Herpesviruses and Other DNA Viruses Chapter Notes | Microbiology - NEET PG PDF Download
| Table of contents |

|
| Herpesviruses |

|
| Herpes Simplex Virus |

|
| Varicella Zoster Virus |

|
| Cytomegalovirus (CMV) |

|
| Epstein-Barr Virus (EBV) |

|
| Human Herpesvirus-6 (HHV-6) |

|
| Human Herpesvirus-8 (HHV-8) |

|
| Other DNA Viruses |

|
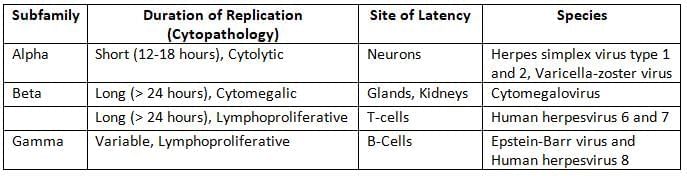
Herpesviruses
Members of the Herpesviridae family have the following characteristics:
- They are large (150–200 nm in size), spherical, and exhibit icosahedral symmetry.
- The tegument is an amorphous structure found between the capsid and envelope.
- These viruses can cause latent or persistent infections and have the ability to reactivate periodically.
- They contain double-stranded DNA (dsDNA) and replicate using the rolling circle mechanism.
Herpes Simplex Virus
Clinical Manifestations
The incubation period ranges from 1 to 26 days (median, 6–8 days).
Orofacial mucosal lesions: These are the most common signs of Herpes Simplex Virus (HSV).
- Most common affected area: The buccal mucosa (the inside of the cheeks).
- Frequent primary lesions:
- Gingivostomatitis: Inflammation of the gums and mouth.
- Pharyngitis: Inflammation of the throat.
- Most common recurrent lesion: Herpes labialis, which appears as painful blisters near the lips.
Nervous system
- Encephalitis: The most common cause of acute sporadic viral encephalitis is HSV, primarily affecting the temporal lobe. More than 95% of these cases are caused by HSV-1.
- Children typically experience a primary infection: HSV enters the body from the outside and reaches the CNS through the olfactory bulb.
- Adults often have recurrent infections due to HSV reactivating in the trigeminal nerve.
- Meningitis: HSV can lead to recurrent lymphocytic meningitis, known as Mollaret’s meningitis.
- Other manifestationsinclude:
- Autonomous nervous system involvement, particularly in the sacral region.
- Transverse myelitis.
- Guillain-Barré syndrome.
- Peripheral nervous system issues, such as Bell’s palsy.
Cutaneous lesions: HSV usually infects through broken skin, leading to various skin issues.
- Herpetic whitlow: Lesions found on the fingers of dentists and hospital staff.
- Febrile blisters.
- Herpes gladiatorum: Skin lesions on wrestlers' bodies.
- Eczema herpeticum: Caused by HSV-1 in people with chronic eczema. Similar lesions can also be seen from vaccinia virus infection; together, these are called Kaposi’s varicelliform eruptions.
- Erythema multiforme: The most common association is with HSV.
Ocular lesions: HSV-1 is more likely than HSV-2 to infect the eyes.
- Severe conjunctivitis is the most frequent symptom.
- Recurrent lesions can turn into dendritic ulcers on the cornea or vesicles on the eyelids.
- Corneal blindness.
Genital lesions: HSV-2 is more common than HSV-1 for causing both primary and recurrent genital lesions.
- Genital lesions are usually described as painful, bilateral, small vesicular ulcers.
- These may occur alongside fever and inguinal lymphadenopathy.
Visceral and disseminated herpes:
- Risk factors: include being immunocompromised, having malnutrition, or being pregnant.
- Common symptoms include pneumonitis, tracheobronchitis, and hepatitis.
Neonatal herpes: HSV is a common cause of congenital infections, similar to other TORCH agents.
