Effects of Cold and Heat Chapter Notes | Forensic Medicine and Toxicology (FMT) - NEET PG PDF Download
| Table of contents |

|
| Introduction |

|
| Classification of Thermal Injury |

|
| Hypothermia |

|
| Hyperthermia (Hyperpyrexia) |

|
| Scalds |

|
| Death Due to Fire (Burns) |

|
Introduction
Thermal injury is damage to the body caused by extreme temperatures, either hot or cold. It can happen in various ways, and the body responds differently to these extreme conditions.
Normal Body Temperature
- The average normal body temperature is 98.6°F (36°C) when measured orally. However, this temperature can vary among individuals due to factors like age, the time of day, and physical activity levels.
- Maintaining a normal body temperature is crucial for health and involves balancing heat production with heat loss. Heat production comes from metabolic processes in the body, while heat gain can occur from the environment.
- Heat loss is essential to prevent overheating and occurs through three main methods: conduction, radiation, and evaporation.
Heat Loss by Evaporation
- Evaporation is a key method for heat loss and involves two mechanisms:
- Insensible Heat Loss: This occurs continuously as water molecules diffuse through the skin and lungs, regardless of the body’s temperature. It happens all the time, even when we are not aware of it.
- Heat Loss through Sweating: This is the more significant method of heat loss, especially in hot weather. Sweating helps cool the body by evaporating sweat from the skin’s surface. In cold weather, sweating is minimal, while in hot weather, it increases significantly to help regulate body temperature.
Classification of Thermal Injury
Thermal injuries are classified into various categories based on the nature of the injury and the temperature involved. Here’s a detailed breakdown:
1. Hypothermia
- Trench Foot: This condition occurs when the feet are exposed to cold, wet conditions for an extended period. The combination of cold and moisture can lead to damage in the tissues of the feet.
- Frostbite: Frostbite happens when skin and other tissues freeze due to extreme cold. It commonly affects extremities like fingers, toes, and the face.
2. Hyperthermia
- Heat Cramps: These are painful muscle contractions that occur during hot weather, often due to excessive sweating and loss of salt.
- Heat Prostration: Also known as heat exhaustion, this condition results from prolonged exposure to high temperatures, leading to symptoms like weakness, dizziness, and nausea.
- Heat Hyperpyrexia: This is a severe form of hyperthermia where the body temperature rises to dangerous levels, potentially leading to heat stroke, which is a medical emergency.
3. Injury from Heated Solid Objects
This type of injury occurs when the skin comes into contact with hot solid objects, leading to burns. The severity of the burn depends on the temperature of the object and the duration of contact.
4. Flame Burns: Dry Heat
Flame burns occur when the skin is exposed to open flames or hot gases. These burns can penetrate deep into the skin and cause severe damage.
5. Scalds: Moist Heat
Scalds are caused by contact with hot liquids or steam. The severity of a scald depends on the temperature of the liquid and the duration of contact with the skin.
6. Chemical Burns
Chemical burns result from exposure to corrosive substances such as acids, alkalis, or other hazardous chemicals. These burns can cause deep tissue damage and require immediate medical attention.
7. Corrosive Burns
Similar to chemical burns, corrosive burns occur due to contact with substances that can corrode or destroy body tissues. This can happen through skin contact, ingestion, or inhalation.
8. Radiation Injury
Radiation injuries occur due to exposure to harmful levels of radiation, which can damage skin and underlying tissues. This type of injury is not as common but can occur in specific environments, such as nuclear facilities or during certain medical treatments.
9. Electrical Injury: Electrocution, Lightning
- Electrocution: This occurs when a person is exposed to a significant electrical current, leading to burns and potential damage to internal organs.
- Lightning Strikes: Being struck by lightning is a rare but severe form of electrical injury that can cause burns, cardiac arrest, and other serious health issues.
10. Frictional Heat
Frictional heat injuries occur when skin is subjected to friction, leading to burns. Common examples include:
- Corns: Thickened skin on the feet due to prolonged pressure and friction.
- Shoe Bites: Injuries caused by friction from ill-fitting shoes.
- Brush Burns: Burns caused by skin rubbing against rough surfaces.
- Rope Burns: Injuries caused by friction from a rope rubbing against the skin.
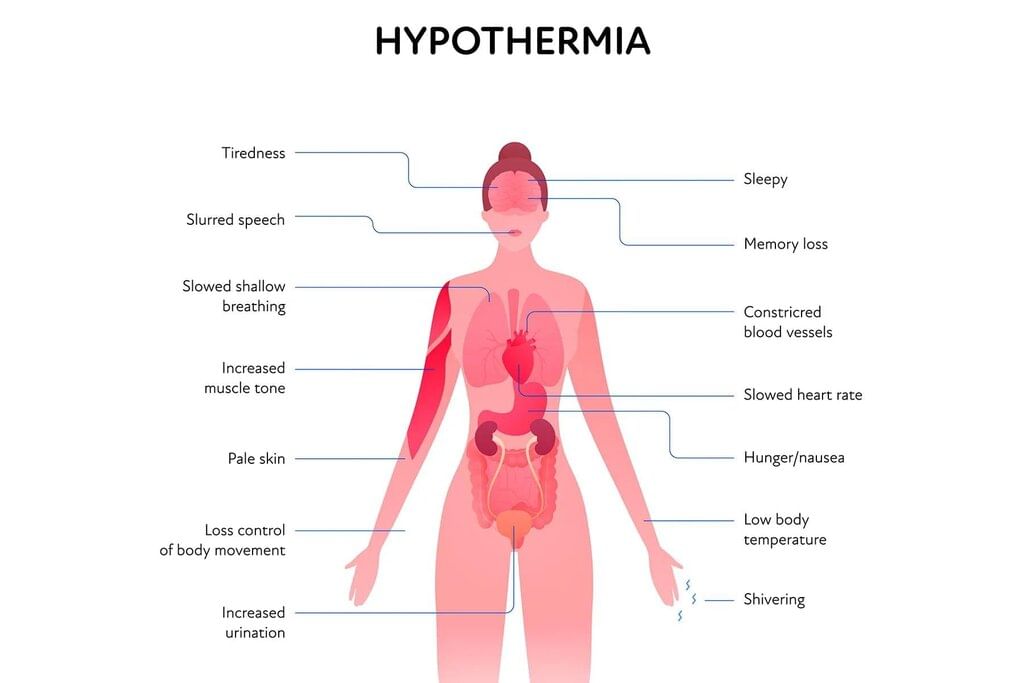
Hypothermia
Hypothermia occurs when the body's temperature drops below 95°F (35°C). This happens when the body loses heat faster than it can produce it. Hypothermia is significant in both medical and legal situations, as many people experience it, especially during winter in mild climates. It primarily affects the extremities and exposed areas like the face. Hypothermia can be further classified into different types, including:
Trench Foot
Trench foot is caused by exposure to cold temperatures, typically between 5-8°C, combined with damp conditions. Importantly, trench foot does not involve the freezing of tissue, and it does not result in permanent damage.
