NEET PG Exam > NEET PG Notes > Microbiology > Chapter Notes: Intestinal Amebae, Free-Living Ameba and Balantidium Coli
Intestinal Amebae, Free-Living Ameba and Balantidium Coli Chapter Notes | Microbiology - NEET PG PDF Download
Intestinal Amebae: Entamoeba Histolytica
- Entamoeba histolytica resides in the large intestine of humans.
- It exists in three morphological stages: trophozoites, pre-cyst, and cyst.
Life Cycle
- Humans serve as the sole host for Entamoeba histolytica.
- The mature quadrinucleate cyst is the infective form.
- Transmission occurs primarily through the faeco-oral route, with rare cases (20–30%) via sexual transmission among homosexuals.
- Excystation happens in the small intestine, releasing eight small metacystic trophozoites.
- These trophozoites are carried to the large intestine, where they colonize the gastrointestinal mucosa.
- Depending on the host’s nutritional status and immunity, outcomes include:
- Asymptomatic cyst passers.
- Amebic dysentery.
- Amebic liver abscess.
- Encystation occurs in the large intestine, starting with precyst formation, followed by immature cysts, and culminating in mature quadrinucleated cysts released in feces, which are the diagnostic form.
- For example, the life cycle illustrates how a person consuming contaminated water with mature cysts can develop amebic dysentery if trophozoites invade the intestinal mucosa, highlighting the faeco-oral transmission risk in poor sanitation settings.
Virulence Factors
- Amebic lectin antigen aids in adhesion to host tissues.
- Other factors include cysteine proteinase, amebapore, hydrolytic enzymes, neuraminidase, and metallocollagenase, which contribute to tissue invasion and damage.
Intestinal Amebiasis
- Affects males and females equally, with a 1:1 ratio.
- Amebic ulcers are flask-shaped, featuring a broad base and narrow neck.
- The ileocecal region is the most common site for these ulcers.
- Complications include:
- Fulminant amebic colitis.
- Amebic appendicitis.
- Intestinal perforation and amebic peritonitis.
- Toxic megacolon and intussusception.
- Perianal skin ulcers.
- Ameboma, a diffuse pseudotumor-like mass in the recto-sigmoid region, seen in chronic amebiasis.
Amebic Liver Abscess
- The posterior superior surface of the right lobe of the liver is the most commonly affected site.
- Male to female ratio is 9:1.
- Liver abscess pus, known as anchovy sauce pus, is thick and chocolate brown in color.
- Other organs that may be affected include the lung, brain, and skin.
Laboratory Diagnosis
- Collect at least three stool samples on consecutive days due to intermittent shedding of amebae.
- Stool microscopy identifies:
- Trophozoites, indicating active infection.
- Quadrinucleated cysts, indicating a carrier state.
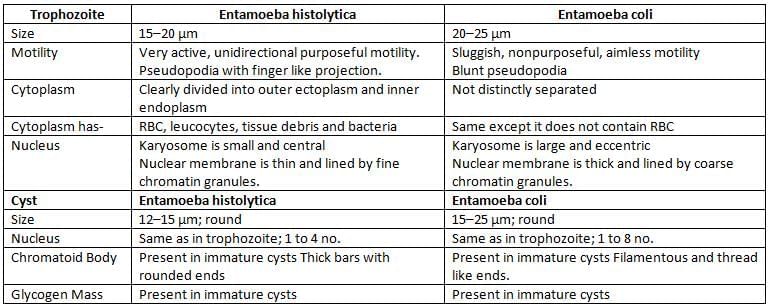
- Differentiation is necessary between Entamoeba histolytica and Entamoeba coli, a commensal in stool.
- Stool culture is used for detection.
- Polyxenic culture includes bacterial supplements to nourish amebae, used for chronic or asymptomatic carriers with low cyst numbers.
- Polyxenic culture has 50–70% sensitivity and 100% specificity, considered the gold standard.
- Culture media include:
- National Institute of Health (NIH) media.
- Boeck and Drbohlav egg serum medium with Locke’s solution.
- Balamuth’s medium, Nelson’s medium, and Robinson’s medium.
- Axenic culture, lacking bacterial supplements (e.g., Diamond’s medium), is useful for:
- Studying ameba pathogenicity.
- Testing antiamebic drug susceptibility.
- Preparing amebic antigen for serological tests.
- Harvesting parasites for zymodeme pattern analysis.
- Stool antigen detection (copro-antigen) uses ELISA or immunochromatographic tests (ICT) to detect lectin antigen.
- Amebic antigen in serum indicates recent or active infection, detected via ELISA for lectin antigen.
- Amebic antibodies appear in later stages of intestinal amebiasis, detected by ELISA, indirect fluorescent antibody (IFA), or indirect hemagglutination test (IHA).
- Zymodeme analysis detects isoenzyme markers such as malic enzyme, hexokinase, and isomerase.
- Nested multiplex PCR is used for diagnosis.
- Presence of Charcot-Leyden crystals in stool and moderate leucocytosis in blood are additional findings.
Laboratory Diagnosis of Amebic Liver Abscess
- Microscopy and histopathology of liver pus reveal trophozoites but never cysts, with low sensitivity (<25%) but high specificity.
- Stool microscopy and culture are not useful for liver abscess diagnosis.
- Lectin antigen is usually absent in stool but detectable in serum, liver pus, and saliva.
- Antibody levels are often elevated, detected by ELISA and IHA, but persist post-cure, making it difficult to distinguish recent from past infections.
- PCR is performed on amebic liver pus.
- Ultrasound (USG) of the liver identifies the abscess site and its extension.
