Clinical Microbiology (Infective Syndromes) Chapter Notes | Microbiology - NEET PG PDF Download
| Table of contents |

|
| Urinary Tract Infections (UTIs) |

|
| Diarrhea, Dysentery and Food Poisoning |

|
| Meningitis |

|
| Bloodstream Infections |

|
| Other Infective Syndromes |

|
| Microbiological Profile of Osteomyelitis |

|
Urinary Tract Infections (UTIs)
Lower UTI
- Sites involved: Urethra and bladder
- Symptoms: Local manifestations including dysuria, urgency, and frequency
- Route of spread: Ascending route
- Occurrence: More common
Upper UTI
- Sites involved: Kidney and ureter
- Symptoms: Local and systemic manifestations such as fever, vomiting, and abdominal pain
- Route of spread: Both ascending which is common and descending route
- Occurrence: Less common
Microorganisms causing UTI
- Bacterial agents:
- Gram-negative bacilli:
- Escherichia coli as the commonest agent of UTI
- Proteus mirabilis
- Klebsiella pneumoniae
- Pseudomonas aeruginosa
- Acinetobacter species
- Enterobacter species
- Serratia species
- Gram-positive cocci:
- Staphylococcus saprophyticus
- Staphylococcus aureus
- Staphylococcus epidermidis
- Enterococcus spp.
- Gram-negative bacilli:
- Other agents:
- Fungus: Candida albicans
- Parasites:
- Schistosoma haematobium
- Trichomonas vaginalis
- Viruses:
- Herpes simplex virus
- Adenovirus
- JC and BK virus
- Cytomegalovirus
- Most organisms are acquired by ascending route. Organisms acquired by descending route include Staphylococcus aureus, Salmonella, Mycobacterium tuberculosis, Leptospira and Candida
- For example, in ascending route infections, bacteria like Escherichia coli travel from the urethra upwards to the bladder, illustrating how proximity to external environments facilitates common lower UTIs
Diarrhea, Dysentery and Food Poisoning
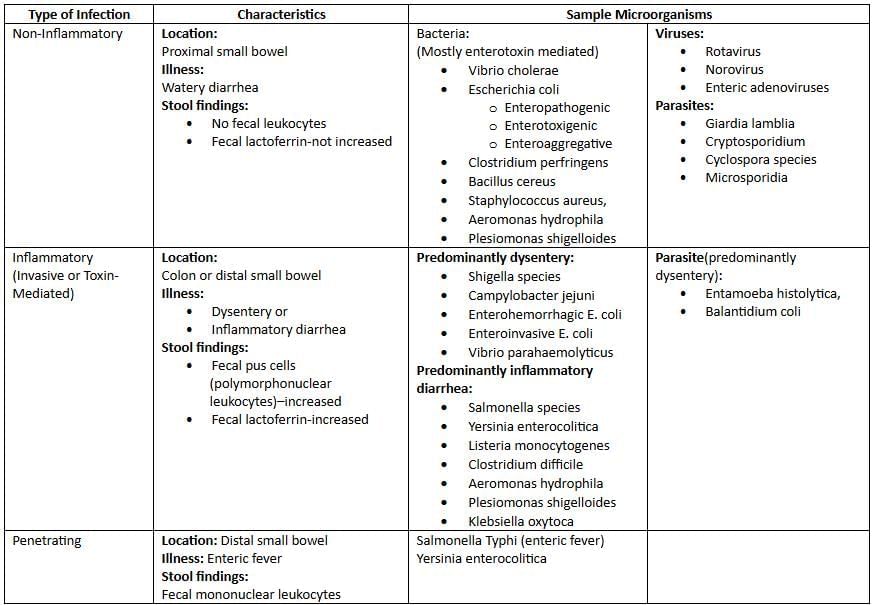
Infectious agents of acute diarrhea and the underlying mechanism
Infectious agents causing food poisoning
- 1–6 h incubation period
- Staphylococcus aureus
- Symptoms: Nausea, vomiting, diarrhea
- Common food sources: Ham, poultry, potato or egg salad, mayonnaise, cream pastries
- Bacillus cereus
- Symptoms: Nausea, vomiting, diarrhea
- Common food sources: Fried rice
- Clostridium botulinum
- Symptoms: Nausea, vomiting, diarrhea
- Common food sources: Canned food
- Staphylococcus aureus
- 8–16 h incubation period
- Clostridium perfringens
- Symptoms: Abdominal cramps, diarrhea vomiting rare
- Common food sources: Beef, poultry, legumes, gravies
- B. cereus
- Symptoms: Abdominal cramps, diarrhea vomiting rare
- Common food sources: Meats, vegetables, dried beans, cereals
- Clostridium perfringens
- > 16 h incubation period
- Vibrio cholerae
- Symptoms: Watery diarrhea
- Common food sources: Shellfish, water
- Enterotoxigenic E. coli
- Symptoms: Watery diarrhea
- Common food sources: Salads, cheese, meat, water
- Enterohemorrhagic E. coli
- Symptoms: Bloody diarrhea
- Common food sources: Ground beef, roast beef, salami, raw milk, raw vegetables, apple juice
