Mycology Chapter Notes | Microbiology - NEET PG PDF Download
| Table of contents |

|
| Classification of Fungi |

|
| Superficial Mycoses |

|
| Subcutaneous Mycoses |

|
| Systemic Mycoses |

|
| Opportunistic Mycoses |

|
| Penicillium |

|
| Mycotoxicosis |

|
Classification of Fungi
Fungi can be classified in two ways: Morphological Classification and Taxonomical Classification.
Morphological Classification
- Yeast: Round to oval cells that reproduce by budding. Examples include Cryptococcus neoformans and Saccharomyces.
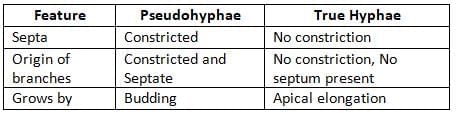
- Yeast-like fungi: Yeasts with structures called pseudohyphae, such as Candida.
- Molds: Long branching filaments known as hyphae, which are 2–10 µm wide. Examples are Dermatophytes, Aspergillus, Penicillium, Rhizopus, and Mucor.
- Dimorphic fungi: Exist as molds at room temperature (25°C) and as yeasts in the human body at 37°C. Examples include:
- Histoplasma capsulatum
- Blastomyces dermatitidis
- Coccidioides
- Paracoccidioides
- Penicillium marneffei
- Sporothrix schenckii
Taxonomical Classification
- Zygomycota: Lower fungi that produce zygospores and have aseptate hyphae, such as Rhizopus, Mucor, and Absidia.
- Ascomycota: Create ascospores and have septate hyphae, for example, Aspergillus.
- Basidiomycota: Produce basidiospores, such as Cryptococcus.
- Deuteromycota (Fungi Imperfecti): The sexual stage is either absent or not identified, which includes most medically important fungi.
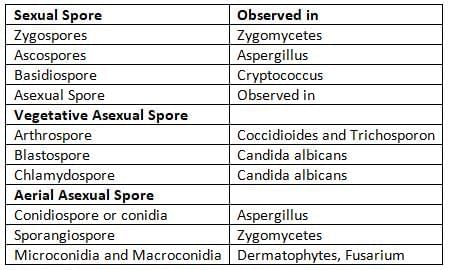
Types of fungal spores
Classification of Fungal Diseases
- Superficial mycoses:
- Tinea versicolor
- Tinea nigra
- Piedra
- Dermatophytosis
- Subcutaneous mycoses:
- Mycetoma
- Sporotrichosis
- Chromoblastomycosis
- Rhinosporidiosis
- Systemic mycoses:
- Histoplasmosis
- Blastomycosis
- Coccidioidomycosis
- Paracoccidioidomycosis
- Opportunistic mycoses:
- Candidiasis
- Cryptococcosis
- Zygomycosis
- Aspergillosis
- Penicilliosis
- Pneumocystis
- Fusariosis
- Mycotoxicoses:
Superficial Mycoses
Tinea Versicolor or Pityriasis Versicolor
- Tinea Versicolor, also known as Pityriasis Versicolor, is a persistent skin condition that impacts the outer layer of the skin.
- It is caused by a fungus called Malassezia furfur, which is a type of yeast naturally found on the skin.
- The condition is characterized by the appearance of scaly patches on the skin that can be either lighter or darker than the surrounding skin, particularly in warm and humid environments.
- These patches typically do not cause inflammation or itching, although there are instances where they may itch slightly.
- Tinea Versicolor commonly affects areas of the body with a high concentration of oil glands, such as the neck, chest, and upper arms.
Other manifestations include:
- Seborrheic dermatitis: Also known as dandruff in adults and cradle cap in babies.
- Atopic dermatitis, folliculitis (an infection of hair follicles), and disseminated infection.
Laboratory diagnosis: Diagnosis is mainly based on clinical examination.
- 10% KOH mount: Shows a mix of budding yeasts and short septate hyphae, often described as a spaghetti and meatballs appearance.
- SDA culture with olive oil overlay: Produces colonies that resemble fried eggs.
- Wood’s lamp examination: Scaly lesions display golden yellow fluorescence.
Treatment: Use topical lotions such as selenium sulfide shampoo, ketoconazole shampoo or cream, and terbinafine cream for 2 weeks.
Tinea Nigra
Tinea nigra is characterized by painless, black, non-scaly patches on the palms and soles. This condition is more prevalent in females and is caused by a black yeast-like fungus known as Hortaea werneckii.
Piedra
Piedra is distinguished by the presence of nodules on the hair shaft, which can be either black or white.
- White Piedra: This condition results in the formation of white nodules on the hair shaft, which are not very securely attached.
- Agent:Trichosporon beigelii
- Identifying feature: This fungus is urease positive and produces creamy white colonies. It contains hyaline septate hyphae interspersed with rectangular arthrospores.
- Black Piedra: This condition leads to the creation of black nodules that are firmly attached to the hair shaft.
- Agent: Piedraia hortae
- Identifying feature: This is a phaeoid fungus that produces reddish-brown colonies, featuring dark brown thick septate hyphae. These hyphae contain ascus with ascospores.
Dermatophytoses
Dermatophytoses, commonly referred to as tinea or ringworm, are the most prevalent superficial fungal infections affecting keratinized tissues. The causative agents include:
- Trichophyton species: These fungi infect the skin, hair, and nails.