- Transmission: Can happen in utero or after birth, but mostly during birth.
- The risk of developing neonatal herpes is significantly higher (10 times) if the mother recently gets the virus (primary infection).
- HSV-2 is more likely than HSV-1 to cause neonatal herpes, accounting for 75% of cases.
- There is a greater likelihood of developing visceral infections.
Laboratory Diagnosis
- Cytopathology: Tzanck smear preparation using Wright’s or Giemsa stain:
- Identifies the presence of inclusion bodies, specifically the Lipschultz body, and the formation of multinucleated giant cells, as well as the swelling of infected cells.
- This method cannot distinguish between HSV-1, HSV-2, and VZV.
- The sensitivity of this staining technique is low, with less than 30% effectiveness for mucosal swabs.
- Virus isolation: This remains the most reliable method for diagnosing HSV.
- Using conventional cell lines can reveal significant rounding and swelling of the cells.
- Viral antigen detection: This can be performed on specimens using direct immunofluorescence (IF).
- This method is both sensitive and specific, allowing for differentiation between HSV-1 and HSV-2.
- HSV DNA detection: The PCR test is the most sensitive and can effectively differentiate between HSV-1 and HSV-2.
- Antibody detection: This can be conducted using ELISAor other methods.
- Most tests typically identify IgG or total antibodies, which means they cannot distinguish between recent and past infections.
- Serologic assays that use type-specific antigens can differentiate between HSV-1 and HSV-2.
Treatment
- Acyclovir is the preferred medication for treating certain viral infections. It works by blocking the action of viral DNA polymerase, which is essential for the virus to replicate.
- In cases where the virus is resistant to acyclovir, Foscarnet becomes the recommended choice. This medication is used specifically when acyclovir is not effective.
Varicella Zoster Virus
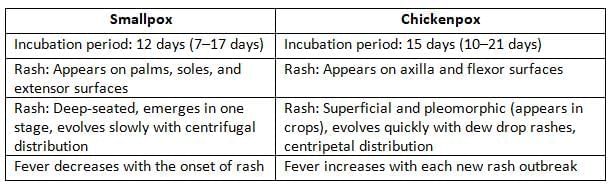
Varicella Zoster Virus (VZV) is responsible for causing vesicular rashes on the skin and mucous membranes in two forms:
- Chickenpox: This occurs after the primary infection, usually affecting children, and is characterised by diffuse bilateral vesicular rashes.
- Zoster or Shingles: This follows the reactivation of latent VZV in the ophthalmic branch of the trigeminal ganglia. It mainly affects adults and results in unilateral and segmental vesicular rashes.
Chickenpox
Clinical Manifestations
- Incubation Period: The incubation period for chickenpox ranges from 10 to 21 days, typically lasting about 2 to 3 weeks.
- Rash Characteristics:
- The rash is vesicular, bilateral, diffuse, and centripetal, meaning it starts on the face and trunk and spreads quickly to the flexor surfaces.
- Rashes appear in multiple crops, with fever accompanying each crop.
- Age Group: Chickenpox is primarily a disease of childhood. When it occurs in adults, it is usually more severe, presenting with bullous and haemorrhagic rashes.
Complications
Complications are more frequent in adults and individuals with a weakened immune system.
- The most prevalent infectious complication is a bacterial infection of the skin.
- The most common extracutaneous complication involves the central nervous system, including conditions like cerebellar ataxia, encephalitis, and aseptic meningitis; this situation typically occurs in children.
- The most severe complication is varicella pneumonia, which frequently develops in pregnant women.
- Reye’s syndrome: This condition involves fatty degeneration of the liver and is associated with the intake of salicylates, such as aspirin.
Chickenpox during pregnancy poses risks to both the mother and the fetus.
- Mothers are at a heightened risk of developing varicella pneumonia.
- Fetal or congenital varicella syndrome: The varicella-zoster virus (VZV) is highly teratogenic, meaning it can cause severe developmental issues in the fetus.