- Salmonella species
- Symptoms: Inflammatory diarrhea
- Common food sources: Beef, poultry, eggs, dairy products
- Campylobacter jejuni
- Symptoms: Inflammatory diarrhea
- Common food sources: Poultry, raw milk
- Shigella species
- Symptoms: Dysentery
- Common food sources: Potato or egg salad, lettuce, raw vegetables
- Vibrio parahaemolyticus
- Symptoms: Dysentery
- Common food sources: Mollusks, crustaceans
- Vibrio cholerae
For example, Staphylococcus aureus food poisoning often arises from improperly stored cream-based desserts, where preformed toxins cause rapid onset symptoms within hours, highlighting the importance of refrigeration in preventing such outbreaks
Agents of Traveller’s diarrhea
Etiologic agent:
- Bacteria 50–75%
- Enterotoxigenic Escherichia coli 10–45%: Single most important agent
- Enteroaggregative E. coli 5–35%: Emerging enteric pathogen with worldwide distribution
- Campylobacter jejuni 5–25%: More common in Asia
- Shigella: Major cause of dysentery
- Salmonella: Common in India
- Others: Aeromonas, Plesiomonas, and Vibrio cholerae
- Viruses < 20%
- Norovirus < 10%: Associated with cruise ships
- Rotavirus < 5%: Common among children
- Parasites 0–10 %: Giardia lamblia, Cryptosporidium, Entamoeba histolytica, Cyclospora
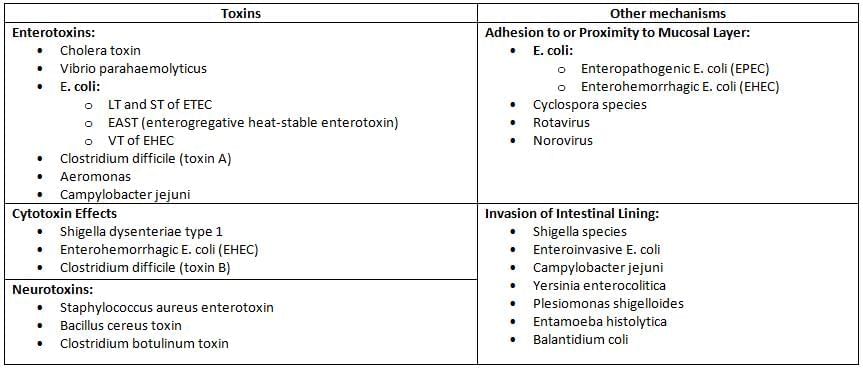
Pathogenic mechanisms of diarrheal agents
Meningitis
Causes of meningitis (pyogenic and aseptic)
- Pyogenic meningitis
- Neonates or infants of 0–2 months
- Escherichia coli
- Group B streptococcus S. agalactiae
- Listeria monocytogenes
- Other Gram-negative bacilli like Klebsiella pneumoniae
- 2–20 years
- Neisseria meningitidis: Most common agent
- Haemophilus influenzae
- Streptococcus pneumoniae
- > 20 years adults
- Streptococcus pneumoniae: Most common agent
- Haemophilus influenzae
- Neisseria meningitidis
- Overall: Most common agent is Streptococcus pneumoniae
- Neonates or infants of 0–2 months
- Aseptic meningitis
- Viruses
- Enteroviruses Polioviruses, echoviruses, Coxsackie viruses: The most common agents
- Herpes simplex virus 1 and 2
- Other Herpes group: Varicella zoster, CMV, EBV
- Myxoviruses: Influenza A and B, parainfluenza virus, and mumps virus
- Arboviruses, and adenoviruses
- Rubella viruses and HIV
- Bacteria: Treponema pallidum, and Leptospira
- Parasites: Naegleria species, Acanthamoeba species and Toxoplasma gondii
- Fungi: Cryptococcus neoformans
- Viruses
For example, in neonates, Group B streptococcus often causes pyogenic meningitis due to maternal colonization, emphasizing the role of perinatal screening to prevent such infections
Cytological and biochemical parameters in CSF of normal individuals and in different types of meningitis
- CSF pressure mm of water
- Normal individual: Normal 50–150
- Pyogenic meningitis: Highly elevated >180
- Tuberculous meningitis: Moderately elevated
- Viral meningitis: Slightly elevated/normal
- Total leukocyte count per mm3
- Normal individual: 0–5
- Pyogenic meningitis: 100–10,000
- Tuberculous meningitis: 10–500