Frostnip and Frostbite
- Frostnip and frostbite are conditions caused by exposure to temperatures below 0°C, leading to freezing of body tissues.
- Initially, when the skin is exposed to extreme cold, there is numbness and tingling without immediate tissue damage. The body’s blood vessels constrict, causing the skin to change color, becoming white, waxy, or grey, and appearing mottled, although it feels normal to the touch. This early stage is known as frostnip.
- If frostnip is not treated, it can progress to frostbite. In frostbite, ice crystals begin to form in the skin and deeper tissues. This process creates an osmotic force that pulls water out of the cells, leading to edema, which is the accumulation of fluid in the spaces between cells. At the same time, the cells become dehydrated, resulting in high osmolarity.
- Additionally, proteins in the cells denature, and enzymes are destroyed. As the condition worsens, the skin becomes numb and discolored, often turning purple. When touched, the affected skin loses its normal elasticity, feeling hard, like a rock, a block of ice, or frozen meat. Blisters may also form, and in severe cases, these blisters can become hemorrhagic, indicating bleeding within the blisters.
Incidence
- The primary cause is exposure to low temperatures.
- Exposure often results in hypothermia, which is a severe condition.
- Frostbite is common among soldiers during winter warfare, particularly in trenches, and among those stranded in shipwrecks in Antarctic waters.
- Numerous fatalities among climbers, outdoor workers, swimmers, and athletes are due to cold exposure.
- Another at-risk group includes intoxicated individuals, who may collapse or fall asleep due to alcohol consumption, increasing the risk of hypothermia.
- Alcohol induces vasodilatation of the skin, resulting in increased heat loss.
- Accidental hypothermia can affect people who become lost while hiking or skiing, or those immersed in ice-cold water in regions like the Himalayas, North Bihar, Uttar Pradesh, and Kashmir.
- In marine disasters, hypothermia can be as prevalent a cause of death as drowning, or it may lead to drowning in survivors who can swim or cling to wreckage.
- Death in such cases can occur within minutes due to rapid heat loss.
- According to Bernard Knight, the majority of hypothermia-related deaths among civilians involve elderly individuals and children.
- In some elderly people, hypothermia may be linked to a peculiar psychiatric condition where they hide in corners, cupboards, or under furniture.
- These individuals are often found undressed, raising concerns of criminal victimization.
- This 'hide-and-die syndrome' is well-recognized; it is unclear whether the person becomes hypothermic first and then confused, or vice versa, leading to hypothermia.
Factors that Modify the Effects of Cold
- Age: Adults generally cope with cold better than infants and the elderly. Children lose heat rapidly because of their larger body surface area relative to their weight. Infants are particularly vulnerable to hypothermia if left in cold rooms during winter due to neglect or family circumstances.
- Duration of Exposure: The severity of cold effects increases with the length of exposure due to ongoing heat loss.
- Bodily Condition: Factors such as fatigue, exhaustion, intoxication, and starvation can accelerate the impact of cold on the body.
- Thyroid Deficiency: The severity of thyroid deficiency, including conditions like clinical myxoedema, can result in lower body temperatures and a heightened risk of hypothermia.
- Medication: The use of phenothiazine drugs can increase the susceptibility to hypothermia.
Pathophysiology of Cold
When a healthy individual is exposed to extreme cold, several physiological changes occur:
- There is a decrease in heart rate and respiration.
- Tissue respiration is impaired due to the difficulty in releasing oxygen from hemoglobin, leading to insufficient oxygen supply.
- Body metabolism is lowered.
- Enzymatic processes in the body slow down.
- There is a drop in body temperature, which can cause essential functions to cease.
In response to extreme cold, the body exhibits vasoconstriction of surface blood vessels, resulting in skin numbness and significant discomfort. This discomfort may trigger a behaviour known as paradoxical undressing, where individuals feel an urge to remove clothing.
Paradoxical Undressing
Paradoxical undressing is a strange behavior often seen in people suffering from hypothermia, where they mistakenly remove their clothing despite being extremely cold.
- When a person is exposed to extreme cold, their body reacts by trying to protect itself. One of the ways it does this is by redirecting blood away from the extremities, like the hands and feet, and towards the warm core of the body.
- This process, known as vasoconstriction, reduces blood flow to the outer parts of the body in order to safeguard vital organs.
- By keeping blood closer to the core, the body can retain heat more effectively as hypothermia worsens.
- As a result of this redirection, the hands and feet often become the first areas to feel cold.
However, in the early stages of hypothermia, the body may experience a false sense of warmth due to the initial cold shock response. This can lead to confusion and impaired judgment, a state sometimes referred to as "cold stupid" in mountaineering.
- Paradoxical undressing occurs when individuals in this state feel an overwhelming urge to remove their clothing, despite the fact that they are freezing.
- This behavior is a result of the body’s impaired ability to recognize and respond to the extreme cold it is experiencing.
