NEET PG Exam > NEET PG Notes > Microbiology > Chapter Notes: Nematodes
Nematodes Chapter Notes | Microbiology - NEET PG PDF Download
| Table of contents |

|
| General Characteristics of Nematodes |

|
| Intestinal Nematodes |

|
| Filarial Nematodes |

|
| Trichinella Spiralis |

|
| Dracunculus Medinensis |

|
| Larva Migrans |

|
| Miscellaneous Topics |

|
General Characteristics of Nematodes
- They are unsegmented, elongated, and cylindrical in shape
- They have separate sexes
- They possess a buccal capsuleaza
- Their gastrointestinal tract is complete
- They have a body cavity
- Regarding size:
- Small ones include Trichinella, Strongyloides, Hookworm, Trichuris
- Large ones include Dracunculus, Ascaris
- Their body is covered with a tough cuticle
Intestinal Nematodes
Classification According to Nematodes Habitat
- Intestinal human nematodes:
- Small Intestine: Ascaris lumbricoides, Hookworm (Ancylostoma and Necator), Strongyloides
- Large intestine: Trichuris and Enterobius
- Somatic human nematodes: Filarial worm, Trichinella spiralis, Dracunculus medinensis (Guinea worm)
Classification According to Whether they Produce Egg/Larva
- Viviparous: Lay Larva- Filarial worm, Trichinella and Dracunculus
- Oviparous: Lay eggs which hatch out to larva later in the environment- Ascaris, Hookworm, Trichuris and Enterobius
- Ovoviviparous: Lay eggs containing larva which immediately hatchout, e.g. Strongyloides
Necator vs Ancylostoma
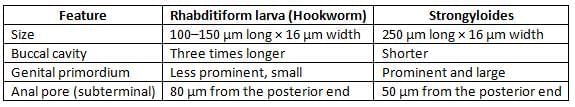
- Egg and Rhabditiform larva—same
- They differ only in filariform larva and in adult worm
- Filariform larva of Necator:
- Gap between oesophagus and intestine
- Cuticle: Bears prominent transverse striation
- Buccal capsule: Larger (15 µm), lumen short