- Viral meningitis: 25–500
- Predominant cell
- Normal individual: Lymphocytes
- Pyogenic meningitis: Neutrophils
- Tuberculous meningitis: Lymphocytes
- Viral meningitis: Lymphocytes
- Glucose mg%
- Normal individual: 40–70
- Pyogenic meningitis: < 40 mg/dL Decreased to absent
- Tuberculous meningitis: 20–40 mg/dL Slightly ↓
- Viral meningitis: Normal
- Total proteins mg%
- Normal individual: 15–45
- Pyogenic meningitis: > 45 mg/dL usually > 250 markedly ↑↑↑
- Tuberculous meningitis: 100–500 mg/dL moderate to markedly ↑↑
- Viral meningitis: 20–80 mg/dL Normal or slightly elevated
For example, in pyogenic meningitis, the markedly low glucose and high proteins reflect bacterial consumption and inflammatory response, as seen in cases of Streptococcus pneumoniae where prompt lumbar puncture aids diagnosis
Bloodstream Infections
Agents of endocarditis
- Agents of endocarditis:
- Streptococci Viridans streptococci and others
- Pneumococci
- Enterococci
- Staphylococcus aureus
- Coagulase-negative staphylococci e.g. Staphylococcus epidermidis
- Fastidious Gram-negative coccobacilli HACEK group
- Gram-negative bacilli
- Candida species
- Diphtheroids
- Culture-negative endocarditis: such as Bartonella, Coxiella
- Most common agent in specific types of endocarditis:
- Native valve endocarditis: Staphylococcus aureus
- Prosthetic valve endocarditis: It occurs following cardiac valve replacement
- Early prosthetic valve endocarditis occurs within 12 months of valve replacement: Staphylococcus epidermidis is the commonest agent
- Late prosthetic valve endocarditis occurs after 12 months of valve replacement: Viridans streptococci are the commonest agent
- Endocarditis in IV drug abusers: Young males are the most common victims. The skin is the commonest source of infection.
- Right sided: Most common agent is Staphylococcus aureus
- Left sided: Most common agent is Enterococcus followed by S.aureus
- Over all: Most common agent is Staphylococcus aureus
- MC cause of Subacute endocarditis: Viridans streptococci
For example, in IV drug users, Staphylococcus aureus targets the right heart valves due to direct bloodstream entry from skin, leading to complications like pulmonary emboli if untreated
Fever of Unknown Origin
- Petersdorf and Beeson classification 1961 was traditionally used for defining PUO.
- Temperatures of > 38.3°C >101°F
- For a duration of > 3 weeks; and
- Failure to reach a diagnosis despite 1 week of inpatient investigation.
- This classification has stood for more than 30 years, but later in 1990s, it was revised as Durack and Street classification. There after it is further modified in 2015. According to Harrison 19th edition, FUO is now defined as:
- Fever > 38.3°C 101°F on at least two occasions
- Illness duration of > 3 weeks
- No known immunocompromised state
- Diagnosis that remains uncertain after a thorough history-taking, physical examination and the obligatory investigations.
- Infections 36% accounts for majority of FUO cases followed by Neoplasms 19%.