- Microsporum species: These fungi primarily infect the skin and hair.
- Epidermophyton species: These fungi infect the skin and nails.
Dermatophytes are categorized based on their typical habitat:
- Anthropophilic species: These species infect only humans and are the most common type of dermatophyte infection in humans. They often cause mild, chronic lesions that are challenging to treat.
- Geophilic species: These species are found in soil and, along with zoophilic species (which infect animals), tend to cause more severe infections but typically resolve more quickly.
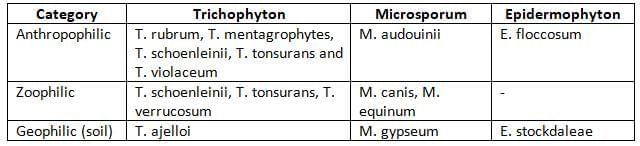
Classification of dermatophytes based on their usual habitat
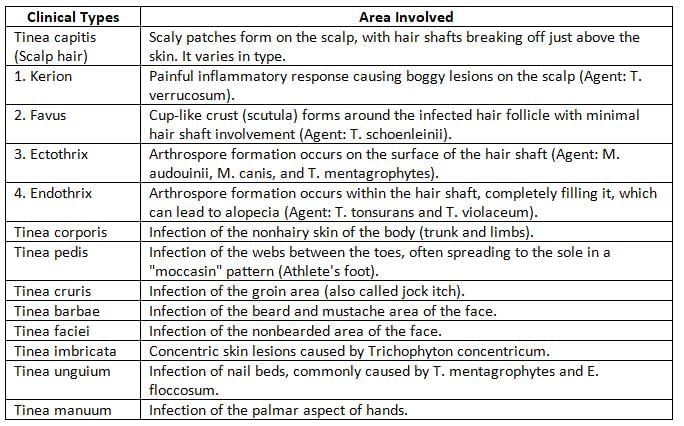
Clinical types of dermatophytoses
Dermatophytid or ID reaction
- Occasionally, some people may become hypersensitive to dermatophyte antigens. This can cause a secondary rash in those who are already sensitized due to the presence of allergenic products in their system.
- These secondary lesions are different from the original ringworm infections as they appear farther away from the initial site of infection. Additionally, fungal cultures often test negative for these secondary lesions.
Laboratory Diagnosis
- Woods lamp examination: Some dermatophytes emit a glow when viewed under a Woods lamp.
- This glow is caused by the presence of pteridine pigment in their cell walls.
- The test is positive for various Microsporum species and Trichophyton schoenleinii but negative for other dermatophytes.
- Specimen collection: Skin scrapings, broken or scaly hair, and nail clippings are collected from the active edge of the lesion and placed in folded black paper.
- Direct examination (using a 10% KOH mount): This shows thin, septate, hyaline hyphae along with arthroconidia.
- Culture on SDA followed by an LPCB mount of the colonies: This reveals two types of spores, macroconidia and microconidia, which help in identifying the species.
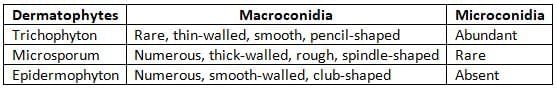
Distribution of conidia of dermatophytes
- Other methods of diagnosis
- The hair perforation test shows positive results for Trichophyton mentagrophytes and Microsporum canis.
- The urease test is positive for Trichophyton mentagrophytes.
- Dermatophyte test medium and dermatophyte identification medium can be utilized.
- PCR (Polymerase Chain Reaction) can help find specific genes related to the species, such as the chitin synthase gene.
- A skin test can be conducted to check for hypersensitivity to dermatophyte antigens like trichophytin.
- Treatment
- The preferred medications are oral terbinafine or itraconazole. The treatment duration is typically:
- 1 to 2 weeks for skin infections,
- 6 weeks for infections of the hair,
- 3 months for onychomycosis (nail infections).
- Alternatives include oral griseofulvin and ketoconazole.
- Topical lotions, such as Whitfield ointment or tolnaftate, can also be used.
- The preferred medications are oral terbinafine or itraconazole. The treatment duration is typically:
Subcutaneous Mycoses
Mycetoma
- Mycetoma is a long-lasting infection that causes a growth in the skin and the tissue just beneath it.
- The main signs of this condition are:
- Swelling in the affected area,
- Discharging sinuses that leak fluid, and
- Presence of granules in the fluid that comes out.
- There are two main types of mycetoma, which are:
- Eumycetoma, caused by true fungi,
- Actinomycetoma, caused by actinomycetes, which are a type of bacteria.
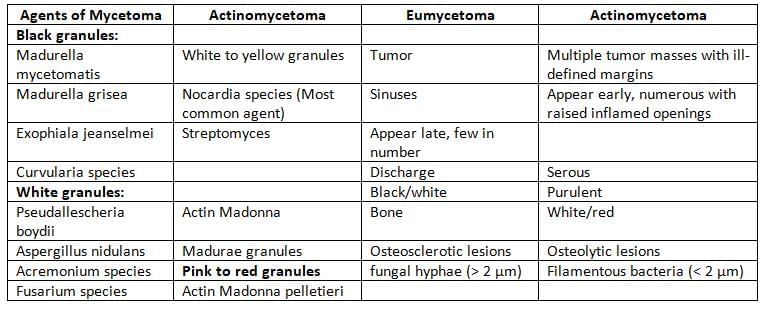
Agents and clinical manifestations of mycetoma
Epidemiology
- Mycetoma is commonly found in Africa, India, and the Central and South Americas.
