Test: Aortic Dissection & Infective Endocarditis - NEET PG MCQ
15 Questions MCQ Test - Test: Aortic Dissection & Infective Endocarditis
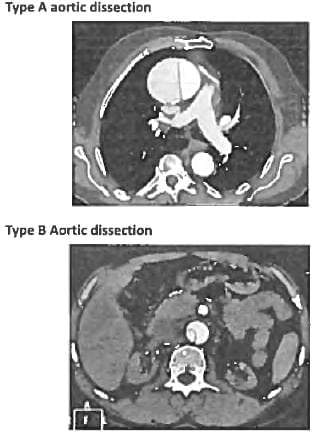
A 50-year male presented with high BP of 160/100 mm Hg and heart rate of 120/min. CECT is shown below. Which is best management of this condition? (AIIMS May 2018)


A 70-year-old man with Hypertension wakes up with severe chest pain and diaphoresis. On examination he has bounding pulses with wide pulse pressure. A diastolic murmur is heard along the right sternal border. Which of the following is the possible aetiology? (Recent Question 2019)
A 65-year old hypertension patient presents with Chest pain, difficulty in breathing for I hour. Chest X-ray done shows presence of:


Investigation of choice for aortic dissection with hypotension is ? (Recent Pattern 2014-15)
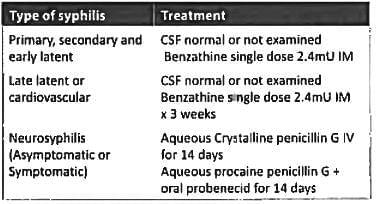
Treatment of choice for late cardiovascular syphilis is? (AIIMS May 2018)
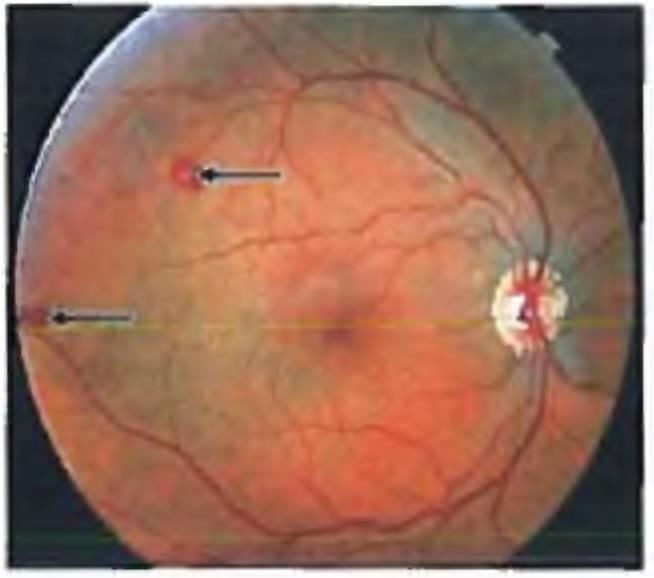
A 50 year man came with a 'grey spot' in his vision. He had recurrent fevers and weight loss for the past 3 months. He had a history of mitral valve infection. Vision is 6/6. This is the picture of his fundus. Choose the FALSE statement? (APPG 2016)
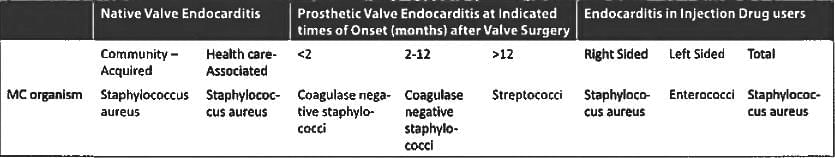
Which of the following is not a part of Duke Criteria for infective endocarditis? (AIIMS May 15)
Osler's nodes are seen in? (Recent Pattern 2014-15)
What is not true about infective endocarditis? (Recent Pattern 2014-15)
Most common cause of infective endocarditis is? (Recent Pattern 2014-15)