What Leads to Paradoxical Undressing?
- Vasoconstriction is the process where the smooth muscles in blood vessels tighten, requiring energy from glucose stored in the body.
- Eventually, when blood flow to these muscles decreases, they become fatigued.
- As the energy in the constricted blood vessel muscles depletes, they relax and open up, a process known as vasodilatation.
- During vasodilatation, warm blood from the body’s core rushes into the extremities, such as the hands and feet.
- This sudden influx of warm blood can create a sensation of heat in a person suffering from hypothermia, prompting them to remove their clothing, even though their core body temperature is still declining.
- The combination of warm blood moving outward and the act of shedding clothing accelerates the decrease in body temperature.
- This dangerous cycle increases the risk of death from hypothermia and contributes to more instances of paradoxical undressing.
- Individuals with hypothermia may also exhibit behaviors such as pushing away warm clothing and resisting assistance.
- Unfortunately, most victims of hypothermia who experience paradoxical undressing do not survive without intervention.
- Paralysis of the blood vessels’ control can lead to thrombosis, capillary dilation, and blood stagnation, resulting in tissue damage known as frostbite.
- Damage to the capillary lining increases permeability, leading to transudation and oedema.
Frostbite
Frostbite refers to the localized death of tissue, commonly impacting soldiers in cold conditions, such as during winter battles in trenches or after shipwrecks in frigid Antarctic waters.
Vasospasm involves the loss of control over blood vessel movement, leading to potential complications.
Clinical Findings
- The skin appears extremely cold with red patches on exposed areas like the ears, nose, fingers, and toes.
- Muscle stiffness may be observed.
- There might be a weak pulse along with a slow heart rate and low blood pressure.
- Reflexes could be diminished.
- Individuals may experience lethargy, heaviness, and drowsiness.
- In severe instances, symptoms can escalate to stupor, confusion, coma, and death due to inadequate oxygen supply to tissues, which struggle to release oxygen from oxyhaemoglobin.
Treatment
- Gently warm the body by placing the victim on a warm bed.
- Provide hot water fomentation and warm drinks.
- Administer oral stimulants like caffeine or specific medical stimulants.
- Give warm saline through an intravenous line.
Postmortem Findings
- Skin: Pale with uneven dark red patches on exposed areas.
- Brain: Congested, with ventricles filled with serum.
- Heart: Full of blood on both sides.
- Pancreas: Microscopic examination may show fat necrosis.
Medicolegal Significance
- Suicide due to cold exposure is highly unlikely.
- The majority of deaths resulting from cold exposure are:
- Accidental deaths, commonly observed in individuals with alcoholism who fall asleep in the snow or in people who become lost in snowdrifts.
- Homicidal cases, such as instances where unwanted newborns or elderly individuals are deliberately left exposed to harsh cold conditions.
- The phenomena of 'Paradoxical undressing' and 'Hide-and-die syndrome' may raise suspicions of a sexual offence against the victim, particularly in cases involving female victims.
Hyperthermia (Hyperpyrexia)
Hyperthermia is a severe condition that occurs when the body absorbs or produces more heat than it can dissipate. This often results from excessive heat exposure. Hyperpyrexia specifically refers to an extremely high body temperature, typically exceeding 41.1°C (106°F). In such cases, the body's temperature regulation system becomes overwhelmed, leading to a hazardous increase in body heat. This situation is critical and requires immediate medical intervention. In extreme instances, hyperthermia is referred to as heat stroke or sunstroke. Heat stroke can escalate rapidly but usually follows a less severe condition known as heat exhaustion or heat prostration.
Progression
Body temperatures exceeding 40°C. 104°F. are life-threatening. This is compared to a normal body temperature of 36-37°C. 97-98°F). At high environmental temperatures, brain damage can occur, but brain death is determined through neurological assessments, not just temperature. At 41°C. 106°F), there is a risk of brain damage, and at 45°C. 113°F), death is nearly certain. Internal temperatures above 50°C. 122°F. will cause muscle rigidity and immediate death.
Trauma and death from hyperthermia can result from exposure to heat, which can come from:
- Natural sources, such as heat from the sun.
- Artificial sources, like industrial furnaces and large baking ovens.
- Poorly ventilated or closed spaces, such as factories with high temperatures and humid air.
Three conditions may arise due to high environmental temperatures:
- Heat cramps —no increase in body temperature.
- Heat prostration —lower than normal body temperature.
- Heat hyperpyrexia —rectal temperature above 41 degrees.
Predisposing Factors
- Malnourishment
- Overexertion
- Fatigue
- Chronic alcoholism, hunger, lack of sleep, etc.
- Mental depression
Pathophysiology of Hyperthermia
- Hyperthermia can cause a range of problems from heat cramps and simple exhaustion to fainting and severe conditions like coma.
- In severe cases, it can lead to respiratory and cardiac failure, which could be fatal.
- The body regulates its temperature mainly through perspiration.
- Perspiration helps remove heat from the body, allowing it to escape through radiation or convection.
- When sweat evaporates, it cools the body further by absorbing heat.
- Initially, a person affected by hyperthermia will sweat a lot, leading to dehydration.
- As dehydration worsens, the body stops producing sweat, which stops heat loss.
- When sweating stops, the core body temperature increases rapidly.
Signs and Symptoms of Heat Prostration or Heat Exhaustion
Initial Symptoms:
- Mental confusion
- Muscle cramps
- Nausea or vomiting
Rising Body Temperature:
- Continued exposure can raise body temperature to dangerous levels between 39 to 40°C (103 to 104°F), risking heat stroke.
Altered Mental State:
- Victims may become confused, aggressive, or have headaches.
- They might also appear intoxicated.
Blood Pressure and Heart Rate:
- Blood pressure may drop significantly due to dehydration, leading to fainting and dizziness, especially when standing.
- Heart rate (tachycardia) and breathing rate (tachypnoea) increase as blood pressure falls.
Skin Changes:
- Initially, the skin may turn red as blood vessels widen to release heat.