- Globally, actinomycetoma is more frequent, making up 60% of cases, while eumycetoma accounts for 40%.
- Eumycetoma is more prevalent in Africa.
- In India, the state of Rajasthan has the highest number of mycetoma cases annually, followed by Tamil Nadu and West Bengal.
- In India, actinomycetoma is the most common type, present in 65% of cases, except in Rajasthan, where eumycetoma is more frequent.
Laboratory Diagnosis
- Direct Examination involves washing granules in sterile saline, crushing them between two slides, and examining them.
- For macroscopic appearance, assess granules for their color, size, shape, and texture.
- If eumycetoma is suspected, perform a KOH mount which shows hyphae measuring 2–6 µm.
- If actinomycetoma is suspected, conduct Gram staining to reveal filamentous Gram-positive bacilli that are 0.5–1 µm wide. If Nocardia is suspected, a modified acid-fast stain is needed as it is partially acid-fast.
- Histopathological staining of granules shows:
- Eumycetoma: Displays a granulomatous reaction with hyphae arranged in a palisade formation in the cement substance.
- Actinomycetoma: Shows a granulomatous reaction with filamentous bacteria on the edges.
Culture
- Granules taken from deep biopsies provide the best samples for culture.
- Use both fungal media (e.g., SDA) and Lowenstein Jensen media for Nocardia.
Treatment
Treatment for mycetoma involves surgically removing the affected area, followed by:
- Using antifungal agents for eumycetoma, such as itraconazole or amphotericin B for 8–24 months.
- Administering antibiotics for actinomycetoma, following the Welsh regimen (combining amikacin with cotrimoxazole).
Sporotrichosis
Sporotrichosis, commonly known as Rose Gardener's Disease, is a long-lasting disease that affects the skin and is characterized by the presence of pus-filled lumps. It is caused by a type of fungus called Sporothrix schenckii, which can change form depending on the temperature. This disease can show up in different ways.
- Painless nodulo-ulcerative lesions that spread through the lymphatic system
- Swollen lymph nodes that may become filled with pus and harden
- Less common forms include:
- Osteoarticular type
- Pulmonary type
- Disseminated sporotrichosis
Epidemiology
- Common in tropical countries with high humidity, such as South Africa and India.
- In India, sporotrichosis is mainly found in the hilly regions of sub-Himalayan areas, stretching from Himachal Pradesh to Assam.
- Risk factors include individuals who walk barefoot, such as farmers and gardeners.
Laboratory Diagnosis
- Direct microscopy using H and E staining of tissue samples shows cigar-shaped asteroid bodies.
- These bodies are identified as a central basophilic yeast cell surrounded by an eosinophilic mass, which is made up of antigen-antibody complexes.
- The surrounding eosinophilic area is known as the Splendore-Hoeppli phenomenon.
- Culture: Samples are placed on SDA and kept at 25°C and 37°C.
- At 25°C: It grows in a mycelial form, which features thin hyphae with conidia that are arranged in a flower-like pattern.
- At 37°C: It develops into a yeast form, noted for its moist, creamy white colonies.
- Serology: The latex agglutination test is used to detect antibodies in the serum of patients who have the extracutaneous form.
- A skin test can show a delayed hypersensitivity reaction to the sporotrichin antigen.
Treatment
- Itraconazole is the drug of choice for most cases.
- For disseminated infections, amphotericin B is the drug of choice.
Chromoblastomycosis
Chromoblastomycosis is a slowly developing chronic skin condition that causes subcutaneous lesions. It is caused by a group of fungi known as dematiaceous or phaeoid fungi, which are fungi that are pigmented darkly. These fungi create a specific structure referred to as sclerotic body.
- Causing agents: The fungi responsible for this condition include:
- Fonsecaea pedrosoi
- Phialophora verrucosa
- Cladosporium carrionii
- Rhinocladiella aquaspersa
- Types of lesions: The lesions can appear in several forms, including:
- Verrucose type (the most common)
- Crusted
- Ulcerative
- Nodular
- Sclerotic bodies: These are thick-walled, round cells that range in size from 5 to 12 micrometers. They have multiple internal partitions and are also known as Medlar bodies or muriform cells.
- Treatment: The treatment usually involves removing the lesion through surgical methods such as cryosurgery or laser therapy. After the surgery, antifungal medications like itraconazole are given to aid recovery.
Phaeohyphomycosis
- Phaeohyphomycosis is a condition characterized by long-lasting skin problems caused by certain types of fungi known as dematiaceous or phaeoid fungi.
- These fungi are different from those that cause chromoblastomycosis, as they do not produce sclerotic bodies.
- They primarily exist in a hyphal form, which means they grow as long, thread-like structures.
- Some of the main fungi responsible for this condition include:
- Alternaria
- Bipolaris
- Curvularia
- Exophiala jeanselmei
- Another important fungus is Cladophialophora bantiana, which is known to affect the nervous system and can lead to brain abscesses, particularly impacting the frontal lobe.
Rhinosporidiosis
- Rhinosporidiosis is a long-lasting granulomatous condition marked by large, soft polyps found mainly in the nose. It can also occur in the conjunctiva and sometimes in the ears, larynx, bronchus, and genitalia.
