Test: Arrhythmias and Emergency Medicine- 3 - NEET PG MCQ
15 Questions MCQ Test - Test: Arrhythmias and Emergency Medicine- 3
Unconscious child, CPR was started and ECG shows normal QRS but peripheral pulse was absent inspite of chest compressions. What should be done next? (JIPMER Nov 2015)
New onset atrial flutter. Best treatment is? (JIPMER Nov 2015)
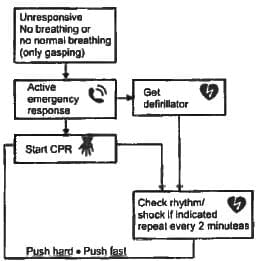
A 75-year-old patient clutches chest and falls down. A Physician arrives on the scene. What is the first thing to be done by the physician? (JIPMER Nov 2015)
A 55-year-old hypertensive patient has a standing BP 190/10 and sitting BP-180/100. He also has irregularly irregular rhythm, double apical impulse and bilateral basal crepitations. But no murmurs could be auscultated and heart rate could not be determined. What is the likely cause? (JIPMER Nov 2014)
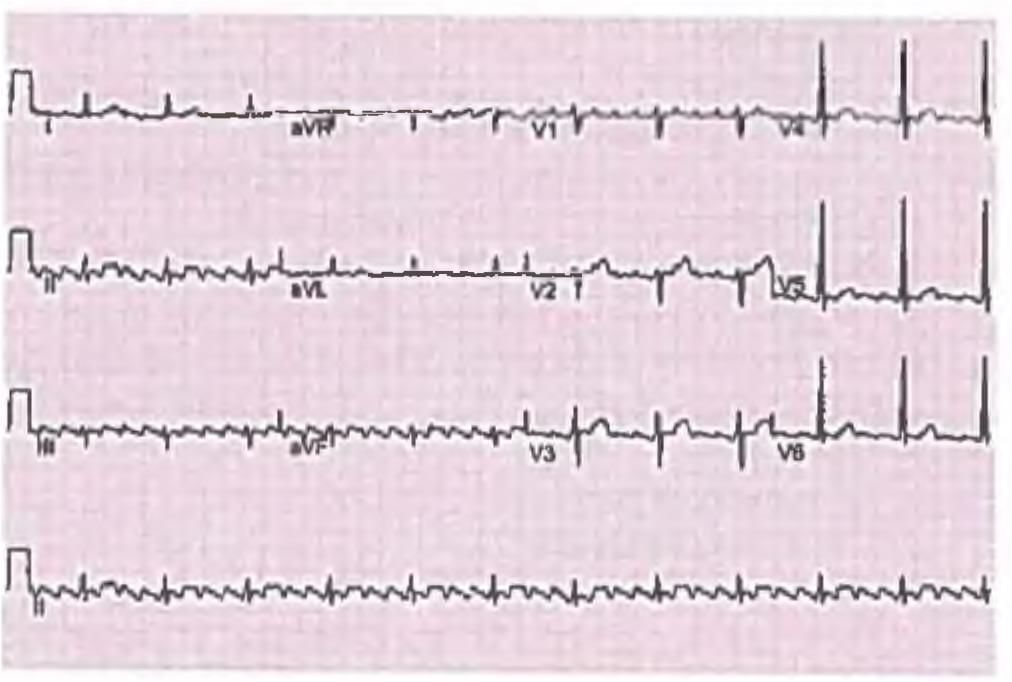
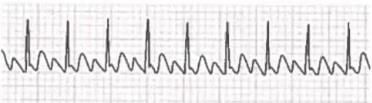
A 62-year-old male with underlying COPD develops a viral upper respiratory infection and begins taking an over-the counter decongestant. Shortly thereafter he experiences palpitations and presents to the emergency room, where the given rhythm strip is obtained, demonstrating: (Recent Question 2015-16)
A 40-year-old Lady intraoperatively develops HR 220 bpm and Blood pressure of 70/40, ECG shows qRS complex Ł 110 milliseconds. Best management is? (JIPMER 2014)
Most common arrhythmia in ICU patients: (Recent Pattern 2015-16)
Most common mechanism of arrhythmia? (Recent Pattern 2014-15)
All of the following electrocardiographic findings may represent manifestations of digitalis intoxication, except: (Recent Pattern 2014-I5)
40-year-old female patient develops recurrent episodes of sudden palpitations with HR = 150/min, rhythm regular. After every episode she has diuresis. What could be the cause? (Recent Pattern 2014-15)
Atrial fibrillation may occur in all the following conditions, except- (Recent Pattern 2014-15)
Which of the following arrhythmia is most commonly associated with alcohol binge in alcoholics? (Recent Pattern 2014-15)