Characteristics of Trophozoites and Cysts of Common Intestinal Entamoeba Species
E. Histolytica Comprises of Three Subspecies
- Subspecies include E. h. histolytica, E. h. dispar, and E. h. moshkovskii.
- Cysts and trophozoites of all three subspecies are morphologically identical.
- All colonize the large intestine, but only E. h. histolytica causes invasive disease.
- Differentiation is based on:
- Lectin antigen, present only in E. h. histolytica.
- Presence of RBCs inside trophozoites, indicating invasion, found only in E. h. histolytica.
- PCR.
- Distinct isoenzyme markers via zymodeme study.
Treatment
- Amebic dysentery or amebic liver abscess is treated with tinidazole and metronidazole.
- Luminal infection is treated with paromomycin and iodoquinol.
Free-living Amebae
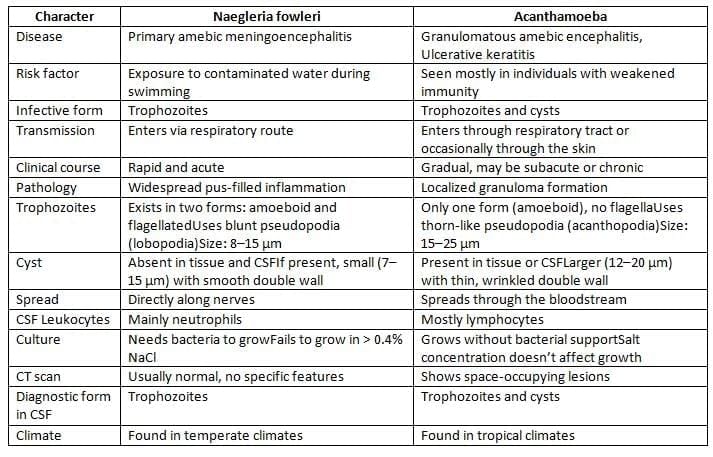
Other Free-Living Ameba
- Balamuthia mandrillaris causes granulomatous amebic encephalitis (GAE) and skin lesions.
- Sappinia diploidea is another free-living ameba.
Balantidium Coli
- Only ciliate parasite that affects humans: The active form, called trophozoite, has tiny hair-like structures.
- Largest protozoan that can invade the human digestive system.
- Location affected: Primarily the large intestine.
- Infective stage: Cysts found in food or drinks that are contaminated.
- Both the trophozoite and cyst forms contain two nuclei: a macronucleus and a micronucleus.
- Trophozoites reproduce through binary fission and conjugation.
- Dysentery: Causes ulcers similar to those from amoebic infections but does not penetrate the muscle layer.
- Diagnosis: Identification of cysts is more common than finding trophozoites.
- Treatment: The main medication used is tetracycline.
The document Intestinal Amebae, Free-Living Ameba and Balantidium Coli Chapter Notes | Microbiology - NEET PG is a part of the NEET PG Course Microbiology.
All you need of NEET PG at this link: NEET PG
|
75 docs|5 tests
|
FAQs on Intestinal Amebae, Free-Living Ameba and Balantidium Coli Chapter Notes - Microbiology - NEET PG
| 1. What are the main life cycle stages of intestinal amebae, and how do they contribute to transmission? |  |
Ans. The life cycle of intestinal amebae, particularly Entamoeba histolytica, includes two main stages: the trophozoite and the cyst stage. The trophozoite is the active, feeding stage that resides in the intestines, while the cyst is a dormant form that can survive outside the host and is responsible for transmission through contaminated food or water. When ingested, the cysts pass through the stomach and excyst in the intestines, releasing trophozoites that can invade the intestinal lining and cause disease.
| 2. What virulence factors do intestinal amebae possess that contribute to their pathogenicity? |  |
Ans. Intestinal amebae, especially E. histolytica, possess several virulence factors that enhance their pathogenicity. These include the ability to produce proteolytic enzymes that degrade host tissues, adherence factors that facilitate colonization, and the ability to evade the host immune response. Additionally, they can induce apoptosis in host cells and disrupt tight junctions in the intestinal epithelium, contributing to tissue damage and inflammation.
| 3. What are the clinical manifestations of amebic liver abscess, and how does it develop from intestinal amebiasis? |  |
Ans. Amebic liver abscess is a serious complication that can arise from intestinal amebiasis. It typically develops when trophozoites invade the portal circulation and migrate to the liver, leading to necrosis and abscess formation. Clinically, patients may present with fever, right upper quadrant pain, and signs of hepatomegaly. If not treated promptly, it can lead to severe complications, including sepsis or death.
| 4. How is laboratory diagnosis performed for amebic liver abscess and intestinal amebiasis? |  |
Ans. Laboratory diagnosis of amebic liver abscess and intestinal amebiasis typically involves stool examination for cysts and trophozoites, serological tests for antibodies against E. histolytica, and imaging studies like ultrasound or CT scans to identify abscesses in the liver. Stool samples should be examined for multiple days due to intermittent shedding of cysts. Serological tests can help confirm the diagnosis, especially in cases where stool examination is inconclusive.
| 5. What are the characteristics of trophozoites and cysts of common intestinal Entamoeba species? |  |
Ans. The trophozoites of Entamoeba histolytica are typically 20-30 µm in size, have a single nucleus with a central karyosome, and may contain ingested red blood cells. In contrast, the cysts are round, 10-20 µm in size, and contain 1-4 nuclei, with a characteristic thick cyst wall. Differentiating between E. histolytica and other species like E. dispar is crucial, as only E. histolytica is pathogenic.
Related Searches