- Agent: This disease is caused by Rhinosporidium seeberi, which has recently been reclassified as an Aquatic Protistan Parasite (Mesomycetozoa). It was previously thought to be a type of lower aquatic fungi.
- Source: The primary source of infection is stagnant water. People can inhale fungal spores while bathing in ponds and rivers.
- Distribution: This disease is mainly found in tropical countries, particularly in Sri Lanka and parts of India, including Tamil Nadu, Kerala, Orissa, and Andhra Pradesh.
- Diagnosis:
- The histopathology of the polyp shows spherules, which are large sporangia filled with many endospores.
- R. seeberi has not yet been successfully cultivated in the lab.
- This organism is better stained with mucicarmine stain.
- Treatment: The main treatment is radical surgery combined with cauterization. The medication Dapsone has shown effectiveness. However, the disease often recurs.
Systemic Mycoses
- All four types of fungi that lead to systemic mycoses can change their form, which is called dimorphic.
- These fungi are spread through the inhalation of spores.
- Once the spores enter the lungs, they change into their yeast phase.
- The most common effect of these fungi occurs in the lungs, known as the pulmonary manifestation.
Histoplasmosis
Histoplasmosis, also referred to as Darling’s disease, is caused by the dimorphic fungus Histoplasma capsulatum, which exists in three biovars:
- H. capsulatum var. capsulatum: Responsible for classical histoplasmosis, the most prevalent type.
- H. capsulatum var. duboisii: Causes African histoplasmosis, often affecting the skin and bones.
- H. capsulatum var. farciminosum: Leads to epizootic histoplasmosis, primarily in horses and mules.
Epidemiology:
- Histoplasmosis is commonly found in the USA, particularly in the Ohio River Valley and lower Mississippi River regions.
- In India, it is frequently reported in West Bengal along the Ganga River.
- Reservoir: Humid, acidic soil enriched with bird or bat droppings.
- Transmission: Inhalation of spores (microconidia) from contaminated soil.
Clinical Manifestations:
- Pulmonary histoplasmosis: Most common form, initially presenting as a mild flu-like illness.
- Chronic cavitary histoplasmosis: Severe form characterized by cavitary lesions.
- Mucocutaneous oral lesions: Particularly observed in Indian patients.
- Disseminated histoplasmosis: Occurs in individuals with severely compromised cellular immunity, such as HIV patients.
Diagnosis:
- Histopathological staining reveals small oval yeast cells (2-4 µm) with narrow-based budding within macrophages, accompanied by a granulomatous response.
- Culture is the gold standard for diagnosis, with Histoplasmabeing dimorphic:
- At 25°C: Produces white mycelial colonies with thick tuberculate macroconidia and thin microconidia.
- At 37°C: Converts to yeast form (creamy white colonies) in specialized Kelley’s media.
- Serological Tests: Antibodies can be detected in serum using Complement Fixation Test (CFT) and immunodiffusion tests. A skin test may indicate delayed-type hypersensitivity.
Treatment:
- Liposomal amphotericin B: Preferred for acute pulmonary and disseminated histoplasmosis.
- Itraconazole: Recommended for chronic cavitary pulmonary histoplasmosis.
Blastomycosis
Blastomycosis, also known as North American blastomycosis, Gilchrist’s disease, or Chicago disease, is caused by the dimorphic fungus Blastomyces dermatitidis.
- Clinical manifestations:
- Acute pulmonary: This is the most common form of the disease.
- Other manifestations:
- Skin lesions
- Osteomyelitis
- CNS involvement in AIDS patients (can lead to brain abscess)
- Epidemiology:
- Commonly found in North America, especially in states near the Ohio River and Mississippi River.
- Laboratory diagnosis:
- Histopathological staining: Examining tissue biopsy samples shows thick-walled round yeast cells, measuring 8–15 μm with a characteristic single broad-based budding, appearing like a figure of eight.
- Antibody detection: Using an immunodiffusion test to find antibodies against yeast phase antigens such as antigen-A, BAD-1, and ASWS antigen (alkali soluble water soluble).
- Antigen detection assay: This test is used to identify Blastomyces antigen in urine (more sensitive) and in serum.
- Treatment:
- The preferred medication is Liposomal amphotericin B.
- Itraconazole can be prescribed for immunocompetent patients with mild cases of blastomycosis.
Coccidioidomycosis
Coccidioidomycosis, also known as desert rheumatism, Valley fever, or California fever, is a systemic fungal infection caused by a soil fungus known as Coccidioides. This fungus has two species: C. immitis and C. posadasii.
- Clinical Manifestations
- Pulmonary coccidioidomycosis (main form). Other forms include skin lesions, erythema nodosum, and arthritis, particularly in women.
- Those at higher risk for disseminated infection include males and individuals with low cell-mediated immunity (for example, HIV patients with a CD4 count less than 250 cells/µL). Common areas affected by dissemination are the skin, bones, joints, soft tissues, and meninges.
- Epidemiology: This disease is commonly found in certain regions of Arizona, California, New Mexico, Texas, and Northern Mexico.
- Laboratory Diagnosis
- Histopathological staining of sputum or tissue biopsy samples shows spherules (large sac-like structures filled with endospores).
- Culturing the fungus on SDA results in mycelial growth characterized by fragmented hyphae and barrel-shaped arthrospores with distorted empty cells.