- As heat stroke progresses, skin may become pale or bluish.
Feeling Hot and Subsequent Chills:
- Victims may feel hot initially, followed by chills and trembling, resembling a fever.
Convulsions in Young Children:
- Some young children may experience convulsions.
Severe Dehydration Effects:
- Nausea and vomiting
- Temporary blindness
Organ Failure:
- Can lead to unconsciousness and coma.
Clinical Manifestations of Heat Exposure
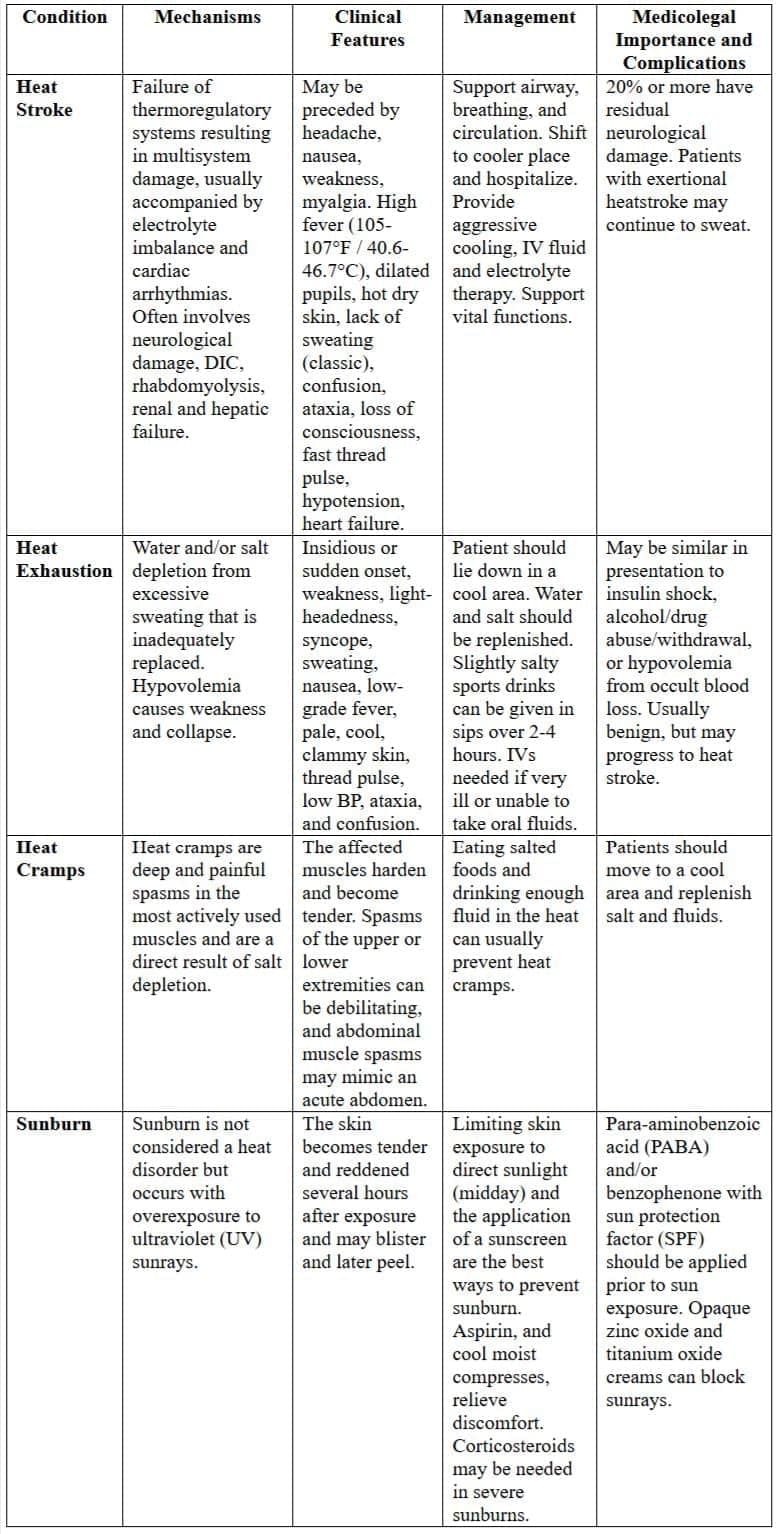
Exposure to elevated temperatures can result in various effects, which are broadly categorized into three main types: heat cramps, heat exhaustion, and heat stroke.
Heat Cramps
- Intense and painful spasms in voluntary muscles may occur.
- This condition is triggered by excessive sweating and electrolyte loss following vigorous activity in hot conditions.
- The mortality rate associated with heat cramps is virtually nonexistent.
Heat Exhaustion: Understanding the Impact on the Circulatory System
Heat exhaustion primarily affects the circulatory system and is characterized by a series of symptoms resulting from peripheral vascular collapse. This condition leads to poor venous return, causing several noticeable effects on the body.
- Peripheral Vascular Collapse: The body’s blood vessels, especially those in the periphery, struggle to maintain proper blood flow.
- Pallor: The skin becomes pale due to the inadequate return of blood to the heart, affecting circulation.
- Hypotension: Blood pressure drops as a result of poor venous return, leading to insufficient blood flow to vital organs.
- Flushing of the Face: Despite the overall pallor, the face may appear flushed. This is often accompanied by throbbing temples and scanty perspiration.
Fortunately, most patients experiencing heat exhaustion typically recover without severe complications, and fatalities are extremely rare.
Heat Stroke: A Life-Threatening Condition
Heat stroke represents a critical failure of the body’s heat regulation system and can be fatal due to the paralysis of the brain's control centers. This condition manifests in two distinct forms:
- Acute Form: Sudden onset without prior warning symptoms.
- Gradual Onset Form: Develops slowly with early warning signs.
