NEET PG Exam > NEET PG Notes > Microbiology > Chapter Notes: Neisseria and Moraxella
Neisseria and Moraxella Chapter Notes | Microbiology - NEET PG PDF Download
Introduction
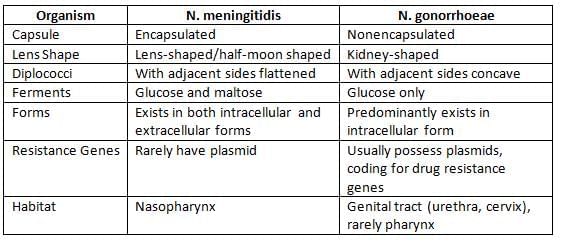
Gram-negative cocci encompass Neisseria, Moraxella catarrhalis, and Veillonella. Neisseria species are characterized as catalase and oxidase positive, non-motile, aerobic gram-negative diplococci.
- Among them, two species are harmful to humans: N. meningitidis and N. gonorrhoeae.
- The remaining species typically act as harmless residents in the intestines, genital tract, or oral cavity.
Meningococcal disease patterns:
- In Africa, epidemics are primarily caused by serogroup A, with occasional cases of serogroup W135.
- Outbreaks are attributed to serogroup C.
- Hyperendemic disease is linked to serogroup B.
- Sporadic cases can occur from all serogroups: A, B, C, Y, and W135.
- Gram-negative cocci encompass Neisseria, Moraxella catarrhalis, and Veillonella.
- Neisseriae are catalase and oxidase positive, non-motile, aerobic gram-negative diplococci.
- Harmful species to humans include N. meningitidis and N. gonorrhoeae, while some Neisseria species are harmless and reside in the intestine, genital tract, and oral cavity.
Neisseria Meningitidis (Meningococcus)
Virulence Factors
- Capsular Polysaccharide: This component helps the bacteria evade phagocytosis by immune cells. It can be classified into 13 serogroups, but only five serogroups— A, B, C, Y, and W135 —are responsible for most cases. Other capsular types and noncapsulated strains (16% of isolates) can be found in the nasopharynx of healthy carriers.
- Outermembrane Proteins: These proteins are used to classify serogroups into serotypes.
- Lipopolysaccharide and Endotoxin: These substances damage blood vessel linings, leading to increased vascular permeability, intravascular thrombosis, Waterhouse-Friderichsen syndrome, and myocardial dysfunction.
- IgA Proteases: These enzymes break down mucosal IgA.
- Transferrin Binding Protein: This protein helps the bacteria acquire iron from the host.
- Adhesins. These are mediated by OPA protein and pili, helping the bacteria adhere to host tissues.
Epidemiology
- Meningococcal disease affects nearly 500,000 people worldwide each year, with about 10% of those cases resulting in death.
- Disease patterns:
- Epidemics mainly occur in sub-Saharan Africa, primarily due to group A and W135 strains.
- Outbreaks often arise from serogroup C, particularly in semi-closed communities like schools and military camps.
- Hyperendemic disease (more than 10 cases per 100,000 people) is usually caused by serogroup B.
- Sporadic cases (ranging from 0.3 to 5 cases per 100,000 people) can be due to any of the strains: A, B, C, Y, and W135.
- High prevalence areas include the sub-Saharan belt of Africa, stretching from Ethiopia to Senegal.
- Seasonal variations are often seen during winter and spring, particularly in cold and dry climates.
- Age group: Meningitis is most common in young children, especially those between 3 months and 5 years old.
- Risk factors that increase the chance of colonization include:
- Overcrowding and living in semi-closed communities such as schools, military bases, and refugee camps.
- Travelers, especially Hajj pilgrims, and those who smoke.
- Viral and Mycoplasma infections of the respiratory tract.
- Risk factors that increase the likelihood of disease include:
- Deficiency of terminal complement components, specifically C5 to C9.
- Hypogammaglobulinaemia, a condition characterized by low levels of immunoglobulins in the blood.
- Hyposplenism, which is reduced function of the spleen.
