Miscellaneous Bacteria Chapter Notes | Microbiology - NEET PG PDF Download
Miscellaneous Gram-positive Bacteria
Listeria monocytogenes
Listeria monocytogenes is a type of bacteria found in food that can cause serious infections in humans, particularly in newborns, pregnant women, and the elderly.
Pathogenicity
- Listeria monocytogenes can grow in refrigerated foods and resist various preserving agents.
- It is transmitted through contaminated food, such as raw milk and dairy products, and can also be passed from mother to fetus.
- This bacterium can survive inside host cells by preventing the destruction of the phagosome and creating pores through a process involving listerio-lysin O.
- It spreads directly between cells by polymerizing host cell actin, a process facilitated by listeriopods.
Clinical Manifestations
- Infection During Pregnancy: Infection before 20 weeks of pregnancy is uncommon and may lead to abortion or stillbirth.
- Neonatal Disease: There are two types of neonatal disease:
- Early Onset
- Late Onset
- Adult Cases:
- This condition is associated with steroid therapy, HIV, diabetes mellitus (DM), and malignancy, particularly in patients treated with fludarabine.
- Bacteremia can lead to meningitis.
- The most common cause of meningitis in kidney transplant patients after one month is...
- Bacteremia can also cause gastroenteritis, which may occur after consuming contaminated milk, meat, or salad.
- Early Onset Neonatal Disease occurs:
- Within 5 days after birth
- Acquired from maternal genital flora
- Associated with obstetrical complications
- Most common form is neonatal sepsis
- Mortality rate is greater than 30%
- Does not cause nosocomial outbreaks
- Late Onset Neonatal Disease occurs:
- After 5 days of birth
- Acquired from the environment
- Not associated with obstetrical complications
- Most common form is neonatal meningitis
- Mortality rate is less than 10%
- Nosocomial outbreaks are observed
- Granulomatosis Infantiseptica is a rare condition and is not seen in late-onset cases.
Laboratory Diagnosis of Listeria
- Listeria is identified as Gram-positive coccobacilli that are catalase positive.
- The bacterium exhibits a characteristic tumbling type of motility.
- It is motile at 25°C but non-motile at 37°C, which is a key differentiating feature.
- Growth is enhanced when Listeria is cultured in thioglycollate broth at 4°C, a process known as cold enrichment.
- Suitable media for culture include blood agar, chocolate agar, and PALCAM agar, the latter being a selective medium.
- The Anton test is used to demonstrate the pathogenicity of Listeria monocytogenes by instilling the organism into a rabbit's eye, which leads to conjunctivitis.
Treatment
- DOC: Ampicillin (also penicillin)
- Alternate: Cotrimoxazole (if allergic to penicillin)
- Cephalosporins: These are not effective.
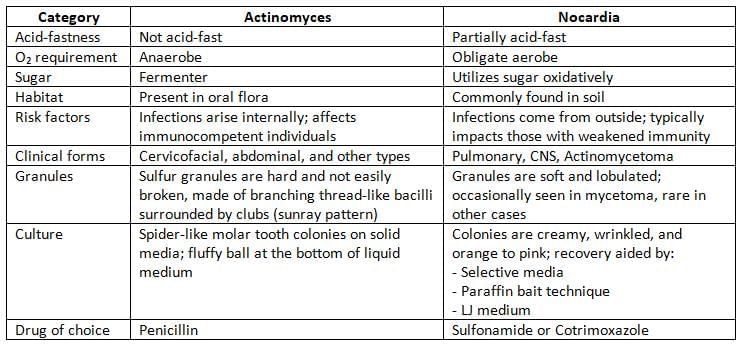
Actinomycetes
Actinomycetes are a group of Gram-positive bacteria known for their unique branching filamentous structure. Some species within this group can cause diseases in humans.
Human Pathogenic Actinomycetes:
- Actinomyces: These bacteria are non-acid fast and thrive in anaerobic environments. They are commonly found in the oral cavity and can cause infections when they enter deeper tissues.
- Streptomyces: These are aerobic bacteria that are non-acid fast. They are known for their role in soil ecology and can lead to a condition called actinomycetoma, which is characterized by tumor-like swelling in the skin.
- Nocardia: Nocardia species are acid-fast bacteria that can survive in harsh conditions, including 1% sulfuric acid. They are aerobic and can cause opportunistic infections, particularly in immunocompromised individuals.