Early Symptoms
In the gradual onset form, individuals may experience early symptoms such as:
- Headache
- Nausea
- Vomiting
- Dizziness
- Weakness in the legs
- Strong urge to urinate
Signs of Heat Stroke
- Sudden Unconsciousness: Collapse and loss of consciousness.
- Facial Symptoms: Flushed face, initially dilated pupils that later become constricted (pinpoint), and congested conjunctiva.
- Skin: Hot and dry with no sweating.
- Cardiovascular System: Full, bounding, and rapid pulse.
- Respiratory System: Laboured and rapid breathing.
- Body Temperature: 43°C or higher, known as heat hyperpyrexia.
- Central Nervous System: Delirium and convulsions may occur.
Potential Outcomes
Heat stroke can lead to severe consequences, including death, due to the paralysis of the hypothalamus, which is responsible for regulating body temperature. Immediate medical intervention is crucial in such cases to prevent fatal outcomes.
Treatment
First Aid for Heat Stroke
- Heat stroke is a severe medical condition that requires immediate hospital care, so it's crucial to contact local emergency services right away.
- Rapidly reducing the body temperature is essential, and both passive and active cooling methods can be effective.
Passive Cooling
- Move the individual to a cooler environment, either indoors or in a shaded area.
- Remove their clothing to facilitate heat loss.
Active Cooling
- Immerse the person in cool water.
- Use a hyperthermia vest or wrap them in a cool, damp towel.
- Apply cold compresses to the torso, head, neck, and groin to aid in cooling.
- Utilize a fan to enhance evaporation and further cool the person.
- Avoid using ice or very cold water without medical guidance, as it may induce shock.
- Immersing a victim in a bathtub of cold water is an accepted cooling method, typically requiring 4-5 people for assistance and close monitoring of the victim.
- This method should not be used on an unconscious person; if necessary, keep their head above water.
Hydration
- Hydration is essential for cooling the patient, and this can be achieved through oral rehydration by drinking water.
- In specific cases of dehydration, commercial isotonic drinks may be used, but improper use can lead to complications.
- Alcohol and caffeine should be avoided as they can contribute to dehydration.
- Some experts recommend against providing fluids, except when administered by emergency personnel.
- Intravenous hydration via a drip is necessary if the patient is confused, unconscious, or unable to drink fluids.
- The patient’s condition should be reassessed and stabilized by trained medical personnel.
- Continuous monitoring of the patient’s heart rate and breathing is crucial, and CPR may be required in case of cardiac arrest.
- The patient should be placed in the recovery position to maintain an open airway.
Prevention
- Avoid overheating and dehydration:
- Wear light, loose-fitting clothing: Choose clothes that allow sweat to evaporate, helping your body stay cool.
- Use wide-brimmed hats: Opt for brightly coloured hats with vents to protect your head and neck from the sun and help keep you cool.
- Avoid vigorous exercise during hot daylight hours: Refrain from intense physical activity when it's hottest outside.
- Be mindful of humidity: High humidity can make it feel much hotter than it is, so be cautious in such conditions, especially in direct sunlight.
- Drink plenty of liquids: In hot weather, replace fluids lost through sweating by drinking enough liquids. Don't rely solely on thirst to gauge your need for fluids; instead, pay attention to the colour of your urine. Dark yellow urine is a sign of dehydration. While drinks like alcohol, tea, and coffee can have a diuretic effect, they still contribute to hydration, though not as effectively as water. Pure water is the best choice for staying hydrated.
Susceptible Populations
Hyperthermia can affect anyone, but certain groups are particularly at risk for heat-related illnesses and injuries. These include low-income individuals, city residents, young children, people with chronic physical or mental health conditions, substance users, older adults, and those engaging in intense physical activity in extreme conditions.
Medicolegal Significance
- Hyperthermia can be deliberately induced for medical purposes, known as thermotherapy, using drugs or medical devices.
- It is sometimes employed in cancer treatment to target and destroy or weaken tumor cells while sparing healthy tissue.
- Malignant hyperthermia is a rare but serious complication associated with certain types of general anesthesia.
- Deaths from hyperthermia are typically accidental, often occurring in hot, humid environments, though they may rarely be suicidal or homicidal.
- Workplace conditions causing hyperthermia in employees may lead to liability under the Workmen’s Compensation Act.
- Homicides disguised as heatstroke, involving substances like belladonna, atropine, or cocaine, have been documented.
- In cases of sunstroke, individuals may enter a state of suspended animation, so resuscitation efforts should be attempted before declaring death.
Postmortem Findings in Hyperthermia
- Postmortem Caloricity. The body temperature remains elevated after death, contrasting with the usual postmortem cooling process.
- Eye Changes. Sinking and pitting of the eyeballs may occur, resembling alterations seen in evolutionary processes.
- Rigor Mortis. This phenomenon sets in rapidly and resolves more quickly than normal.
- Postmortem Stains. These stains are prominent due to increased blood fluidity.
- Putrefaction. The process of putrefaction occurs swiftly.
- Cerebral Degeneration. Changes in the cerebral cortex, cerebellum, and basal ganglia are commonly observed.
- Visceral Congestion. Congestion is often evident throughout the entire viscera.
- Blood Testing for Alcohol Levels. Blood may be preserved for testing alcohol levels, as excessive alcohol consumption can trigger fatal episodes.
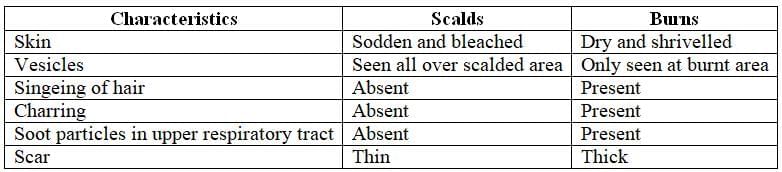
Scalds
Scalds are injuries caused by contact with moist heat, typically affecting only the outer layers of the skin.
Scalds occur when the skin comes into contact with moist heat, which can cause damage to the outer layers of the skin. The mechanism involves the transfer of heat from the hot liquid or steam to the skin, leading to various degrees of injury depending on the temperature and duration of contact.