- The risk of fetal infection is highest when the mother acquires a primary VZV infection during pregnancy.
- During the late first trimester to early second trimester, there is an increased frequency of congenital malformations in the fetus, which may include:
- Cicatricial skin lesions (scarring skin abnormalities)
- Limb hypoplasia (underdeveloped limbs)
- Microcephaly (abnormally small head size)
- Infections occurring close to the time of delivery can pose significant risks to the newborn.
- If the mother contracts the infection more than 5 days before delivery, the baby is usually asymptomatic due to the protective maternal antibodies passed to the fetus.
- If the mother contracts the infection within 5 days to 2 days after delivery, there may not be sufficient time for maternal antibodies to develop. This can lead to the virus spreading to the baby, resulting in a severe form of chickenpox known as neonatal varicella.
Epidemiology of Chickenpox
Chickenpox is a highly contagious viral infection caused by the varicella-zoster virus (VZV).
- Period of Infectivity: Individuals with chickenpox are infectious from 2 days before the rash appears until 5 days after, or until the blisters have crusted over.
- Immunity: single attack of chickenpox provides lifelong immunity.
- Reservoir: Humans are the only known hosts for the varicella-zoster virus.
- Source of Infection: Infected patients are the only source of the virus; there are no asymptomatic carriers.
- Secondary Attack Rate: The rate of secondary infection among susceptible individuals is very high.
Zoster (Shingles)
Zoster typically occurs due to the reactivation of latent VZV, particularly in individuals over 60 years of age, those with weakened immune systems, or rarely in healthy adults.
- The rashes associated with zoster are unilateral and segmental, confined to the area of skin supplied by the affected nerves.
- Post-herpetic Neuralgia: This is the most common complication in elderly patients, characterized by pain at the local site of the rash.
- Ramsay Hunt Syndrome: This syndrome occurs when the geniculate ganglion of the facial nerve is affected. It is characterized by facial nerve palsy and vesicles located on the tympanic membrane, external auditory meatus, and tongue.
Vaccine
- A live attenuated vaccine using the Oka strain of VZV is available to prevent chickenpox.
- The vaccine is administered to children after 1 year of age, with 2 doses recommended: the first dose at 12–15 months and the second dose at 4–6 years of age.
Treatment
Acyclovir: Acyclovir is the drug of choice for preventing complications of chickenpox and halting the progression of zoster in adults. However, it cannot prevent post-herpetic neuralgia.
- Acyclovir is recommended for post-exposure prophylaxis, ideally within 72 to 96 hours of exposure.
- It is indicated for neonates born to mothers with chickenpox if the onset of the mother’s infection occurs between 5 days before delivery and up to 48 hours after delivery.
Cytomegalovirus (CMV)
CMV is the largest virus within the Herpesviridae family and is named for its ability to cause significant enlargement of the host cells it infects.
- Host Specificity: CMV is specific to certain species.
- Cell Type Specificity: CMV primarily infects kidney and salivary gland cells.
- Cell-to-Cell Spread: CMV typically spreads from cell to cell, with very little of the virus being free in the body.
Clinical Manifestations
Congenital CMV Infection
- Cytomegalovirus (CMV) is one of the most common infections transmitted from mother to child during pregnancy, and it is associated with congenital defects in nearly 1% of newborns.
- Cytomegalic Inclusion Disease
- This condition occurs in about 5% of infected fetuses.
- While some infants may appear healthy at birth, 5–25% of them could develop serious problems with development, hearing, vision, or dental health within the first two years of life.
- Congenital Defects
- Common Defects: These include petechiae (small red or purple spots), hepatosplenomegaly (enlargement of the liver and spleen), and jaundice (yellowing of the skin and eyes).
- Less Common Defects: These may include microcephaly (small head size), cerebral calcifications (calcium deposits in the brain), intrauterine growth restriction (IUGR), and prematurity (being born too early).