- Stool Culture is required for Hookworm and Strongyloides: To demonstrate rhabditiform larva which on further cultivation, transform to filariform larva
- Harada Mori technique
- Baermann funnel technique
- Charcoal culture method
- Agar Plate technique (more sensitive)
- Chandler’s index is done for hookworm: eggs per gram of stool:
- Below 200: Hookworm is not of much significance
- 200–250: May be regarded as potential danger
- 250–300: Minor public health problem
- Above 300: Important public health problem
- N. americanus is predominant hookworm in India (and world) and except in Punjab and UP (Ancylostoma is more common)
- Wakana disease:
- Seen only in Ancylostoma but not in Necator
- Occurs: When L3 larva is transmitted by oral route (Not by skin penetration)
- Both GIT and pulmonary symptoms seen
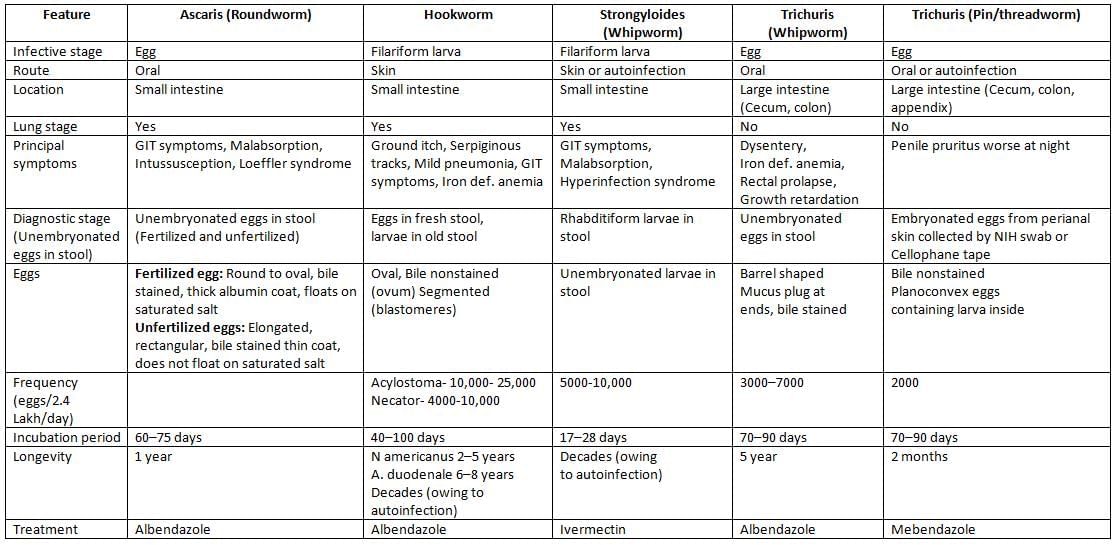
 Life cycle of trichuris/enterobius/ascaris
Life cycle of trichuris/enterobius/ascaris
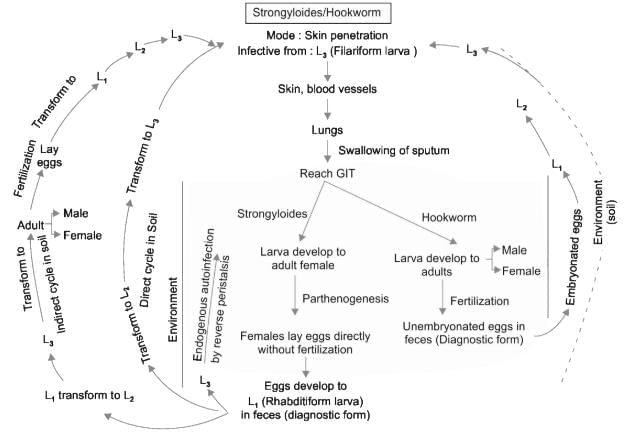 Life cycle of strongyloides/hookworm
Life cycle of strongyloides/hookworm
- Hyperinfection syndrome
- Repeated autoinfection cycles lead to heavy filariform larvae load
- Seen in HTLV1 infected people (rarely HIV)
- Most important risk factor: Glucocorticoid therapy
- Serum IgE level becomes low
- Larvae may invade the GIT and migrate to various organs including CNS, peritoneum, liver, and kidneys
- Moreover, the passage of enteric flora through disrupted mucosa lead to Gram-negative sepsis
- CNS invasion: Brain abscess and meningitis are common. Larvae can be seen in CSF
- Sometimes, if the stool sample is examined late, the eggs of hookworm may transform to rhabditiform larva which have to be differentiated from that of Strongyloides
Treatment
Albendazole is the DOC of all nematodes except- Enterobius: Mebendazole
- Strongyloides: Ivermectin
- Wuchereria and Brugia: DEC
- Onchocerca: Ivermectin
- Dracunculus: Metronidazole
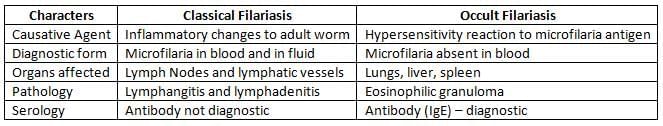
Filarial Nematodes
Pathogenesis and Life Cycle
- Infective form: Filarial larvae (L3) transmitted by Mosquito bite
- L3 larva migrate through lymphatics to local LN where they transform to adult worm then to L1(microfilaria)