- Coccidioides is unique among dimorphic fungi because it can grow as mold at both 25°C and 37°C in standard culture media, and it forms spherules at 37°C in specific culture media.
- Cultures are highly infectious and must be handled with biosafety level-3 precautions.
- Serology: Antibodies can be detected using the immunodiffusion test and complement fixation test (CFT).
- Skin test with fungal extracts (coccidioidin or spherulin).
- Treatment: Itraconazole is the drug of choice (DOC) for treatment, while Amphotericin-B is used for severe pneumonia cases.
Paracoccidioidomycosis
Paracoccidioidomycosis, also referred to as South American blastomycosis or Lutz-Splendore-de Almeida disease, is a systemic infection caused by the dimorphic fungus Paracoccidioides brasiliensis. This fungus exists in soil and can infect humans, leading to various clinical manifestations.
- Clinical Manifestations
- Acute Form (Juvenile Type): This form primarily affects young adults under 30 years of age. It is less common but more severe, presenting as a disseminated infection that involves multiple organs and is challenging to treat.
- Chronic Form (Adult Type): The more prevalent form, accounting for 90% of cases, typically affects older men. It is usually less severe and manifests as progressive pulmonary disease, skin lesions, and cervical lymphadenopathy.
- Epidemiology: Paracoccidioidomycosis is endemic in countries such as Brazil and other regions of South America, where the fungus is present in the environment and can lead to infections in susceptible individuals.
- Laboratory diagnosis:
- Histopathological staining of pus, tissue biopsies, or sputum shows round, thick-walled yeasts that have several narrow-necked buds attached around them, resembling a Mickey Mouse or pilot wheel shape.
- When grown on SDA, the fungus shows a mycelial form at 25°C, and it changes into the yeast phase at 37°C.
- In serology, antibodies can be found using immunodiffusion methods, and more recently with ELISA, which uses the gp43 antigen.
- A skin test can show a delayed type hypersensitivity response to the paracoccidioidin antigen.
- Treatment
- Itraconazole is the preferred treatment for paracoccidioidomycosis, especially in cases that are not severe.
- Amphotericin B is recommended for seriously ill patients who require more aggressive treatment due to the severity of their condition.
Opportunistic Mycoses
Opportunistic mycoses are infections caused by fungi that usually live in the human body, like Candida, or are found in nature and often contaminate laboratory samples, such as Aspergillus, Rhizopus, and Penicillium.
Candidiasis
Candidiasis is a common fungal infection caused by Candida, a type of yeast that forms pseudohyphae. It is especially prevalent in individuals with weakened immune systems. The different species of Candida include:
- Candida albicans. The most common and pathogenic species.
- Other species include C. tropicalis, C. glabrata, C. krusei, C. parapsilosis, C. dubliniensis, C. kefyr, and C. viswanathii.
Pathogenesis
Factors that increase the risk of Candida infections include:
- Physiological state. Extremes of age (infancy and old age) and pregnancy.
- Low immunity. Individuals on steroids or immunosuppressive drugs, those who have undergone transplantation, have malignancies, or are HIV-positive.
- Use of broad-spectrum antibiotics, which can disrupt normal flora.
- Diabetes mellitus, febrile neutropenia, and deficiencies in zinc or iron.
Clinical Manifestations
Candida species are normally found on the skin and mucous membranes, including the gut. Under certain opportunistic conditions, they can cause various infections.
1. Mucosal Candidiasis:
- Oropharyngeal candidiasis, commonly known as oral thrush, presents as white, sticky, and painless spots inside the mouth.
- Candidal vulvovaginitis is characterized by a thin, whitish, curd-like discharge from the vagina.
- Balanitis and balanoposthitis primarily affect uncircumcised males.
- Esophageal candidiasis occurs in the throat.
- Angular stomatitis and denture stomatitis are also types of mucosal candidiasis.
- Chronic mucocutaneous candidiasis is observed in individuals with weakened immune systems and is challenging to treat.
2. Cutaneous Candidiasis:
- Intertrigo, paronychia, and onychomycosis (nail fungal infection).
- Diaper candidiasis in infants and perianal candidiasis.
- Erosio interdigitalis blastomycetica, an infection occurring between fingers or toes.
- Generalized disseminated cutaneous candidiasis in infants.
3. Invasive candidiasis refers to the spread of fungi through the bloodstream or locally, leading to various infections such as:
- Urinary Tract Infections (UTI), Pulmonary Candidiasis, Meningitis, Osteomyelitis, and Hepatosplenic and Disseminated Candidiasis
- Septicemia caused by Candida albicans and Candida glabrata
- Ocular Issues: Keratoconjunctivitis and Endophthalmitis
- Hospital-Acquired Candidiasis (mainly due to Candida glabrata)
4. Allergic Candidiasis
- Candidiasis: This condition is characterized by fluid-filled sores that develop in the spaces between the fingers. These sores resemble a dermatophytid reaction, and both candidiasis and dermatophytid reaction are known as 'ID' reactions.
- Allergic Reactions: Candidiasis can be associated with other allergic reactions, including:
- Gastritis: Inflammation of the stomach lining.
- Irritable Bowel Syndrome (IBS): A gastrointestinal disorder causing symptoms like abdominal pain and changes in bowel habits.
- Eczema: A skin condition causing itchy and inflamed skin.
Laboratory Diagnosis
- Direct Microscopy: This diagnostic method involves observing oval yeast cells that are gram-positive, measuring 4 to 6 micrometers in size, and exhibiting pseudohyphae.