- The risk of congenital defects is highest when the infection occurs early in pregnancy, particularly if the mother is experiencing her first infection at that time.
Perinatal Cytomegalovirus (CMV) Infection
- Transmission to Newborn: CMV can be transmitted to newborns during:
- Delivery
- Postnatal period through infected breast milk or mother's secretions
- Asymptomatic Individuals: Most people infected with CMV are asymptomatic but can shed the virus in their urine for several years.
- Premature Infants: Some infants, particularly those born prematurely, may develop interstitial pneumonitis due to CMV infection.
Immunocompetent Adults
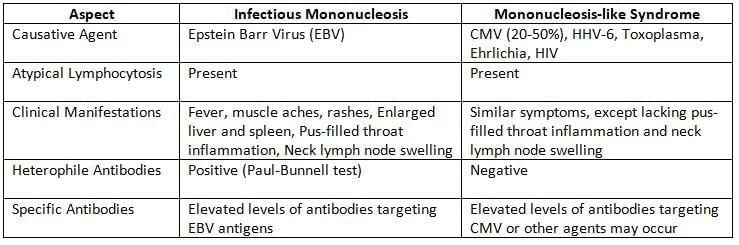
- Mononucleosis-like Syndrome: Healthy adults may develop a mononucleosis-like syndrome after receiving a blood transfusion.
In the Immunocompromised Host
- CMV can cause serious infections in people with weak immune systems, especially when latent CMV viruses reactivate.
- In AIDS patients who have a CD4 T-cell count below 50 cells per microliter, CMVcan lead to:
- Chorioretinitis (the most common symptom)
- Gastroenteritis
- Dementia
- For organ transplant recipients, CMV is likely the most common viral infection.
- Typically, CMV infection happens between 1 to 4 months after the transplant.
- In patients who receive a bone marrow transplant, CMV can cause bilateral interstitial pneumonia.
Epidemiology
- Transmission of CMV: CMV spreads through close contact, unlike HSV (Herpes Simplex Virus).
- The primary modes of transmission are oral and respiratory contact.
- Other methods of transmission include:
- Transplacental transmission (from mother to fetus)
- Blood transfusion (risk varies from 0.1% to 10%)
- Sexual transmission
- Reservoir for CMV: Humans are the only known hosts for Cytomegalovirus.
- Prevalence of CMV: In developing countries, about 90% of the population is seropositive (has antibodies against CMV), whereas in developed countries, the rate is 40% to 70%.
Laboratory Diagnosis
- Detection of CMV: Inclusion Bodies in Urine: CMV produces characteristic inclusion bodies in cells, known as "Owl’s eye appearance," which can be seen in urine samples.
- Virus Isolation: CMV can be isolated from throat washings and urine samples.
- Best Cell Lines: Human fibroblasts are the most effective cell lines for isolating CMV, with growth observed within 2 to 3 weeks.
- Shell Vial Technique: This method allows for the detection of CMV growth within 4 to 5 days.
- Antibody Detection:
- IgM Antibodies: The presence of IgM antibodies indicates an active CMV infection.
- IgG Antibodies: fourfold increase in IgG antibodies suggests a recurrent CMV infection.
- Immunocompromised Patients: In patients with compromised immune systems, antibodies may be undetectable, making this method less reliable.
- Antigen Detection: This method involves the detection of CMV-specific pp65 antigens, which is a highly specific and reliable way to diagnose CMV infections.
- PCR (Polymerase Chain Reaction): PCR is used to detect specific CMV DNA in blood or body fluids such as cerebrospinal fluid (CSF). This method is highly sensitive and can identify CMV infections even when the virus is present in low quantities.
Treatment
CMV does not respond to acyclovir.
- Ganciclovir is the DOC for cytomegalic inclusion disease or retinitis or transplant infections.