Causes of Moist Heat
- Hot water, oil, or any liquid at or near boiling point.
- Superheated industrial steam.
Clinical Features
Scalded skin typically appears swollen, blistered, and pale. The effect is less severe in areas covered by clothing, as it cools more quickly. The heat from moist sources spreads from the point of contact, causing the most damage at the initial site and decreasing as it disperses. Clinically, scalds are categorized into three degrees:
- Erythema: Immediate reddening of the skin upon contact with moist heat.
- Vesication: Blister formation due to increased capillary permeability, developing a few minutes after exposure. Blisters are often surrounded by a red, inflamed area, and removing them reveals a pink, raw surface.
- Necrosis of the Dermis: Occurs when deeper skin layers are affected, resulting in thinner scars with minimal contraction and disfigurement upon healing.
Medicolegal Significance
- Scalds are typically accidental, often occurring during cooking or bathing, especially among children and the elderly.
- Boiling water may be intentionally thrown with harmful intent.
- Deliberate scalding is a common form of child abuse.
- Suicidal or homicidal scalding is extremely rare.
- Distinguishing between scalds (moist heat) and dry heat burns is sometimes necessary.
Summary of mechanisms, clinical features, management and medicolegal Importance and complications of hyperthermia
 Scalds of the left thigh
Scalds of the left thigh
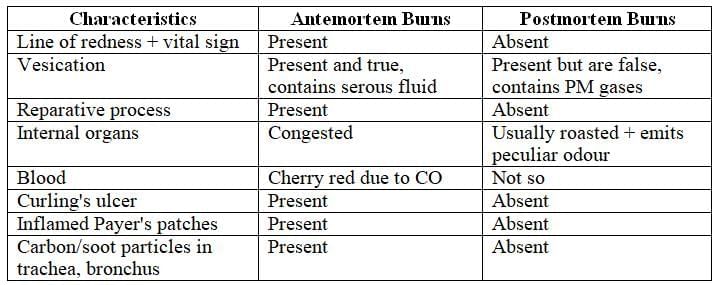
Differences between antemortem and postmortem scald
- Line of redness: Present (+ve) in antemortem scalds, absent (-ve) in postmortem scalds.
- Vesicle content: Contains albuminous material (+ve) in antemortem scalds, contains gas/air (-ve) in postmortem scalds.
- Infection: Possible (+ve) in antemortem scalds, absent (-ve) in postmortem scalds.
Death Due to Fire (Burns)
In India, there are thousands of deaths each year resulting from fire or burns. Most of these incidents occur at home and are caused by:
- Smoking
- Faulty electrical wiring
- Faulty kerosene stove explosions
- Self-immolation
- Homicidal burns, often related to dowry deaths or bride burning by husbands or in-laws
Definition
Deaths caused by fire or burns typically occur when dry heat is applied to the body.
Incidence of Burns
- Burns can occur due to various incidents, including:
- A building catching fire
- Explosions involving flammable liquids
- Burns from industrial furnaces
- Clothing catching fire
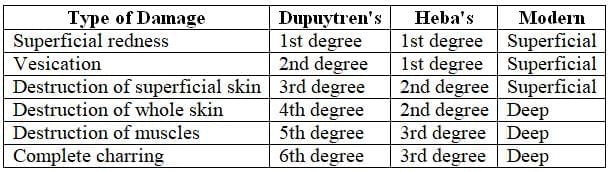
Classification of Burns
- There are three widely accepted systems for classifying burns:
- Dupuytren’s classification
- Heba’s classification
- Modern classification
Effects of Burns
- In severe burns, both stages of the Modern classification can often be seen together.
- Burns caused by dry heat tend to show more noticeable scarring, especially when the dermis is affected.
- When burns only involve the epidermis, they usually heal without leaving scars.
- Keloid formation is more common with corrosive burns.
- Curling’s ulcer is a rare complication of severe burns that affects the gastrointestinal tract, particularly in cases of stress-related mucosal disease. This condition results from tissue hypoxia and damage to the capillary endothelium. Dr. T.B. Curling first described it in 1842.
Factors Modifying Effect of Burns
- Intensity: The severity of the effects increases with higher intensity.
- Duration of Exposure: The longer the duration of exposure, the more severe the effects will be.
- Depth of Burn: The depth of burn injuries is crucial as it determines the severity of tissue damage. This is especially important if the burn affects the oxygen supply to the fingers and toes or causes difficulties with chest expansion and breathing.
- Types of Burns: Depending on the skin and its structure, burns can be classified into three types:
- Superficial Burns
- Partial Thickness Burns
- Mid-Dermal
- Deep-Dermal
- Full-Thickness Burns
Superficial Burns
- These burns are typically red, moist, and quite painful.
- They affect the epidermis, which is the outermost layer of skin, and may cause blisters.
- Healing usually occurs within 7 to 10 days with minimal or no scarring.
Partial Thickness Burns
- Mid-dermal: In this type of burn, the outer layer of skin is damaged, along with portions of the dermis, which is the layer beneath the epidermis.
- The affected area appears pink with small white patches.
- The skin remains painful and blanches (turns white) when pressed.
- Healing can take 7 to 14 days, depending on the extent of skin damage.
- There may be some mild pigmentation changes or scarring after healing.
- Deep-dermal burns: These burns involve deeper layers of the dermis.
- The burn site appears white and does not blanch when pressed.
- The skin in these areas is less sensitive and takes a longer time to heal, often resulting in significant scarring.