- Actinomadura: Similar to Streptomyces, Actinomadura are aerobic and non-acid fast. They are also associated with actinomycetoma.
Tropheryma whipplei
- Tropheryma whipplei is a type of gram-positive actinomycete that is not closely related to any other known genus.
- It causes Whipple's disease, which primarily affects the small intestine.
- Common symptoms of Whipple's disease include:
- Fever
- Abdominal pain
- Diarrhea
- Weight loss
- Migratory polyarthralgia, which is pain in multiple joints that can move from one joint to another.
- The mesenteric lymph nodes in the small intestine are mainly affected by this disease.
Laboratory Diagnosis:
- Histopathological staining of an intestinal biopsy shows vacuoles within macrophages that contain bacilli positive for PAS stain.
- Culturing T. whipplei has been largely unsuccessful.
- PCR targeting 16S rRNA can be utilized to identify the bacilli.
Treatment of Whipple's Disease
- Penicillin, ampicillin, tetracycline, or cotrimoxazole for a duration of 1 to 2 years.
- Doxycycline combined with hydroxychloroquine for a period of 12 to 18 months.
Erysipelothrix Rhusopathiae
- Gram-positive bacilli
- Catalase negative, H2S positive
- Causes a skin condition known as erysipeloid, which results in a purple swelling that is very painful, but does not produce pus.
- The most common area affected is the finger, which is informally referred to as ‘seal finger’ or ‘whale finger’.
- Treatment: The drug of choice is penicillin G, but it is naturally resistant to vancomycin.
Miscellaneous Gram-Negative Bacteria
Campylobacter
Campylobacter species are curved, gram-negative bacilli that thrive in low-oxygen environments. These bacteria are primarily transmitted from animals to humans and are responsible for various illnesses, including diarrheal diseases caused by C. jejuni and systemic infections associated with C. fetus.
Epidemiology
- Mode of transmission:
- By eating raw or undercooked food, especially poultry (the most common source), raw (unpasteurized) milk, or contaminated water.
- Through direct contact with animals.
- Through oral-anal sexual contact.
- Age groups affected:
- C. jejuni primarily affects children.
- C. fetus affects individuals at the extremes of age (very young or elderly).
- Developing vs developed countries:
- In developing countries, the infection is often hyperendemic, meaning it is constantly present but usually shows no symptoms except in children under 2 years old, who may show symptoms.
- In developed countries, Campylobacter is the main bacterial cause of diarrheal disease.
- Seasonality:
- The number of cases usually increases during the summer and early autumn.
Pathogenesis
- Motility: Campylobacter strains possess a single polar flagellum, which enables them to move with a characteristic darting motion.
- Adhesion: These bacteria have the ability to adhere to host tissues, facilitating infection.
- Toxins: The role of toxins in pathogenesis is relatively minor and includes:
- Enterotoxin: heat-labile toxin similar to cholera toxin.
- Cytotoxins: Such as the cytolethal distending toxin (CDT).
- S-layer: Campylobacter fetus produces a proteinaceous capsule-like structure known as the S-layer, which may contribute to its pathogenicity.
Clinical Manifestations
- Intestinal Infections: Campylobacter can cause inflammatory diarrhea, abdominal pain, fever, and, in rare cases, bloody stools.
- Extraintestinal Infections: Primarily affect immunocompromised individuals and those at extreme ages, particularly with Campylobacter fetus.
- HLA-B27 Association: In individuals with the HLA-B27 antigen, Campylobacter infections may lead to reactive arthritis and other rheumatic symptoms.
- Guillain-Barre Syndrome: Campylobacter, especially the C. jejuni serotype O19, has been associated with triggering Guillain-Barre syndrome, although further clarification regarding α chain disease is needed.
Laboratory Diagnosis
- Gram Staining: Fecal smears may reveal curved Gram-negative bacilli that resemble commas, S-shapes, or spirals, similar to Vibrio.
- Dark Ground Microscopy: This technique shows the characteristic darting movement of the bacilli.
- Culture Media:
- Transport Medium: Cary-Blair medium is suitable.
- Selective Media: Includes Skirrow’s, Butzler’s, and Campy BAP selective media.
- Culture Conditions: Microaerophilic conditions (5% O2 ) and thermophilic temperatures (42°C) are required for most species, except for C. fetus, which is non-thermophilic.
Treatment
- Fluid and electrolyte replacement is the primary treatment method.
- Antibiotics may also be administered as needed.