- Others: Valganciclovir (given orally), foscarnet (DOC in ganciclovir-resistant cases), cidofovir and CMV Ig.
Epstein-Barr Virus (EBV)
Pathogenesis
- EBV is spread through contact in the mouth, mainly via infected saliva.
- It attaches to specific receptors called complement receptors (CD21 or CR2) found on B-cells and cells in the throat.
- The initial infection happens in the throat area, where EBV multiplies in the epithelial cells or B-lymphocytes located in the throat and salivary glands.
- Once inside B-cells, EBV goes into a latent phase.
- In children, the virus can lead to a condition known as infectious mononucleosis:
- The infected B-cells become immortal due to the virus and start producing a large variety of immunoglobulins (polyclonal), including many autoantibodies.
- As a result, the surrounding CD8 T-lymphocytes are activated and appear atypical.
- In some individuals, EBV can trigger cancer (the process of oncogenesis):
- EBV can cause infected B-cells and epithelial cells to become cancerous by producing latent EBV antigens such as LMP and EBNA.
- LMP-1 (latent membrane protein-1) is the main viral gene responsible for cancer.
- The viral EBNA-2 (EBV nuclear antigen-2) activates the host cell's cyclin-D, which encourages cell growth.
Clinical Manifestations
Infectious Mononucleosis
- Infectious mononucleosis, commonly referred to as the kissing disease or glandular disease, is primarily transmitted through saliva.
- This condition predominantly affects young adults in developed countries.
- Symptoms of infectious mononucleosis include:
- Headache, fever, and a general feeling of illness.
- Swelling of lymph nodes in the neck, along with enlargement of the liver and spleen.
- Rashes may develop following the administration of ampicillin.
- Presence of atypical lymphocytes, particularly CD8 T cells.
- Detection of autoantibodies reacting to sheep red blood cell antigens, as indicated by the Paul-Bunnell test.
EBV-Associated Malignancies
EBV (Epstein-Barr Virus) is associated with various cancers, including:
- Burkitt’s Lymphoma: Affects the jaw in children and young adults. EBV is linked to about 90% of African cases and 20% of non-African cases. Most cases involve a pre-existing mutation [t(8;14)] that activates the MYC oncogene, promoting cell growth.
- Nasopharyngeal Carcinoma: More common among Chinese individuals, often linked to the consumption of salted fish (containing nitrosamines) and the use of herbal snuff (containing phorbol esters).
- Hodgkin’s Lymphoma: Especially the mixed-cellularity type.
- Non-Hodgkin’s Lymphoma (NHL): A significant number of central nervous system NHL cases and about 50% of systemic NHL cases are EBV positive.
Other Conditions Linked to EBV
- Post-transplant lymphoproliferative disorder, a genetic condition that mainly affects young boys.
- In some patients with HIV and transplant recipients, a wart-like growth of epithelial cells on the tongue may occur.
- Chronic fatigue syndrome.
Laboratory Diagnosis
Heterophile Antibody Detection by Paul-Bunnell Test
- The Heterophile Antibody Detection by Paul-Bunnell Test is used to detect heterophile antibodies in a patient's serum using sheep red blood cells.
- Confirmation is done through the differential absorption test and Monospot test.
Detection of EBV-Specific Antibodies
- Antibodies to viral capsid antigen (VCA):
- IgM: Indicates a current infection.
- IgG: Indicates past infection and immunity.
- Antibodies to early antigen (EA):
- EA-D antibody: Targets the early antigen, which is present in the nuclei and cytoplasm of infected cells. This antibody is elevated during acute infections and in conditions like Burkitt's lymphoma.
- EA-R antibody: Restricted to the cytoplasm and is elevated in nasopharyngeal carcinoma.
- Antibodies to EBNA (EBV nuclear antigen): Indicate past infection, but a significant increase in antibody levels suggests a current infection.
Treatment
- Acyclovir: Effective for oral hairy leukoplakia, but its use in treating infectious mononucleosis is limited, and it is generally not effective for most malignancies.