- Culture on Sabouraud Dextrose Agar (SDA): When cultured on SDA, the colonies of Candida appear creamy white, smooth, pasty, and emit a typical yeasty smell.
- Species Identification Tests: These tests help identify specific Candida species, such as:
- Germ Tube Test: Also known as the Reynolds Braude phenomenon, this test is specific for Candida albicans.
- It is different from pseudohyphae because there is no narrowing at the point of origin.
- Although the test is specific for C. albicans, it can also show positive results for C. dublinensis.
- Dalmau Plate Culture on Cornmeal Agar: This method is used to produce thick-walled chlamydospores from C. albicans.
- CHROM Agar: Different species of Candida produce colonies of various colors on this agar, aiding in species identification.
- Growth at 45°C: This test helps differentiate between C. albicans, which grows well at this temperature, and C. dubliniensis, which does not.
- Sugar Fermentation Test and Sugar Assimilation Test: These tests are used to differentiate between C. albicans and other species based on their sugar fermentation and assimilation capabilities.
- Immunodiagnosis: Various immunodiagnostic methods can be used to detect antibodies, antigens, and enzymes specific to Candida infections. These methods include:
- Antibody Detection: Detecting antibodies against cell wall mannan antigen.
- Antigen Detection: Identifying cell wall mannan and cytoplasmic antigens using ELISA (Enzyme-Linked Immunosorbent Assay).
- Enzyme Detection: Detecting specific enzymes like enolase and aspartate proteinase associated with Candida.
- Metabolite Detection: Detecting metabolites specific to Candida, such as mannitol and arabinitol.
- G Test: Used for detecting α1-3 glucan, a specific marker for Candida infections.
Treatment
Antifungal Medications: The choice of antifungal medications depends on the type of candidiasis being treated:
- Cutaneous Candidiasis or Oral Thrush: The recommended medication is topical azole antifungals.
- Esophageal and Vulvovaginal Candidiasis: The preferred treatment is oral fluconazole.
- Disseminated Candidiasis: The drug of choice is Amphotericin B, a potent antifungal.
- C. glabrata and C. krusei: These species may exhibit resistance to certain azole antifungals, necessitating alternative treatment options.
Cryptococcosis
Cryptococcus has two main species: C. neoformans and C. gattii, and four serotypes: A, B, C, and D.
- C. neoformanshas two varieties:
- C. neoformans var. grubii - corresponds to serotype A.
- C. neoformans var. neoformans - corresponds to serotype D.
- C. gattii is diverse in its antigens and relates to serotypes B and C.
- Many labs do not differentiate between the species and simply report all samples as C. neoformans.
- Spread in the CNS: A unique feature of Cryptococcus is its ability to cross the blood-brain barrier. This occurs as yeast cells either move directly through the endothelium or are carried inside macrophages like a 'Trojan horse'.
- Virulence factors that help Cryptococcus invade and spread include:
- Polysaccharide capsule.
- Ability to produce melanin through the enzyme phenyl oxidase.
- Production of other enzymes, such as phospholipase and urease.
- Risk factors:Individuals at higher risk for cryptococcosis include:
- Patients with advanced HIV infection and CD4 T-cell counts less than 200/µl, which is the main risk factor for C. neoformans. However, C. gattii is not linked with HIV and can infect healthy individuals.
- Patients with hematologic malignancies.
- Transplant recipients.
- Patients undergoing immunosuppressive or steroid therapy.
Clinical Manifestations:
Various symptoms of cryptococcosis include:
- Pulmonary cryptococcosis is the most common type.
- Chronic meningitis.
- Skin lesions are often seen with C. neoformans var. neoformans (serotype D).
- Osteolytic bone lesions.
Epidemiology
- Geographical distribution: C. neoformans var. grubii (serotype A) can be found worldwide, while var. neoformans is mainly in Europe.
- Habitat: C. neoformans is commonly found in soils polluted with bird droppings, especially from pigeons. In contrast, C. gattii is found in eucalyptus trees.
Laboratory Diagnosis
Direct detection methods:
- Negative staining with modified India ink and nigrosin stain to show the capsule, which appears as a clear space around the yeast cells against a dark background. Sensitivity is between 60-70%.
- Gram staining may reveal Gram-positive round budding yeast cells.
- Other stains such as mucicarmine, Masson-Fontana, and Alcian blue can be used.
- Capsular antigen detection from CSF or serum can be done using the latex agglutination test, which is rapid and highly sensitive (95%).
- Confirming Cryptococcus species:
- Culturing on SDA: Colonies appear as mucoid, creamy-white yeast-like colonies.
- Niger seed agar and bird seed agar are used to check for melanin production.
- Grows at 37°C, and is urease test positive.
- Has the ability to assimilate inositol and nitrate, and shows positive results in the mouse pathogenicity test.
Treatment
The treatment varies based on the type of cryptococcosis.
- If there is no CNS involvement, Fluconazole is the preferred medication.
- For HIV-infected patients with CNS involvement, an induction phase lasting two weeks with Amphotericin-B plus flucytosine is recommended, followed by lifelong maintenance therapy with fluconazole.