- For diarrheal disease, the preferred medications are oral macrolides, specifically:
- Erythromycin
- Azithromycin
- In cases of systemic infection, the recommended treatments include:
- Parenteral gentamicin
- Imipenem
- Chloramphenicol
Helicobacter
Helicobacter pylori is a type of curved, gram-negative bacterium that resides in the stomach. It is associated with conditions like peptic ulcer disease and stomach cancer.
Pathogenesis
- Colonization: About 50% of people worldwide have H. pylori living in their stomachs, with 30% in developed countries and almost 80% in developing nations.
- Adhesins: A small number of strains, around 2%, attach to the stomach's mucosal lining by producing:
- Blood group antigen-binding adhesion: This binds to the Lewis blood group antigen.
- Adherence-associated lipoprotein: Another protein that helps with attachment.
- Induction of pathological changes: The bacteria cause harmful effects by making toxins, including:
- Vacuolating Cytotoxin (VacA): This toxin leads to the creation of vacuoles within the cytoplasm of epithelial cells.
- Cytotoxin-associated Gene A (cagA): Another important factor linked to the harmful effects of the bacteria.
- Molecular Mimicry: The lipopolysaccharide (LPS) of Helicobacter pylori can mimic the Lewis blood group antigen. This mimicry contributes to chronic active gastritis.
- Environmental Risk Factors:
- Smoking: In individuals infected with Helicobacter pylori, smoking increases the risk of developing ulcers and stomach cancer.
- Diet: diet high in salt and preserved foods increases the risk of stomach cancer. In contrast, antioxidants and vitamin C may offer protective effects.
Clinical Manifestations
- Acute gastritis: The most common area affected is the antrum, while the cardiac end is not involved.
- Antral gastritis: This type can lead to duodenal ulcers.
- Pangastritis: This condition can increase the risk of stomach adenocarcinoma.
- Peptic ulcer disease: Around 80% of duodenal ulcers and 60% of gastric ulcers are caused by H. pylori.
- Chronic atrophic gastritis: A long-term inflammation of the stomach lining that can worsen health.
- Autoimmune gastritis: The immune system attacks the stomach lining.
- Pernicious anemia: A condition promoted by autoimmune gastritis that affects vitamin B12 absorption.
- Adenocarcinoma of the stomach: A type of cancer that can develop in the stomach.
- Non-Hodgkin's gastric lymphoma: A type of cancer that affects the stomach's lymphatic tissue.
- Protective role of H. pylori: Infection with H. pylori, especially certain strains like cagA, is linked to a lower risk of:
- Gastroesophageal reflux disease (GERD)
- Barrett's esophagus
- Adenocarcinoma of the esophagus
- Asthma
Laboratory Diagnosis
Invasive Tests:
Endoscopy allows for the collection of multiple biopsies from the gastric mucosa, specifically from the antrum and corpus. These biopsies are analyzed through:
- Histopathology using Warthin Starry silver staining.
- Microbiological methods include:
- Gram staining: This shows curved, gram-negative bacilli that have a seagull shape.
- Culturing for H. pylori: This is the most specific test, but it lacks sensitivity.
- Media for Campylobacter can be used, such as Skirrow’s media.
- Chocolate agar can also be utilized.
- Plates should be incubated at 37°C under microaerophilic conditions.
Noninvasive Tests:
- Urea Breath Test: This test is popular because it is noninvasive and highly sensitive. It is also useful for monitoring treatment, as it becomes negative after successful treatment.
- Stool Antigen Assay: This test, also known as coproantigen assay, is used for monitoring treatment and screening children.
- Antibody Detection by ELISA: This test detects IgG antibodies against Helicobacter pylori and is used for screening before endoscopy and sero-epidemiological studies.
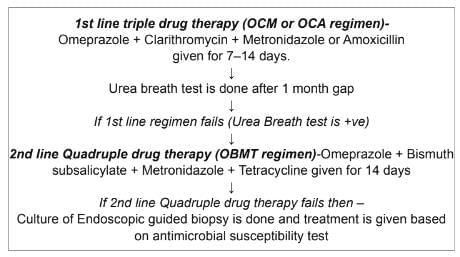
Treatment Regimen for H.pylori Infection
- H. pylori infections require treatment in cases of:
- Duodenal or gastric ulcers
- Low-grade gastric B cell lymphoma
- Treatment is not recommended for:
- Asymptomatic colonizers
- Primary prevention of gastric cancer due to potential side effects and antibiotic resistance
Legionella
- Legionellae are delicate, gram-negative bacteria that appear as short rods.
