Test: Malabsorption Syndrome, Pediatric Gastroenterology & MALT-oma - NEET PG MCQ
25 Questions MCQ Test - Test: Malabsorption Syndrome, Pediatric Gastroenterology & MALT-oma
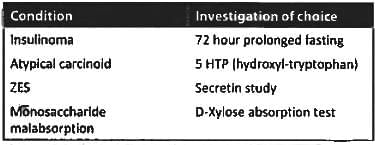
Which test is recommended for this patient? (Recent Question 2019)
Which is the most important complication of celiac sprue? (Recent Question 2016-17)
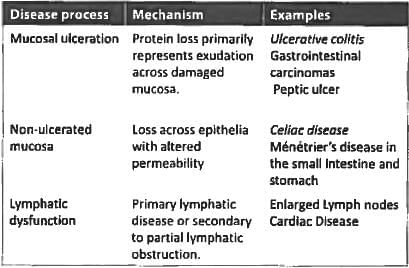
The following conditions can cause protein-losing enteropathy except? (UPSC 2015)
Malabsorption syndrome features include all, except: (Recent Pattern 2014-15)
Anti - T.T.G antibodies are seen in: (Recent Pattern 2014-15)
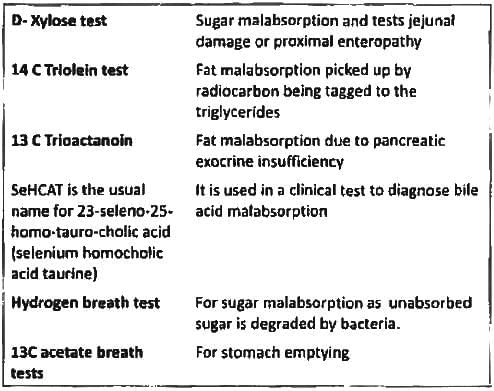
Xylose absorption test is used to assess: (Recent Pattern 2014-15)
Protein losing enteropathy is characterized by all except: (Recent Pattern 2014-15)
Alpha 1 anti-tryspin in stool is indicative of? (Recent Pattern 2014-15)
Jejunal biopsy is diagnostic in: (Recent Pattern 2014-15)
True about tropical sprue are A/E: (Recent Pattern 2014-15)
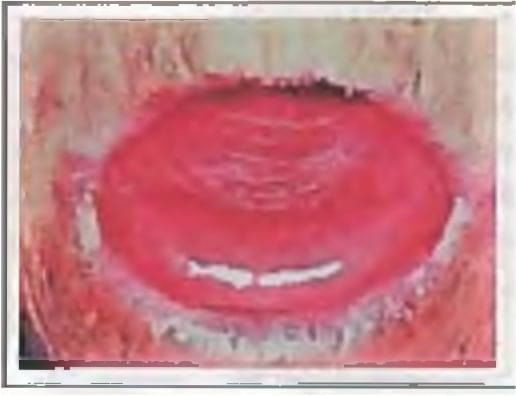
A 30-year-old lady presents with features of malabsorption and iron deficiency anaemia. Duodenal biopsy shows complete villous atrophy. Probable diagnosis is: (Recent Pattern 2014-15)
In celiac sprue there is a deficiency of all except: (Recent Pattern 2014-15)
Not included in armamentarium of tests for malabsorption syndrome (AIIMS May 2013)
Malabsorption syndrome does not result from: (Recent Pattern 2014-15)
Non-tropical sprue is characterized by: (Recent Pattern 2014-15)
Consider the following:
a. Visible gastric peristalsis
b. Bilious vomiting
c. Palpable mass
d. Melena
Which of the above is/are the feature/features of infantile hypertrophic pyloric stenosis? (UPSC 2015)
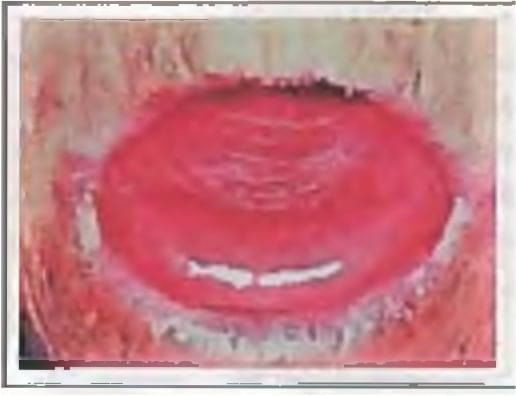
A Term neonate with respiratory distress since birth. The CXR shows?

A neonate has been diagnosed with necrotizing enterocolitis with X ray abdomen showing gas in the portal vein. The correct staging of the patient is ? (Recent Pattern 2014-15)
Exposure to which of the following drugs is incriminated in IHPS (infantile hypertrophic pyloric stenosis): (Recent Pattern 2014-15)
All of the following are true regarding primary gastric lymphoma, except? (APPG 2016)
Which is the most common site of MALT? (AIMS Nov 2014)