Zygomycosis
Zygomycosis, also known as mucormycosis, refers to a group of serious infections caused by aseptate fungi in the phylum zygomycota. Common examples of these fungi include:
- Rhizopus
- Mucor
- Absidia
Predisposing Factors
The fungi responsible for mucormycosis need iron to grow. Therefore, conditions that lead to high iron levels increase the risk of invasive mucormycosis. The main risk factors include:
- Diabetic ketoacidosis (DKA) - This is the most significant risk factor.
- End-stage renal disease
- Patients receiving iron therapy or deferoxamine (an iron chelator)
- Defects in phagocytic functions (for example, neutropenia or use of steroids)
Clinical Manifestations
The fungi causing mucormycosis are known for invading blood vessels. There are six common types of clinical presentations:
- Rhinocerebral mucormycosis: This is the most common type, presenting as orbital cellulitis, proptosis, and vision loss.
- Pulmonary mucormycosis: The second most common form, often seen in patients with leukemia.
- Cutaneous mucormycosis: Involves skin infections.
- Gastrointestinal mucormycosis: Includes severe conditions like necrotizing enterocolitis, primarily observed in premature neonates.
- Disseminated mucormycosis: The brain is the most frequently affected site.
- Miscellaneous forms: Can affect various body parts, including bones, trachea, and kidneys.
Laboratory Diagnosis
- Histopathological staining: Tissue biopsies show broad, aseptate, hyaline hyphae with wide-angle branching.
- Culturing: On SDA at 25°C, the culture shows cottony, woolly colonies that start white and turn brown-black due to sporulation, resembling a salt-and-pepper appearance.
- Microscopic examination: An LPCB mount reveals broad, aseptate, hyaline hyphae from which sporangiophores extend, terminating in sporangia filled with numerous sporangiospores.
- Rhizoids: Some species have a unique root-like structure called rhizoids, which can help identify the fungus. The species can be differentiated based on the rhizoid position relative to the sporangiophore:
- Rhizopus: Has nodal rhizoids.
- Absidia: Has internodal rhizoids.
- Mucor: Lacks rhizoids.
Treatment
The preferred medication for all forms of mucormycosis is Amphotericin B deoxycholate, except for mild localized skin lesions in immunocompetent individuals, which can be treated through surgical removal.
Aspergillosis
Aspergillus species are commonly found on decaying plants and they create chains of conidia.
Risk Factors for Invasive Aspergillosis:
- Glucocorticoid use: This is the most significant risk factor.
- Profound neutropenia: This refers to a severe reduction in neutrophils or issues with their function.
- Underlying conditions: Includes pneumonia, Chronic Obstructive Pulmonary Disease (COPD), tuberculosis, or sarcoidosis.
- Antitumor necrosis factor therapy: Treatment that can increase risk.
Clinical Manifestations
The symptoms of aspergillosis vary depending on where the infection occurs. The incubation period can last from 2 to 90 days.
Types of Aspergillosis
- Pulmonary aspergillosis: This includes different forms such as:
- Allergic bronchopulmonary aspergillosis (ABPA)
- Asthma
- Extrinsic allergic alveolitis
- Aspergilloma (fungal ball)
- Chronic cavitary pulmonary aspergillosis
- Invasive sinusitis: This includes:
- Invasive sinusitis
- Chronic granulomatous sinusitis
- Maxillary fungal ball
- Allergic fungal sinusitis
- Ocular aspergillosis: This can lead to keratitis and endophthalmitis.
- Ear infection: Known as otitis externa.
- Other infections: These may include:
- Endocarditis
- Brain abscess
- Skin lesions
- Onychomycosis
Species Involved in Clinical Manifestations
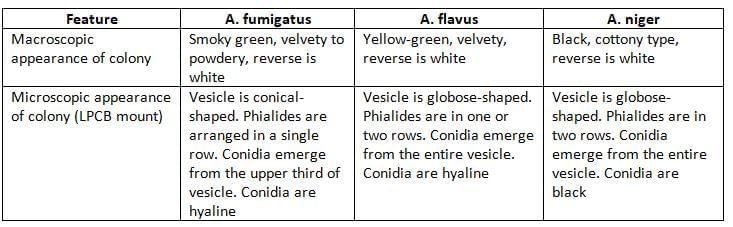
- A. fumigatus: This species is responsible for most cases of acute pulmonary and allergic aspergillosis.
- A. flavus: More frequently found in hospitals, it causes more sinus, skin, and ocular infections compared to A. fumigatus.
- A. niger: This species can cause invasive infections but more often colonizes the respiratory tract, leading to otitis externa.
Laboratory Diagnosis
- Direct examination: Shows narrow, septate, hyaline hyphae that branch at sharp angles.
- Culture on SDA: After culturing, colonies are examined using an LPCB mount (refer to the table).
- Antigen detection: Uses ELISA to find galactomannan antigen.
- Antibody detection: Helpful for diagnosing chronic invasive aspergillosis and aspergilloma, especially when cultures are often negative.
- In allergic conditions: In cases like allergic bronchopulmonary aspergillosis (ABPA) and severe asthma, levels of specific serum IgE are increased.
- Metabolite detection: Identifies substances like α1-3 glucan (through the G test) or mannitol.
Treatment
- For invasive aspergillosis: The preferred medication is voriconazole.
- For ABPA: Itraconazole is the recommended treatment.
- For a single aspergilloma: Surgery is the suggested approach.
- For chronic pulmonary aspergillosis: Itraconazole or voriconazole are the preferred drugs.
- For prophylaxis: Posaconazole is recommended.