For example, in FUO, persistent fever without clear cause might stem from hidden infections like tuberculosis, where extensive testing including imaging and biopsies is crucial for resolution
Other Infective Syndromes
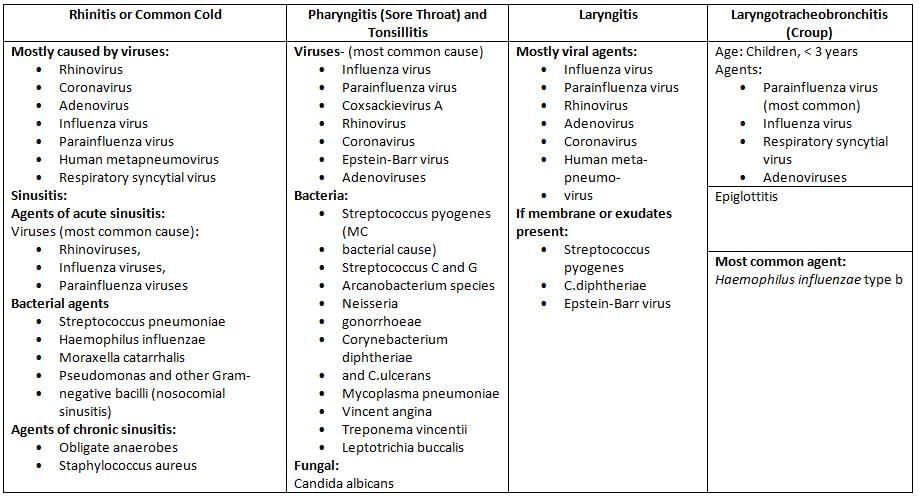
Microorganisms causing URTI (upper respiratory tract infections)
For example, in common cold caused by rhinovirus, the virus replicates in nasal epithelium leading to inflammation and symptoms like runny nose, demonstrating how viral attachment triggers immune responses without bacterial involvement
Comparison of STDs producing genital ulcer
- Feature: Incubation period
- Syphilis: 9–90 days
- Herpes: 2–7 days
- Chancroid: 1–14 days
- LGV: 3 days–6 weeks
- Donovanosis: 1–4 weeks up to 6 months
- Feature: Genital ulcer
- Syphilis: Painless, indurated, single
- Herpes: Multiple, painful
- Chancroid: Painful, soft
- LGV: Single or multiple Painful, soft
- Donovanosis: Painless
- Feature: Lymphadenopathy
- Syphilis: Painless, hard, moderate swelling no bubo
- Herpes: Absence or moderate swelling no bubo
- Chancroid: Painful, soft, marked swelling leads to bubo formation
- LGV: Painless
- Donovanosis: Absent pseudo bubo may be present due to subcutaneous swelling
For example, in syphilis, the painless chancre from Treponema pallidum allows unnoticed progression to secondary stages, underscoring the need for serological testing in at-risk populations
Congenital Infection
- Vertical transmission spread of infections from mother-to-baby may occur by transplacental route congenital infection, during labor and delivery, or after delivery.
- Congenital infection transmission from placenta to fetus: They often lead to defects in fetal development or even death.
- Examples include TORCH syndrome:
- Toxoplasmosis
- Other infections congenital syphilis, hepatitis B, Coxsackievirus, Epstein-Barr virus, varicellazoster virus, Plasmodium falciparum and human parvovirus
- Rubella
- Cytomegalovirus CMV
- Herpes simplex virus
- Perinatal infections during labor and delivery: CMV, Gonococcus, Chlamydia, HSV, HPV and Group B streptococci
- Postnatal infections after delivery: CMV, HIV and Group B streptococcus.
- For example, in TORCH infections like rubella, maternal infection during first trimester can cause congenital heart defects in the fetus, highlighting vaccination's role in prevention
Emerging and Re-Emerging Infection
- Emerging infection: Incidence in human increased in last two decades newly appearing disease or those spreading newly to a geographical area. Example include:
- Crimerian congo hemorrhagic virus in India Ahmedabad- Jan 2011
- Plasmodium knowlesi
- H1N1 -2009 and Avian flu H5N1-2005,
- SARS-2003 did not affect India
- HGV, HEV, HHV8, Sin Nombre
- Re-emerging infection: Incidence was brought down in past but again increased due to breakdown in public health measure including emergence of drug resistance
- India: Plague in Gujrat 1994, Chikungunya 2005, Dengue North, V.cholerae O139 south east costal
- MRSA, MDRTB, Leptospira South, Andaman
For example, SARS as an emerging infection rapidly spread globally in 2003 via travel, demonstrating how novel viruses can exploit modern connectivity, necessitating swift international surveillance
Bioterrorism and classification of bioweapons (CDC)
Bioterrorism is a form of terrorism unlawful use of weapon against mankind where there is intentional and deliberate release of biological agents bacteria, viruses, or their toxins to cause mass illness or death of people, animals, or plants
- Category A: Agents are the highest-priority pathogens which pose the greatest risk to national security
- Can be easily disseminated or transmitted from person to person
- Result in high mortality rates and have the potential for major public health impact
- Might cause public panic and social disruption
- Require special action for public health preparedness.