- They are linked to two main types of respiratory illnesses: Pontiac fever and Legionnaires’ disease.
- The majority of cases are caused by serogroup 1, with serogroup 4 and serogroup 6 being less common.
- Other species of Legionella rarely infect humans, including L.micdadei, known as the Pittsburgh pneumonia agent (which is acid-fast), and L.longbeachae.
Epidemiology
- Reservoir: Legionella thrives in various water environments, including:
- Natural water sources like rivers and amoebae.
- Artificial sources such as air conditioners and water coolers.
- Transmission:
- Aspiration can happen through oropharyngeal colonization or by directly drinking contaminated water.
- Aerosols can come from contaminated air conditioners, nebulizers, and humidifiers.
- There is a risk of direct instillation into the lungs during procedures that involve the respiratory tract.
- There is no person-to-person transmission, no animal reservoir, and no carriers for this condition.
Pathogenesis
- After Legionellae enter the lungs through aspiration or direct inhalation:
- Attachment and invasion to the respiratory mucosa.
- Coiling phagocytosis: Macrophages engulf Legionellae using a coiling method.
- Legionella avoids being killed inside cells by stopping the fusion of the phagosome and lysosome.
Clinical Manifestations
- Pontiac Fever: A sudden illness that feels like the flu.
- Legionnaires’ Disease(Pneumonia): This is a type of atypical pneumonia:
- It is the fourth most common cause of community-acquired pneumonia, making up 2-9% of cases.
- It causes 10-50% of nosocomial pneumonia, with serogroup 6 being frequently involved in hospital outbreaks.
- Extrapulmonary Legionellosis:
- The most common site outside the lungs is the heart, causing conditions like myocarditis, pericarditis, and prosthetic-valve endocarditis.
- Other manifestations include sinusitis, peritonitis, pyelonephritis, and skin and soft tissue infections.
Laboratory Diagnosis
- Gram stain shows many neutrophils but usually no organisms, as they are weakly stained and often missed.
- Direct fluorescent antibody (DFA) testing.
- Culture: Using Buffered charcoal yeast extract (BCYE) agar is the recommended method.
- Antibody Detection: Used mainly for epidemiological purposes.
- Urinary Antigen testing:
- It is quick, inexpensive, and easy to do.
- It stays positive even after antibiotics are given.
- Besides culture, it is highly sensitive and specific.
- PCR is useful for isolating Legionella from environmental water.
Treatment
The preferred antibiotics for treating Legionella infections are macrolides (such as azithromycin) and respiratory quinolones.
Calymmatobacterium Granulomatis
- Granuloma inguinale is also known as Granuloma venereum or Donovanosis.
- The current name for the agent causing this condition is Klebsiella granulomatis.
- Clinical Features:
- Painless Ulcer: This condition presents as a beefy red ulcer that tends to bleed easily.
- No Lymphadenopathy: There is no swelling of the lymph nodes, but pseudobubos may occur due to the presence of a subcutaneous abscess.
- Donovan Bodies: When stained with Wright's or Giemsa, these appear as large, cyst-like macrophages filled with deeply stained bacteria that have a safety-pin or bipolar appearance.
- Culture: The bacteria can be cultured using embryonated hens' eggs or on HEp-2 cell lines.
- Treatment: The drug of choice (DOC) for treatment is Azithromycin. Alternatives include Cotrimoxazole, Erythromycin, and Tetracycline.
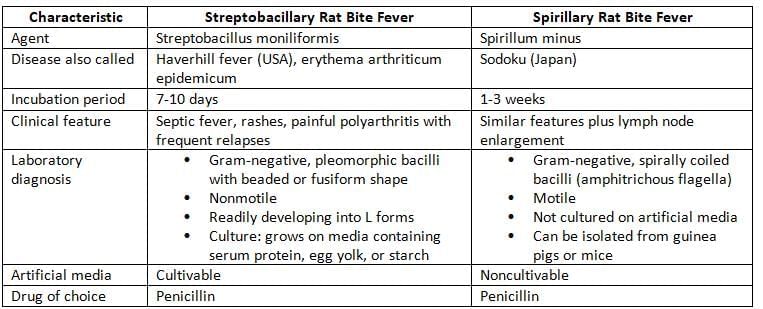
Rat Bite Fever
Gardnerella vaginalis
- Gardnerella vaginalis is responsible for causing bacterial vaginosis.
