Nerve lesioned is: (AIIMS Nov 2019)
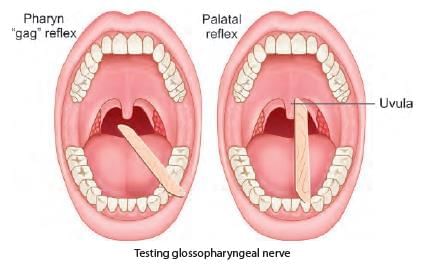
A patient was admitted with skull base trauma and difficulty in swallowing. The doctor was touching the marked structure. Which of the following cranial nerve is being tested? (NEET-PG 2021)


A patient with a fracture skull base at the temporo-occipital region, presented with difficulty in speaking post trauma. During investigation which structure should be tested which helps in diagnosis related with the points marked below? (INI-CET Nov 2021)
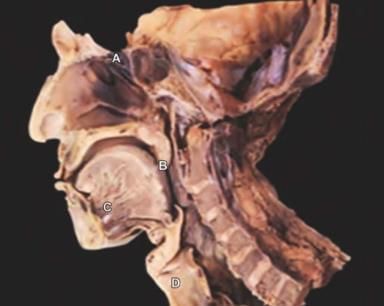
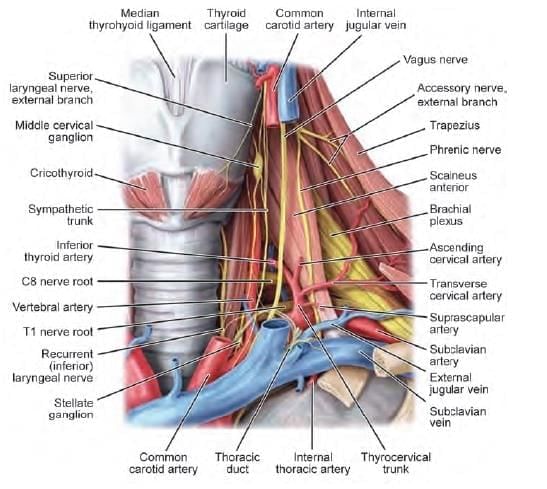
Which of the following arrow marked nerves, if injured present with paradoxical breathing? (INI-CET Nov 2020)
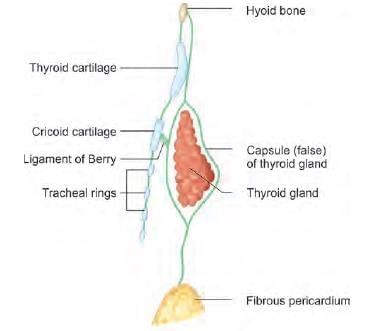