Pathogenesis of Meningococcal Infection
- Source of Infection: The primary source of meningococcal infection is human nasopharyngeal carriers, with children being the most significant contributors.
- Carrier Rate: The rate of carriers can fluctuate, ranging from 5–10% during inter-epidemic periods to as high as 70–80% during epidemics.
- Transmission: Meningococcal infection spreads through inhalation of respiratory droplets.
- Spread of Infection: Meningococci can reach the meninges from the nasopharynx through several mechanisms:
- Hematogenous Spread: This is the most common method of infection spread.
- Direct Spread: Meningococci can directly spread via the olfactory nerve through the cribriform plate.
- Conjunctival Route: Although rare, infection can also occur through the conjunctiva.
- Case Fatality Ratio: The case fatality ratio is 80% in untreated individuals or specific populations but decreases to 10% with early treatment.
Clinical Manifestations
- Asymptomatic colonization is the most frequent occurrence.
- Rashes: non-blanching rash, either petechial or purpuric, is present in over 80% of cases.
- Septicemia: Caused by endotoxin-induced damage to blood vessels.
- Waterhouse-Friderichsen syndrome: severe complication of meningococcemia characterized by large purpuric rashes (purpura fulminans), shock, disseminated intravascular coagulation (DIC), adrenal gland hemorrhage, and multi-organ failure.
- Pyogenic meningitis: Typically affects young children between 3 to 5 years old.
- Chronic meningococcemia: rare form presenting with a petechial rash, fever, arthritis, and splenomegaly.
- Postmeningococcal reactive disease: Occurs 4 to 10 days later due to immune complexes, leading to arthritis, rash, iritis, pericarditis, polyserositis, and fever.
Diagnosis in the Laboratory
- Laboratory Diagnosis
- Specimen:
- For affected individuals: Blood and CSF
- For carriers: Nasopharyngeal swab
- CSF examination:
- The first part is spun down and used for:
- Capsular antigen detection
- Biochemical analysis: Increased CSF pressure, increased protein, and decreased glucose in CSF
- Gram staining: Shows pus cells with gram-negative diplococci, which are lens-shaped
- The second part is used for cultures on blood agar and chocolate agar
- The third part is enriched in BHI broth and incubated for 7 days
- The first part is spun down and used for:
- Nasopharyngeal swab culture: Grown on Thayer Martin medium
- Biochemical tests:
- Oxidase and catalase positive
- Can ferment glucose and maltose but not sucrose
- Serogrouping: Done using a latex agglutination test
- Serology: Detects antibodies to capsular antigen (using ELISA), helpful for looking back at previous cases of the disease
- Molecular diagnosis: Performed using multiplex PCR
- Specimen:
Treatment of Meningococcal Infections
- Drug of Choice (DOC) for treatment: Ceftriaxone and Cefotaxime
- DOC for carriers and prophylaxis: Ceftriaxone
- Alternatives for carriers and prophylaxis: Rifampicin and Ciprofloxacin
Vaccine
A polyvalent vaccine that covers four groups: A, C, Y, and W135.
- No vaccine for Group B:
- The capsule for Group B is made of sialic acid residues, which can cause brain inflammation and is not very effective at generating an immune response.
- Research on outer membrane vesicle (OMV) based vaccines for Group B is currently underway.
- Dose:
- A single dose of 50 µg is administered.
- Immunity begins within 10 days and lasts for up to 3 years.
- Indication:
- This vaccine is recommended for travelers, especially those going on the Hajj pilgrimage.
- Contraindications:
- The vaccine is not recommended for pregnant women and children under 3 years old because the capsule is poorly immunogenic for those under 3.
Neisseria Gonorrhoeae (Gonococcus)
N. gonorrhoeae is a type of bacteria that is shaped like a kidney bean and is found in pairs (diplococcus). It is Gram-negative, which means it does not have a protective outer capsule.
Virulence Factors
- Pili or fimbriae: The main factor for causing disease, aids in sticking to surfaces and prevents being engulfed by immune cells.