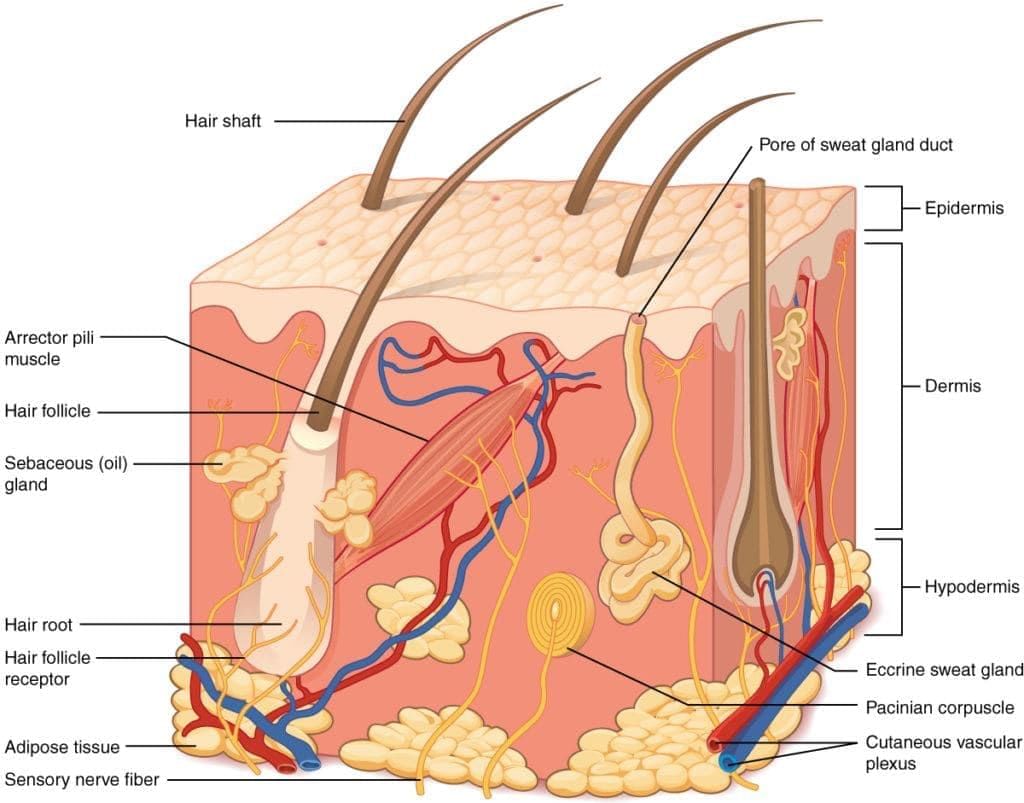 Skin and its morphology presenting the structures in its depth
Skin and its morphology presenting the structures in its depth
Differences between scalds and burns
Differences in classification of burns
Full Thickness Burns
- These burns penetrate deep into the dermis, resulting in a leathery texture. The coloration can range from white to grey or black.
- Surprisingly, full thickness burns are not painful because there is a loss of sensation in the affected area. When pressed, the skin does not turn white, indicating the severity of the injury.
- Healing occurs slowly, starting from the edges of the surrounding skin. Unfortunately, this type of burn often leads to scarring and contracture, where the skin tightens as it heals.
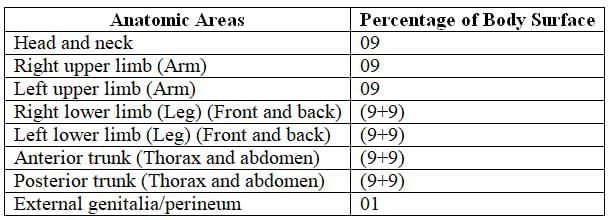
Extent of Body Surface Area (BSA)
- The extent of the burn on the body surface area is crucial in determining the severity and treatment of the burn.
- Clinicians use the rule of nines to assess the extent of burns. This method divides the body into sections, each representing 9 percent of the total body surface.
- When more than 20 percent of the surface area is affected, it leads to significant fluid loss and shock. Involvement of 30 to 50 percent can be fatal.
Lund and Browder Chart
- The Lund and Browder chart is specifically used for children and takes age into account when calculating body surface area affected by burns.
Rule of Nines for Adults
- The rule of nines is applicable to adults and is not suitable for infants due to their different body proportions.
Recent Developments
- Recent advancements include computer software that provides colour-coded calculations for burn assessment and an instant resuscitation guide.
Percentage of body surface area involved in burns (Rule of nine)
Factors Affecting Severity of Burns
- Site of the Body: Burns on the trunk, lower abdomen, and genitalia are more likely to be fatal due to the vital organs and structures in these areas.
- Age of the Patient: Older individuals are at a higher risk of fatality from burns compared to children and younger adults. This is because older adults may have weaker skin, underlying health issues, and a decreased ability to recover from traumatic injuries.
- Sex of the Patient: There may be differences in how men and women respond to traumatic injuries like burns. Factors such as hormonal differences, body composition, and overall health can influence the outcomes. For instance, women might have different pain thresholds or healing responses, though more research is needed to fully understand these differences.
Causes of Death in Burns
Death in burn cases can occur either within the first 48 hours or after that, and the causes can be classified accordingly.
Death Occurring within Few Hours
In the initial hours after a severe burn, death may result from shock, coma, or asphyxia. Each of these causes is explained below:
Shock:
- Primary neurogenic shock can occur due to factors like fear, intense pain, or injury to vital organs. This type of shock can lead to death within 24 to 48 hours.
- Secondary (vascular) shock is caused by the loss of serum from the burnt area, leading to a decrease in blood volume and resulting in hypovolemic shock. This too can be fatal within a similar timeframe.
Coma:
- Coma can occur due to congestion in the brain and significant fluid accumulation in the brain's ventricles.
Asphyxia:
- Asphyxia may result from inhaling smoke or toxic gases during a fire. It can also be caused by external pressure on the chest from collapsing structures such as roofs, beams, or walls.
Death Occurring within Few Days
The victim may die due to inflammation of internal organs, gangrene, exhaustion, septic absorption, toxaemia, and hepatorenal syndrome. Each of these is discussed individually:
Inflammation of Internal Organs:
- Inflammation can lead to conditions such as meningitis, peritonitis, pneumonia, bronchitis, pleurisy, enteritis, and Curling’s ulcer in the duodenum.