The upward extension of thyroid swelling is prevented by which of the following structure attached to thyroid cartilage? (NEET-PG 2020)
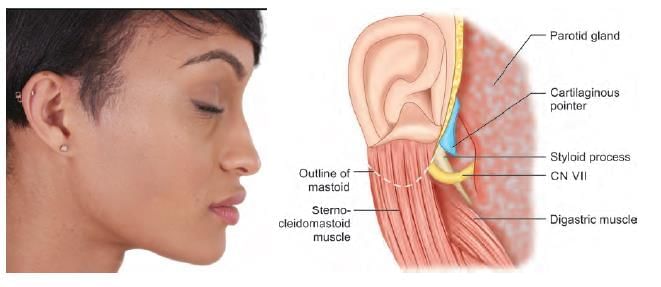
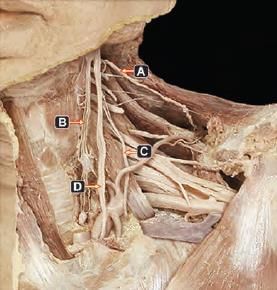
NOT an anatomical landmark of facial nerve identification in parotid surgery: (NEET-PG 2020p)
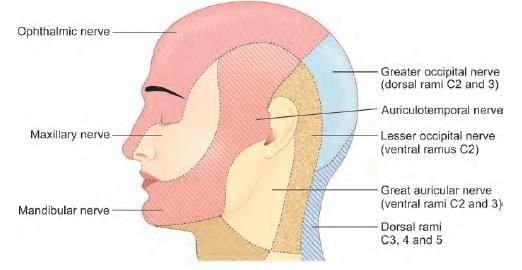
Post parotidectomy, patient feels numb while shaving. Which nerve was involved? (AIIMS May 2019)
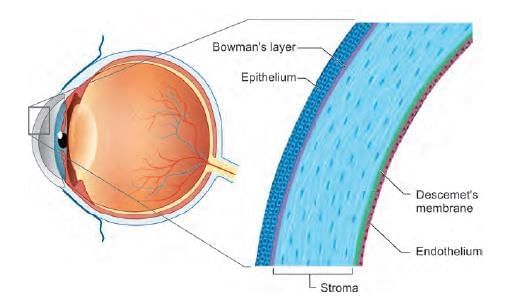
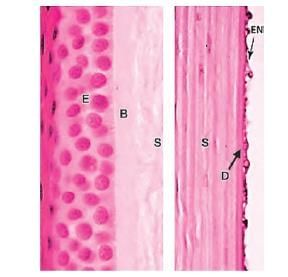
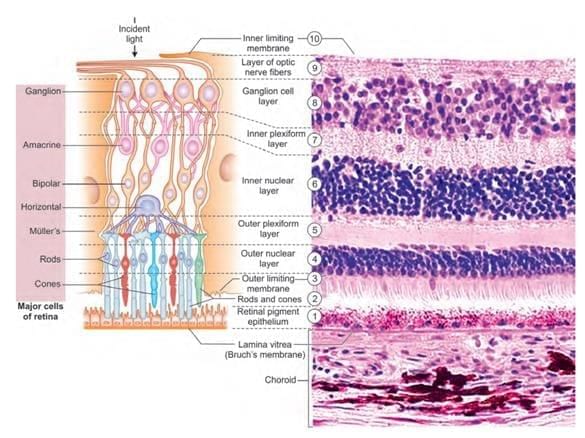
Which layer maintains hydration of corneal stroma? (NEET-PG 2020p)
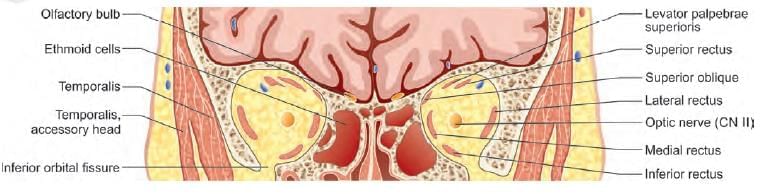
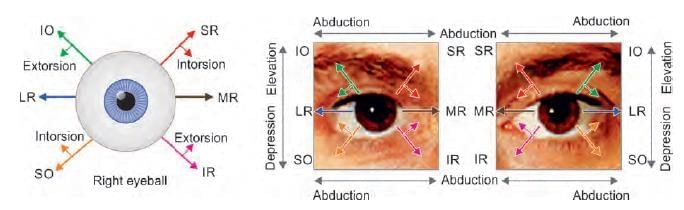
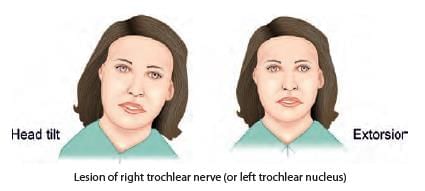
A patient presented with squint in right eye, as shown below. Identify the nerve lesioned in this case: (NEET-PG 2020p)