- Rituximab: An antibody targeting CD20, has shown effectiveness in some cases of EBV-related conditions.
Human Herpesvirus-6 (HHV-6)
HHV-6 infects T-cells by binding to the CD46 receptor. There are two types of HHV-6: 6A and 6B.
- In children, HHV-6, usually the 6B variant, causes a condition known as sixth disease, which is also called exanthema subitum or roseola infantum.
- In older individuals, HHV-6 is associated with a mononucleosis-like syndrome.
Human Herpesvirus-8 (HHV-8)
HHV-8 is known as Kaposi’s sarcoma-associated herpesvirus (KSHV).- Epidemiology
- In areas with high rates, HHV-8 is common in Africa and spreads through oral secretions.
- In areas with low rates like North America, Asia, and northern Europe, it mainly affects homosexual men.
- Less common ways of transmission include organ transplants, IV drug use, and blood transfusions.
- Manifestations: In people with weakened immune systems (like those with HIV), HHV-8 can cause:
- Kaposi’s sarcoma
- Primary effusion lymphoma (lymphomas that occur in body cavities)
- Castleman’s disease (a condition affecting B-cells)
- In people with healthy immune systems, HHV-8 may lead to fever and rash.
- Treatment: Infections caused by HHV can be effectively treated with:
- Foscarnet
- Ganciclovir
- Cidofovir
Other DNA Viruses
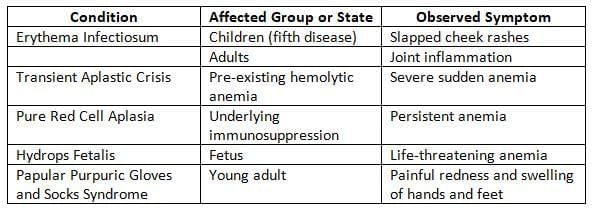
Parvoviruses
- Parvoviruses are the smallest known viruses, measuring between 18 and 26 nanometers.
- They are nonenveloped and have a shape that shows icosahedral symmetry.
- These viruses contain linear single-stranded DNA, making them unique as the only DNA viruses with this structure.
- Transmission: Parvovirus B19 primarily infects humans, typically spreading through the respiratory route. Other methods of transmission include:
- Blood transfusions
- Transplacental transmission (which occurs in 30% of cases, with the highest risk during the second trimester).
- Tropism for RBCs: This virus targets red blood cell (RBC) precursors by using the P blood group antigen as its receptor.
- Genotyping: Parvovirus B19 has three different genotypes but only one serotype. The most common genotype worldwide is genotype 1, while genotype 3 is most prevalent in Western Africa.
Papillomaviridae and Polyomaviridae
- The family formerly known as Papovaviridae is now divided into two distinct families.
- The Papillomaviridae family includes 16 genera, and one of these, the Human papillomavirus, specifically infects humans.
- The Polyomaviridae family contains several genera that infect animals. In humans, the following infections are noted:
- The JC virus can cause Progressive Multifocal Leukoencephalopathy (PML).
- The BK virus can lead to kidney problems in those who have received transplants. It is different from the JC virus because it can grow in a variety of cell types and is not as likely to cause cancer.
- The Merkel cell virus is linked to a type of skin cancer called Merkel cell carcinoma.
- The SV40 virus (Simian vacuolating 40 virus) does not cause disease in humans.
Human Papillomavirus (HPV)
The HPV primarily affects the skin and mucous membranes, causing various infections. Early gene products E6 and E7 have cancer-causing potential in these ways: HPV targets skin (squamous epithelium) and mucous membranes, leading to both benign and malignant growths.
Pathogenesis
- HPV affects the skin (specifically squamous epithelium) and mucous membranes, leading to various benign and malignant growths.
- Benign warts include:
- Common warts (known as verruca vulgaris) and flat warts (verruca plana) found in children.