Gangrene:
- Complications can arise from ulcers caused by burns, including gangrene, erysipelas, tetanus, and significant hemorrhage when slough separates.
Exhaustion:
- Exhaustion occurs due to severe pain and dehydration from fluid loss.
Septic Absorption:
- Sepsis can develop from excessive suppuration, leading to potential death within 5 to 6 weeks or longer. Pseudomonas is the most common organism responsible for infection and sepsis.
Toxaemia:
- Toxaemia results from the absorption of histamine, which forms when tissue burns.
Hepatorenal Syndrome:
- In all cases of burns, regardless of severity, absorption of altered proteins occurs, causing cellular damage to the liver and kidneys (acute tubular necrosis). The heart may also be affected.
Postmortem Appearances of Burns
General Observations: Burn marks will be present in both antemortem and postmortem burns. However, signs of antemortem burns, such as vital reactions, indicate that the burns contributed to the cause of death.
External Examination:
- Clothing: Carefully remove and inspect for traces of flammable substances like kerosene or petrol.
- Personal Items: Preserve items such as keys, rings, or ornaments for identification purposes.
- Face: Often appears swollen, distorted, with the tongue protruding.
- Skin: The appearance varies based on the burn source:
- Radiant heat: Whitish skin.
- Heated solid objects:
- Brief contact: Blisters and redness matching the object’s shape.
- Prolonged contact: Roasting or charring.
- Explosions (e.g., coal mines or gunpowder): Blackening and tattooing of skin.
- Kerosene burns: Distinctive odor with sooty blackening.
- Antemortem burns: Show a line of redness (hyperemia) as a vital reaction.
- Cuticular peeling: May result in degloving or destocking.
- Hair: Singeing causes hair to curl, become brittle, and show vacuoles under microscopic examination.
- Pugilistic Attitude (Boxer’s or Fencing Attitude): The body adopts a rigid, flexed posture resembling a defensive stance.
- Features: Flexed limbs, closed fists, forward-bent body, and tense, leathery skin with potential splitting.
- Cause: Heat causes muscle protein coagulation, leading to contraction.
- Medicolegal Significance: This posture may occur in both antemortem and postmortem burns. In charred bodies, it may be mistaken for a defensive reaction against an attacker. Cracks or fissures resembling incised wounds may align with exposed blood vessels.
- Charring: The extent depends on the degree of postmortem burning.
Internal Examination:
- Skull: Intense heat may fracture or burst skull bones along sutures.
- Brain and Meninges: Congested, with extravasated blood giving the dura mater a brick-red color (heat hematoma). The brain may appear shrunken.
- Larynx, Trachea, and Bronchi: Contain soot and carbon particles with congested mucosa and frothy secretions, indicating antemortem burns due to smoke inhalation causing suffocation or asphyxia.
- Pleura: Congested, inflamed, with serous effusion.
- Lungs: Congested and edematous.
- Heart: Chambers filled with cherry-red blood due to carbon monoxide inhalation.
- Stomach and Intestines: Stomach mucosa may be carbon-impregnated or red. Inflammation or ulceration may occur in Peyer’s patches or intestinal glands. Curling’s ulcers in the duodenum may develop 7–10 days post-burn due to liver-derived irritants causing thrombosis in small vessels.
- Spleen: Enlarged and softened.
- Liver: Shows cloudy swelling or cellular necrosis in delayed deaths.
- Kidneys: Exhibit nephritis, with straight tubules containing blood cell debris, appearing reddish-brown.
Differences between Antemortem and Postmortem Burns
Medicolegal Importance
- Identification of the Deceased: Identifying a completely burnt body is challenging, but certain clues can assist:
- Metallic Objects: Items like rings, bangles, or keys on the body may survive the fire and aid identification.
- Sex Determination: The prostate gland and a nulliparous uterus are resistant to high temperatures and can indicate the deceased’s sex.
- Age Estimation: Teeth and bone ossification patterns can help determine the age of the deceased.
- Antemortem vs. Postmortem Burns: Differences between burns sustained before or after death.
- Burns as Cause of Death: Two key indicators confirm burns as the cause of death:
- Presence of soot or carbonaceous particles in the respiratory tract, mixed with mucus.
- Cherry-red blood discoloration due to carboxyhemoglobin.
- Nature of Burns (Suicidal, Accidental, or Homicidal):
- Suicidal Burns: Common among Indian women, often involving kerosene and self-immolation. Some may stuff cloth in their mouths to muffle cries.
- Accidental Burns: Frequently occur among children and the elderly, often due to incidents like kerosene stove explosions.
- Homicidal Burns: Prevalent in India, particularly linked to dowry disputes among certain Hindu communities. Young women may be killed by being doused with kerosene and set alight, with perpetrators claiming it was accidental. This practice, known as dowry deaths or bride burning, has prompted India’s Home Ministry to mandate that postmortem examinations of married women dying under suspicious circumstances (within 7 years of marriage or under age 30) be conducted by a panel of two doctors (IPC, Section 304B).
- Self-Inflicted Burns for False Accusations: Such burns are typically found on easily accessible body parts.
- Spontaneous or Preternatural Combustion: Rare claims of burns caused by ignition of flammable intestinal gases (e.g., hydrogen sulfide, methane) have been reported but are now widely dismissed as myths.
- Burning to Conceal Homicide: Bodies may be burned postmortem to hide evidence of murder, with head injuries and neck compression being common methods of homicide.
|
76 docs|3 tests
|
FAQs on Effects of Cold and Heat Chapter Notes - Forensic Medicine and Toxicology (FMT) - NEET PG
| 1. What are the main differences between frostnip and frostbite? |  |
| 2. What is trench foot and how does it develop? |  |
| 3. How does paradoxical undressing occur in cases of severe hypothermia? |  |
| 4. What factors can modify the effects of cold on the human body? |  |
| 5. What are the causes and pathophysiology of frostbite? |  |