A child presented with left sided head tilt. On head straightening, there is right hypotropia, which increases on tilting head to right side. Which of the following muscle is paralysed? (AIIMS June 2020)
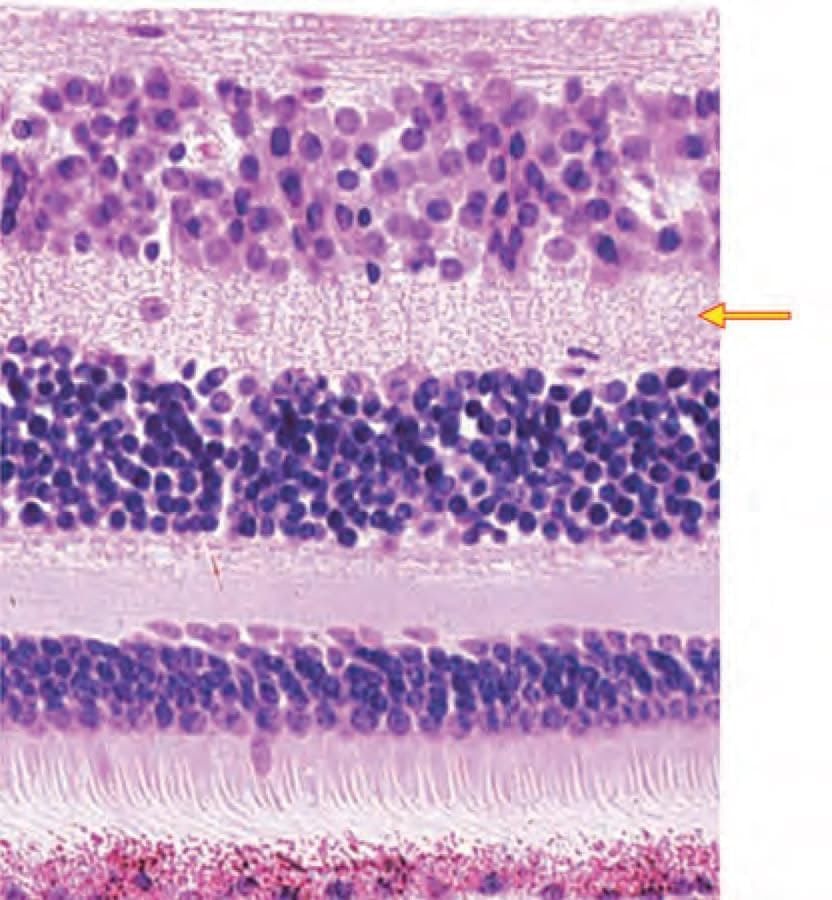
Identify the marked layer in the given histological section: (AIIMS Nov 2019)
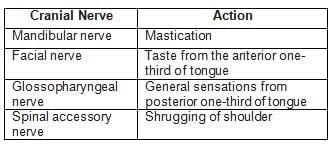
Match the following cranial nerves with their corresponding actions: (INI-CET May 2023)
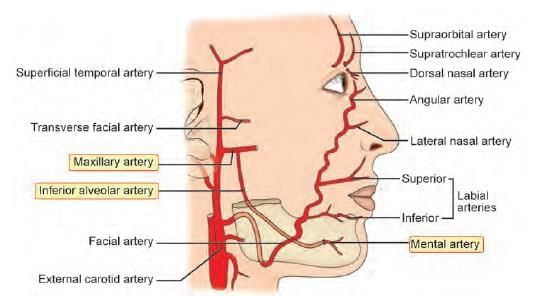
Which of the following is NOT a branch of facial artery? (INI-CET May 2022)
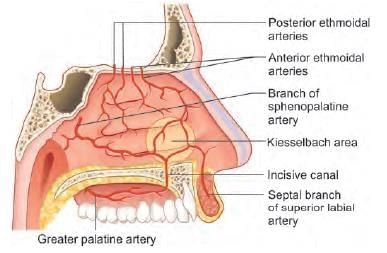
External carotid artery supplies nasal septum by all of the following branches, except: (AIIMS May 2019)
Inferior thyroid artery supplies: (INI-CET Nov 2021)