- Anthrax Bacillus anthracis
- Botulism Clostridium botulinum toxin
- Plague Yersinia pestis
- Tularemia Francisella tularensis
- Smallpox Variola major
- Hemorrhagic viruses
- Arenaviruses: Lassavirus
- Bunyaviridae: Crimean-Congo virus,
- Filoviridae: Ebola, Marburg virus
- Category B: These agents are the second highest priority pathogens
- Moderately easy to disseminate,
- Result in moderate morbidity rates and low mortality rates,
- Require specifically enhanced diagnostic capacity.
- Melioidosis Burkholderia pseudomallei
- Glanders Burkholderia mallei
- Brucellosis Brucella species
- Psittacosis Chlamydophila psittaci
- Q fever Coxiella burnetii
- Typhus fever Rickettsia prowazekii
- Toxin: Ricin, S.auerus Enterotoxin B, Epsilon toxin of Clostridium perfringens
- Viral encephalitis alphaviruses e.g., Venezuelan, eastern, and western equine encephalitis
- Food threats: Salmonella, Shigella, E.coli O157
- Water threats: Vibrio cholerae, Cryptosporidium
- Category C: These agents are the third highest priority pathogens. They are the emerging pathogens, to which the general population lacks immunity
- These agents could be engineered for mass dissemination in the future because of availability, ease of production, and ease of dissemination.
- They have a potential for high morbidity and mortality rates
- Nipah virus
- Hantavirus
- SARS coronavirus,
- Pandemic influenza virus
- MDRTB
- Yellow fever virus
For example, anthrax in Category A was used in 2001 letter attacks, causing inhalation disease with high fatality, illustrating how spore stability makes it ideal for bioterror, requiring vaccines and antibiotics for response
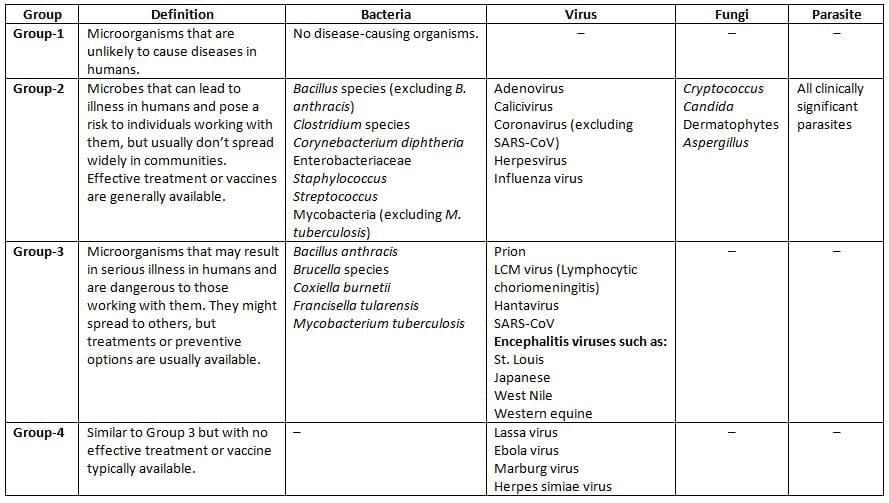
Risk-based classification of agents causing laboratory-acquired infections
Microbiological Profile of Osteomyelitis
- MC cause of osteomyelitis - S. aureus in all sites hematogenous long-bone and Vertebral and sternal. Harrison 19th/p838-844
- Sickle cell disease-Salmonella osteomyelitis is frequently cause
- IV drug users- P. aeruginosa is common Harrison 19th/p844
- Diabetic foot osteomyelitis - Polymicrobial MC is S. aureus followed by anaerobes and Gram negative like E.coli Harrison 19th/p845
- Implant associated osteomyelitis- Coagulase-negative staphylococci S. epidermidis are the second most common etiologic agents after S. aureus. Harrison 19th/p842
- Streptococcus agalactiae is common in children next to S. aureus
- Ref: Harrison 19th/p 838-844, Other Journals and e Books
- For example, in diabetic foot, polymicrobial involvement including anaerobes complicates healing due to poor circulation, often requiring debridement and targeted antibiotics
|
75 docs|5 tests
|
FAQs on Clinical Microbiology (Infective Syndromes) Chapter Notes - Microbiology - NEET PG
| 1. What are the most common microorganisms that cause urinary tract infections (UTIs) ? |  |
| 2. What could be the potential causes of fever of unknown origin (FUO) ? |  |
| 3. What are some common congenital infections, and how can they affect newborns ? |  |
| 4. What are the characteristics of emerging and re-emerging infections ? |  |
| 5. How can one differentiate between viral and bacterial infections in clinical microbiology ? |  |



