- Outer membrane proteins:
- Porin (protein I): These create small channels (pores) in the membrane.
- Two main types:
- Por B.1A: Linked with local and widespread gonococcal infections (DGI).
- PorB.1B: Typically causes local genital infections.
- Opacity-associated protein (Protein II): Assists in sticking and invading host cells.
- Transferrin-binding and lactoferrin binding protein: Necessary for absorbing iron.
- IgA1 protease: Breaks down mucosal IgA antibodies.
- Lipooligosaccharide (LOS): Different from the LPS of Enterobacteriaceae as it lacks the repeating O side chain.
Typing of Gonococci
- Serotyping: Based on protein-I (porin).
- Auxotyping: Classification based on the nutritional needs of the strains, for example, the AHU auxotype requires arginine, hypoxanthine, and uracil for growth.
Clinical Manifestations
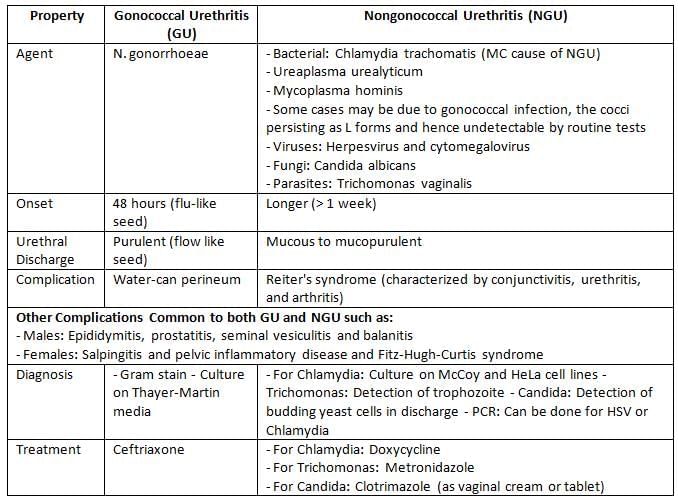
Gonorrhea is a sexually transmitted infection known since ancient times.
- In males:
- Acute urethritis: The most common symptom, characterized by pus in the urethra (the term "gonorrhea" means flow of seed, similar to semen).
- Incubation period: Usually lasts 2 to 7 days.
- Complications: May include epididymitis, prostatitis, swelling of the penis, and balanitis.
- Infection spread: Can move to nearby tissues, causing abscesses and sinus formations (termed water-can perineum).
- In females: Gonococcal infections tend to be milder, often leading to asymptomatic cases:
- Mucopurulent cervicitis: The most common symptom.
- Vulvovaginitis: Seen in prepubescent girls and postmenopausal women, but not typically in adult women due to resistance from low pH and thick epithelial tissue.
- Salpingitis and pelvic inflammatory disease: Can result in infertility.
- Fitz-Hugh-Curtis syndrome: A rare condition marked by peritonitis and associated liver inflammation.
- In both sexes:
- Anorectal gonorrhea: Presents as acute proctitis, often with drug-resistant rectal isolates.
- Pharyngeal gonorrhea: Spread through oral sex.
- Ocular gonorrhea: Infection in the eyes.
- In neonates: Ophthalmia neonatorum:
- Symptoms: Characterized by pus in the eyes, appearing 2 to 5 days after birth.
- Transmission: Occurs during birth from the mother’s genital bacteria.
- Treatment: Application of silver nitrate solution in the newborn's eyes (Crede’s method).
- Disseminated gonococcal infection (DGI): Occurs in 0.5 to 3% of untreated individuals:
- DGI symptoms: Features polyarthritis and, in rare cases, skin rashes and heart infections.
- Common associations: Most linked to PorB.1A serotypes and AHU auxotypes.
- Risk factors: Menstruation and deficiencies in complement proteins (C5–C9) increase the risk.
- In HIV-infected individuals: Gonorrhea increases the risk of spreading HIV.
Laboratory Diagnosis
Sample Collection:
- Males: Urethral discharge is collected for testing.