- Plantar warts (verruca plantaris) that appear in young adults.
- Anogenital warts (condyloma acuminatum) observed in adults.
- Epidermodysplasia verruciformis is another condition related to HPV.
- Cervical lesions include:
- CIN (Cervical Intraepithelial Neoplasia) is a benign condition linked to low-risk HPV types 6 and 11.
- Cervical cancer (squamous cell carcinoma) is connected to high-risk HPV types such as 16, 18, 31, 33, and 45.
- High-risk serotypes can also lead to squamous cell carcinoma in other genital areas, including the penis, anus, vagina, and vulva.
HPV Vaccine
- The HPV vaccine is recommended for girls and young women.
- This subunit vaccine is composed of virus-like particles containing HPV L1 proteins, which are produced using yeast through DNA recombinant technology.
- The quadrivalent vaccine offers protection against types 6, 11, 16, and 18, known as Gardasil by Merck.
- The bivalent vaccine targets the high-risk types 16 and 18, called Cervarix from GlaxoSmithKline.
- Utilizing barrier methods of contraception can aid in preventing the sexual transmission of HPV, thereby reducing the risk of anogenital infections.
Poxviridae
- Poxvirusesare the largest viruses, with a size of approximately 400 nm, allowing them to be seen under a light microscope.
- They possess the most intricate structure among viruses.
- Their shape can be either brick-shaped or ellipsoid.
- The nucleocapsid contains a biconcave dumbbell-shaped DNA core.
- Unlike most large DNA viruses, poxviruses replicate in the cytoplasm.
- Important members of this family include: Variola, Vaccinia, and Molluscum contagiosum.
Smallpox (Variola)
Smallpox is a contagious and severe skin disease that leads to rashes. It was the first disease to be eradicated globally.
Timeline
- The final natural case of variola major was documented in a woman from Bangladesh in May 1975.
- The last natural case of variola minor took place in Merca, Somalia, on 26th October 1977.
- The World Health Organization (WHO) announced the eradication almost three years later, on 8th May 1980.
- Following eradication, vaccination ceased. As a result, individuals born after 1980 are not immunised, raising the possibility of smallpox being used as a bioterrorism weapon.
Factors Contributing to Successful Eradication
- Variola exclusively infects humans, eliminating the presence of animal carriers.
- Infected individuals were the only source of the virus, as there was no carrier state.
- Case identification was easy due to the unique appearance of the rash.
- Asymptomatic individuals did not transmit the virus.
- The global smallpox eradication initiative was exceptionally effective.
- A highly effective live vaccinia vaccine was utilised.
- Stable freeze-dried vaccine formulations were created.
- The vaccine was administered using a bifurcated needle through a simple and cost-effective multiple puncture method.
Vaccination
- Live vaccinia vaccine was very effective.
- It was administered as a single dose when children were between 1-2 years old.
- Because it used an un-attenuated live virus, there were often side effects.
- The cowpox vaccine was discovered by Edward Jenner, known as the father of vaccination.
- Variolation involved giving healthy individuals small amounts of skin scraping from a smallpox patient.
Vaccinia
Vaccinia is different from variola in several ways:
- It is not harmful to humans or causes less severe skin lesions.
- It produces a structure called a Guarnieri body, while variola produces a Paschen body.
- When grown on chick embryo membranes (CAM), vaccinia virus creates larger, hemorrhagic, and necrotic pock lesions.
- The ceiling temperature is the highest temperature at which pock formation can happen on CAM; this temperature is higher for vaccinia virus (41 °C) than for variola virus (38 °C).
- Vaccinia can create plaques on chick embryo tissue cultures, but variola cannot.
Molluscum Contagiosum Virus
- Lesions: Causes pink, pearly wart-like bumps with a central dimple (umbilicated).
- Can occur anywhere on the body except palms and soles; genital lesions are common in adults.
- Spread: Among children through direct and indirect contact.