- It is a gram-variable organism, primarily gram-negative coccobacilli, and is characterized by the presence of metachromatic granules.
- Other organisms associated with bacterial vaginosis include:
- Mycoplasma hominis
- Mobiluncus
- Prevotella
- Ureaplasma
- Peptostreptococcus
- Amsel’s Criteria: Bacterial vaginosis is diagnosed when at least 3 out of the following 4 criteria are met:
- Profuse, thin (low viscosity), white, homogeneous vaginal discharge.
- Vaginal discharge pH > 4.5, indicating a decrease in Lactobacilli.
- Strong fishy odour when vaginal secretions are mixed with a 10% KOH solution (Whiff test).
- Presence of clue cells: Vaginal epithelial cells covered with coccobacilli.
- Nugent’s score assesses the levels of Gardnerella vaginalis, Mobiluncus, and Lactobacilli in a Gram-stained smear of vaginal discharge. A score of ≥ 7 indicates bacterial vaginosis.
- Treatment: Metronidazole is the preferred medication.
Pasteurella multocida
- Common organism: Often found in wounds caused by bites from cats and dogs.
- Clinical findings:
- Can lead to wound infections, swelling in lymph nodes, and respiratory infections.
- Laboratory diagnosis:
- Identified as nonmotile gram-negative coccobacilli with a bipolar staining pattern.
- They look like yersiniae, but differ in the following ways:
- Oxidase-positive and indole positive.
- Do not grow on MacConkey agar.
- Treatment: The preferred medication for P. multocida infections is Penicillin G.
Francisella tularensis (Tularemia)
- Transmission: Direct contact with rodents > Tick bite > Inhalation and ingestion
- Subspecies: F.tularensis has four subspecies:
- tularensis
- holarctica
- novicida
- mediasiatica: Found in central Asia
- The first three subspecies are found in North America.
- tularensis is the most common and the most harmful.
- Clinical Manifestations: Tularemia shows different symptoms:
- Ulceroglandular tularemia: Causes an ulcer at the infection site with swollen lymph nodes.
- Pulmonary tularemia
- Oropharyngeal tularemia and Lemming fever in Norway
- Oculoglandular tularemia
- Typhoid-like illness
- Agent of bioterrorism (classified as class A).
- Laboratory Diagnosis:
- Small gram-negative coccobacillus with a bipolar shape, nonmotile, and has a capsule.
- It is filterable, requires specific nutrients, and is an obligate aerobe.
- Media: Francis blood dextrose cysteine agar is used for culture.
- Detecting antibodies is the main method for diagnosis.
- Treatment: Gentamicin is the preferred medication.
Chromobacterium violaceum
It lives in water and soil in tropical areas.
- It can sometimes lead to skin problems, blood infections, and abscesses in the liver.
- It is a moving, gram-negative bacterium that can grow without oxygen, is non-spore forming, and has a shape like a short rod.
- It creates a unique violet pigment that does not spread in its environment, known as violacein.
Capnocytophaga Species
- Several types of bacteria, including C. ochracea, C. gingivalis, and C. sputigena, are part of the normal bacteria found in the human mouth.
- These bacteria can sometimes lead to periodontal diseases and can cause sepsis in people with weakened immune systems.
- Other species, like C. canimorsus and C. cynodegmi, are normally found in the mouths of dogs and can be spread through dog bites.
- Laboratory diagnosis:
- These bacteria are fusiform or filamentous and appear as gram-negative coccobacilli.
- They are very picky and need carbon dioxide to grow well.
- They produce a yellow-orange pigment.
- They do not have flagella but can move by gliding on the surface of agar.
- Treatment: Because these bacteria can produce β-lactamases, the best choice for treatment is ampicillin-sulbactam.
|
75 docs|5 tests
|
FAQs on Miscellaneous Bacteria Chapter Notes - Microbiology - NEET PG
| 1. What is Listeria monocytogenes and what diseases does it cause? |  |
| 2. What are Actinomycetes and their significance in medicine? |  |
| 3. How does Tropheryma whipplei cause Whipple's disease? |  |
| 4. What is Erysipelothrix rhusiopathiae and what conditions does it cause? |  |
| 5. What are the key characteristics of Campylobacter and its associated infections? |  |