- Females: Endocervical swabs are preferred, as high vaginal swabs are not recommended.
- For Disseminated Gonococcal Infection (DGI): Blood and synovial fluid cultures are performed.
Transport Media
- Charcoal impregnated swabs/medium (Stuart/Amies media)
- For longer holding periods: CO2 generating system (JEMBEC system)
Gram staining
- For males: Gram staining of urethral discharge is more sensitive (90%); treatment can be started based on this.
- For females: Gram staining is less sensitive (50–60%) due to the presence of commensal Neisseria spp. in the genital tract, so endocervical culture is recommended.
- Endocervical culture: Gonococci are more difficult to grow than meningococci.
- Culture media for acute gonorrhoea: Chocolate agar and Mueller-Hinton agar.
- Selective media are useful in chronic cases:
- Thayer-Martin media
- Modified New York City medium
- Martin-Lewis Media
Treatment
- The DOC is a single-dose regimen of Ceftriaxone and Cefotaxime.
- Treat both partners; the regimen should also include azithromycin for Chlamydia.
- Many strains show resistance to penicillin due to penicillinase production. These are called PPNG strains (Penicillinase producing strains of N. gonorrhoeae).
The document Neisseria and Moraxella Chapter Notes | Microbiology - NEET PG is a part of the NEET PG Course Microbiology.
All you need of NEET PG at this link: NEET PG
|
75 docs|5 tests
|
FAQs on Neisseria and Moraxella Chapter Notes - Microbiology - NEET PG
| 1. What are the main virulence factors associated with Neisseria and Moraxella species? |  |
Ans. Neisseria species, particularly Neisseria meningitidis, possess several virulence factors, including a polysaccharide capsule that helps evade phagocytosis, pili for adherence to host tissues, and the ability to produce endotoxin (lipooligosaccharide). Moraxella catarrhalis has virulence factors such as outer membrane proteins that facilitate adherence, a beta-lactamase enzyme that provides resistance to certain antibiotics, and the ability to form biofilms, enhancing its survival in the host.
| 2. What is the epidemiology of Neisseria and Moraxella infections? |  |
Ans. Neisseria meningitidis primarily causes meningococcal disease, which is more common in children and adolescents, particularly in crowded environments like dormitories and military barracks. Moraxella catarrhalis is often associated with respiratory infections, particularly in children and individuals with chronic obstructive pulmonary disease (COPD). Both pathogens can be transmitted through respiratory droplets, and outbreaks of Neisseria meningitidis are more prevalent in certain geographical regions, especially in the "meningitis belt" of sub-Saharan Africa.
| 3. How do Neisseria and Moraxella cause disease in humans? |  |
Ans. Neisseria meningitidis invades the mucosal surfaces of the nasopharynx, leading to bacteremia and potentially meningitis, where the bacteria cross the blood-brain barrier. Moraxella catarrhalis typically causes localized infections such as otitis media and sinusitis, particularly in children, by colonizing the upper respiratory tract and causing inflammation and tissue damage.
| 4. What laboratory methods are used to diagnose infections caused by Neisseria and Moraxella? |  |
Ans. Diagnosis of Neisseria meningitidis often involves culture of cerebrospinal fluid (CSF) or blood, where Gram staining can reveal Gram-negative diplococci. Polymerase chain reaction (PCR) can also be used for rapid detection. For Moraxella catarrhalis, cultures from respiratory secretions can be performed, and Gram staining may show Gram-negative diplococci. Serotyping can aid in identification and differentiation of Neisseria species.
| 5. What treatment options are available for infections caused by Neisseria and Moraxella? |  |
Ans. Neisseria meningitidis infections are typically treated with intravenous antibiotics such as penicillin or ceftriaxone. Prophylactic antibiotics are recommended for close contacts of infected individuals. Moraxella catarrhalis is often treated with antibiotics such as amoxicillin-clavulanate or cephalosporins, as it commonly exhibits resistance to penicillin. Vaccination is also available for Neisseria meningitidis to prevent meningococcal disease.
Related Searches