- Transmission: Sexual transmission primarily affects adults, but can occur in young adults under certain conditions.
- Laboratory Diagnosis: Molluscum bodies are intracytoplasmic eosinophilic inclusions found in skin scrapings (histopathological stains).
- The virus cannot be cultured in tissue culture, eggs, or animals.
- Treatment: Surgical removal of lesions through ablation.
- Prognosis: Generally self-limiting, except in cases of HIV.
Adenoviridae
Adenoviruses are non-enveloped DNA viruses that resemble space vehicles in shape.
Bacteriophages
- Bacteriophages are viruses that specifically infect and target bacteria. They typically have a shape similar to a tadpole, with a hexagonal head and a tail with tail fibers.
- The hexagonal head of a bacteriophage contains tightly coiled double-stranded DNA (dsDNA) and is protected by a capsid, which is a protein coat. However, some bacteriophages may have different shapes or structures. For example:
- Shape: Bacteriophages can be spherical or filamentous instead of hexagonal.
- Nucleic acid: Some bacteriophages may have single-stranded DNA (ssDNA) or RNA instead of dsDNA.
Life Cycle of Bacteriophage
Bacteriophages can be classified into two categories based on their life cycles: Lytic and Lysogenic (or temperate) phages.
- Lytic phase: In this phase, the bacteriophage replicates inside the cytoplasm of the host bacterium, leading to the bursting of the host cell.
- The process of replication in the lytic phase is similar to that of other DNA viruses, but there are some differences:
- During the penetration step, bacteriophages attach to the bacterial cell wall, appearing as "ghosts."
- Unlike other viruses, there is no uncoating step in the case of bacteriophages.
- Daughter phages are released by the lysis of the host bacterium.
- The eclipse phase in bacteriophages lasts about 15 to 30 minutes, whereas it can take 15 to 30 hours for most animal viruses.
- Lysogenic or temperate phase: In this phase, the phage DNA integrates into the host DNA and remains dormant as a prophage.
- Lysogenic to lytic interconversion: Under certain environmental conditions, temperate phages can detach from the bacterial chromosome, become lytic phages, multiply in the cytoplasm, and be released through lysis.
Uses of Bacteriophage
- Phage typing: Bacteriophages are used to identify specific bacteria, including:
- Staphylococcus aureus
- Vi antigen typing of Salmonella Typhi
- Vibrio cholerae (Basu Mukherjee phage typing)
- Brucella (Tbilisi phage typing)
- Corynebacterium diphtheriae
- Phage assay: This method estimates the number of viable phages in preparations.
- Phage therapy: Lytic phages are used in phage therapy to combat bacterial infections, including those resulting from burns and wounds.
- Diagnosis: Mycobacteriophages are employed to identify Mycobacterium tuberculosis.
- Cloning vector: Bacteriophages are used as cloning vectors in genetic engineering.
- Transduction: In Staphylococcus aureus, plasmids coding for β-lactamases are transferred between strains via transduction.
- Toxin coding: Phage genomes encode various bacterial toxins, including:
- A and C of Streptococcal pyrogenic toxin
- Botulinum toxin C and D
- Cholera toxin
- Diphtheria toxin
- Enterohemorrhagic E. coli (EHEC) Verocytotoxin
- Antigenic alteration: Bacteriophages can alter the antigenic properties of bacteria, as seen in Salmonella.
|
75 docs|5 tests
|
FAQs on Herpesviruses and Other DNA Viruses Chapter Notes - Microbiology - NEET PG
| 1. What are the clinical manifestations of chickenpox and shingles? |  |
| 2. How is the laboratory diagnosis of herpesviruses conducted? |  |
| 3. What treatment options are available for chickenpox and shingles? |  |
| 4. What vaccines are available for chickenpox and shingles? |  |
| 5. What is the epidemiology and pathogenesis of chickenpox and shingles? |  |