A. Oesophagus
B. Thyroid
C. Parathyroid
D. Thymus
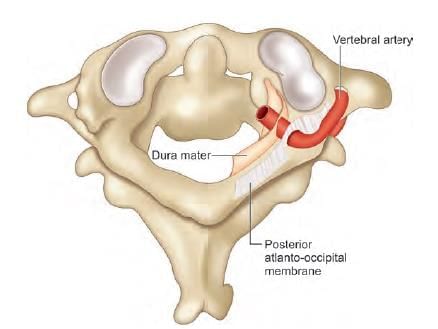
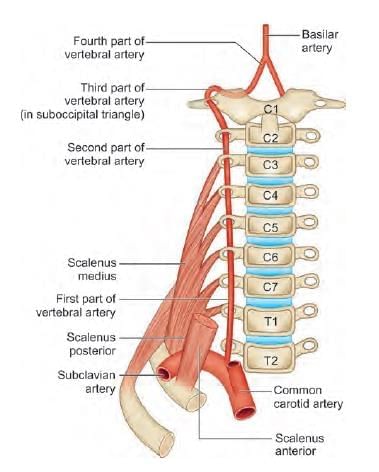
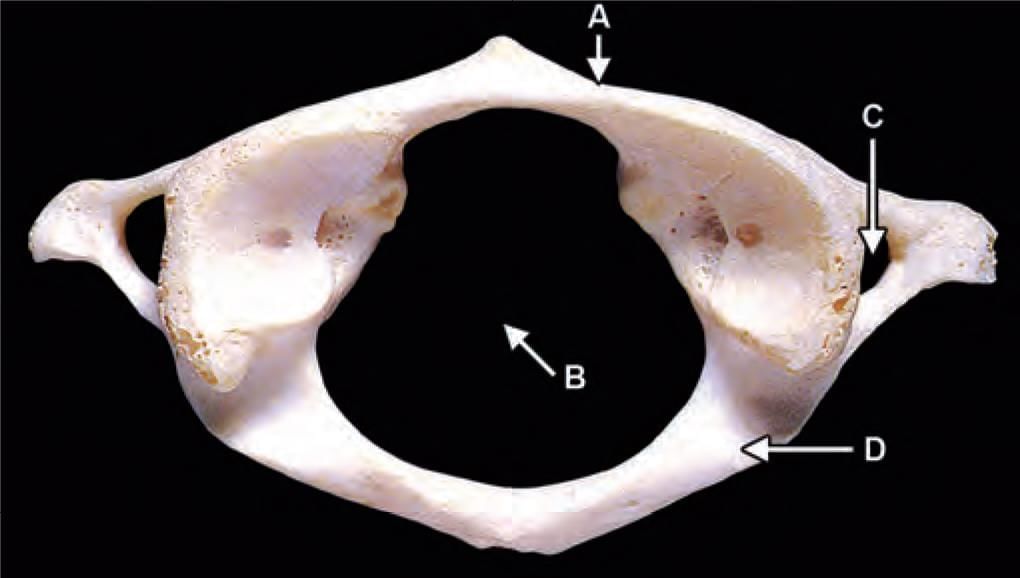
Third part of vertebral artery is related to which of the following marked region in the following diagram? (INI-CET Nov 2021)
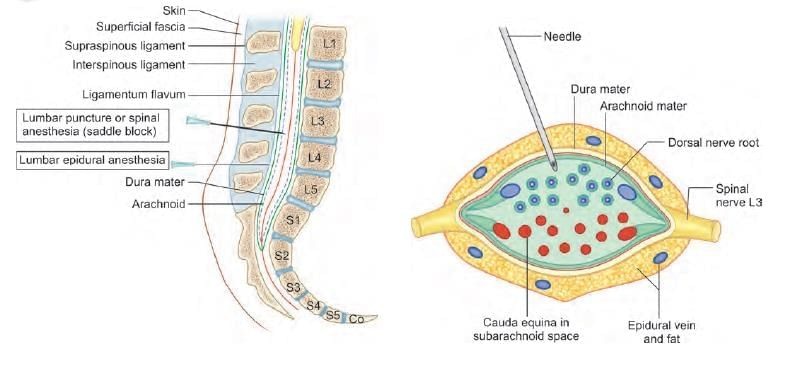
While doing lumbar puncture, which of the following structure is pierced before entering the lumbar cistern? (NEET-PG 2021)
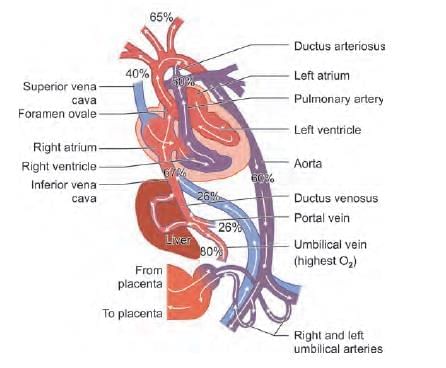
Which vessel carries deoxygenated blood back to placenta in fetal circulation? (NEET-PG 2021)
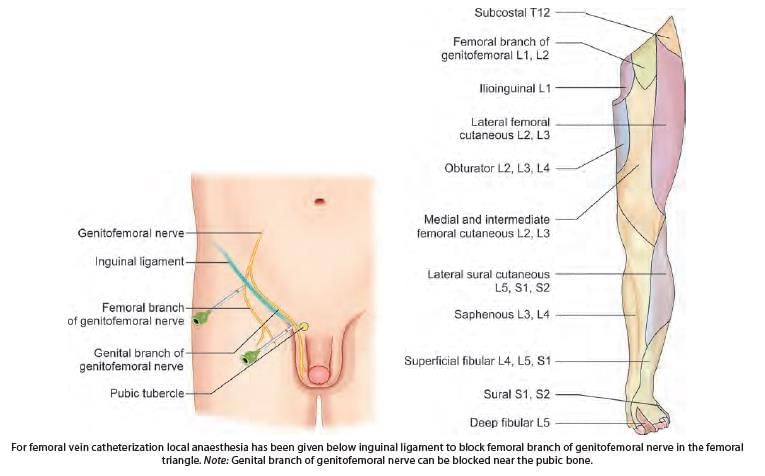
For femoral vein catheterization local anaesthesia has been given below inguinal ligament. Which of the following nerve is blocked?