Penicillium
Penicillium species are usually found in the environment and as laboratory contaminants. Rarely infects humans.
- Common manifestations: endophthalmitis, otomycosis, onychomycosis and allergic pneumonitis.
- Microscopy: Reveal hyaline thin septate hyphae, vesicles are absent, and conidia arranged as brush border appearance.
Penicillium Marneffei
- Penicillium marneffei is a thermally dimorphic fungus that causes opportunistic infection in HIV infected patients.
- Systemic infection mimicking that of dissociated histoplasmosis.
- Skin lesions: Warty lesions mimicking that of Molluscum contagiosum are seen.
- It is endemic in SE Asian countries including Thailand, Vietnam, and India (Manipur).
- P. marneffei is found mostly in rural areas and bamboo rats are the reservoirs of infection.
- Lab Diagnosis:
- Direct Microscopy: Shows oval or elliptical yeast cells with central septation, which indicates that these cells divide by transverse fission rather than budding.
- Culture: P. marneffei being dimorphic; produces yeast-like colonies at 37°C and mold form at 25°C. The mold form has a characteristic brick red pigment.
- Treatment: AIDS patients with severe penicilliosis are treated with amphotericin B till the condition improves followed by maintenance therapy with itraconazole for 12 weeks. In mild penicilliosis, itraconazole is recommended for 12 weeks.
Pneumocystis Pneumonia (PcP)
- Pneumocystis is categorized as a fungus based on studies of its nucleic acid sequences.
- It exists in two forms:
- In the environment, it is found as cysts.
- In human tissues, both cysts and trophozoites can be present.
- The cysts are inhaled and travel to the lungs.
- Once in the lungs, the cysts change into the trophozoite stage.
- This process triggers an inflammatory response in the body.
- The inflammatory response leads to the recruitment of plasma cells.
- The accumulation of plasma cells results in the formation of a frothy exudate that fills the alveoli.
- Because of this, Pneumocystis pneumonia is also referred to as plasma cell pneumonia.
Laboratory Diagnosis:
- Gomori’s methenamine silver (GMS) staining is the preferred method to show the cysts of P. jirovecii. The cysts appear like black, crushed ping-pong balls against a green background.
- Pneumocystis cannot be grown in a lab, and there is no blood test available to detect it.
- Treatment: Cotrimoxazole is the drug of choice for treating Pneumocystis pneumonia. It is prescribed for 14 days for patients who are not infected with HIV and for 21 days for those who are HIV-positive. This medication is also recommended for both primary and secondary prevention in HIV patients.
Fusariosis
Fusarium is a type of saprophyte and rarely causes infections in humans.
- In healthy individuals, it can cause:
- Keratitis in people who wear contact lenses.
- Onychomycosis (nail infection).
- In patients with weakened immune systems:
- It is angioinvasive and can cause infections in the lungs and sinuses.
- In patients who are neutropenic or have blood cancers, disseminated fusariosis can occur, often with skin lesions.
Lab Diagnosis: A mount using LPCB from the colony shows:
- Hyaline septate hyphae with round microconidia.
- Sickle-shaped large macroconidia and chlamydospores.
Treatment: Recommended treatments include:
- Liposomal amphotericin B
- Voriconazole
- Posaconazole
Mycotoxicosis
Mycotic poisoning can be classified into two varieties:
- Mycotoxicosis: This condition happens when a person eats food that is tainted with harmful substances released by certain types of fungi.
- Mycetism: This term describes the harmful effects that occur from consuming poisonous mushrooms, which are a type of fleshy fungus.
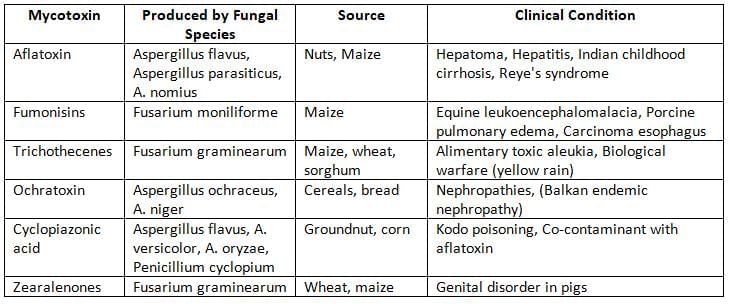
Features of Common mycotoxins
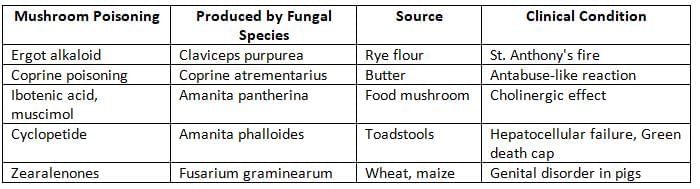
 Features of Common mycetism
Features of Common mycetism
|
75 docs|5 tests
|
FAQs on Mycology Chapter Notes - Microbiology - NEET PG
| 1. What is Tinea Versicolor and how does it manifest on the skin? |  |
| 2. How is Tinea Nigra diagnosed and what are its distinguishing features? |  |
| 3. What is Piedra and what types are recognized in mycology? |  |
| 4. What are dermatophytoses and how do they differ from other fungal infections? |  |
| 5. What laboratory methods are used for the diagnosis of fungal infections in dermatology? |  |



