- Microfilaria are not pathogenic, but are periodically discharged to blood (diagnostic form)
- Adult female worm: Crucial role in pathogenesis
- Triad of pathogenesis:
- Dilatation of lymphatic vessel
- Lymphadenitis
- Obstruction to lymphnode: Fibrotic degeneration of lymph vessel
Lymphatic Filariasis
- Endemic Normal:
- Asymptomatic, no microfilaria in blood
- Occurs due to insufficient exposure, immunological resistance, prepatent period at time of detection
- Asymptomatic Stage:
- Microfilaria present in blood, but no clinical feature
- Th1 is down regulated but Th2 is high (IL4↑)
- After several years, hyporesponsiveness breaks and inflammatory reaction occurs
- Acute Filariasis:
- Due to antigens released from female adult worm
- Filarial fever: High grade fever
- Lymphatic inflammation (lymphangitis and lymphadenitis)
- Transient local edema
- Dermatolymphangitis
- Chronic Filariasis:
- 10–15 years after acute phase
- Fibrotic changes occurs (obstructive phase) in lymph vessels
- Featured by:
- Lymph varices
- Hydrocele
- Elephantiasis of scrotum, leg, arms, breast and vulva (nonpitting edema)
- Granuloma of female breast
- Chyluria chyle in urine (d/t obstruction of lymph vessels of kidney and abdomen)
Brugia Malayi
- Transmission:
- Nocturnal strains: Transmitted from Man-Man by bite of Mansonia
- Subperiodic strains: Transmitted from monkey (Zoonotic): by Mansonia
- Anopheles and Aedes rarely transmit
- Pistia stratiotes plant: Important for survival for Mansonia
- Clinical feature:
- Leg below knee: ONLY affected (Contour of knee- normal)
- Genital and chyluria NOT marked
- MC-acute adenolymphangitis and filarial abscesses
- Diagnosis: Microfilaria is differentiated from that of W. bancrofti by pointed tail tip, Nuclei column darkly stained, large, coarse, overlapping, extended till the tail tip
- B. timori: Timor island of Indonesia, Vector-Anopheles barbirostris
Lab Diagnosis
- Blood microscopy:
- Blood is collected during:
- Nocturnal: 10 pm to 4 am
- Subperiodic nocturnal: 8 pm to 10 pm
- Subperiodic diurnal: 2 pm to 6 pm
- DEC provocation test: Done to demonstrate microfilaria in day time
- Direct wet mount: To see serpentine movement of microfilaria
- Staining: Thick blood smear stained with Leishman/Giemsa
- Concentration methods: Membrane filtration technique and Knott’s centrifugation technique
- QBC: Quantitative Buffy Coat
- Microfilaria NOT found in peripheral blood:
- Occult filariasis
- Chronic filariasis (some cases)
- Wrong time
- Other samples:
- Urine microscopy: 10–20 ml early morning chylous urine
- Hydrocele fluid and LN aspirate microscopy
- Blood is collected during:
- Demonstration of antibody:
- Methods… IHA , IFA, ELISA, RIA
- Disadvantage:
- Cross reactivity
- Unable to discriminate between recent and past infection
- Demonstration of antigen:
- Indicates recent infection
- More sensitive than microscopy
- Can be detected in daytime
- Can differentiate current and past infection: Antigen disappears after clinical cure
- Can detect in urine antigen
- ELISA: Using monoclonal antibody against AD12 antigen detects adult worm only
- ELISA: Using monoclonal antibody against Og4C3 antigen detects adult worm and microfilaria
- No antigen detection methods are available for Brugia infection
- Molecular methods: PCR detecting as low as 1pg of filarial DNA
- Imaging methods:
- X Ray: Dead and calcified worm in LN and chest X ray shows pulmonary infiltrate in TPE
- Ultrasound of scrotum: Live adult worms with serpentine movement (Filarial Dance sign)
Treatment
- Diethyl Carbamazine (DEC): DOC
- DEC + Albendazole regimen: In India
- DEC + Ivermectin regimen: In Africa
- DEC acts on both microfilaria and adult where as ivermectin acts only on microfilaria
Onchocerca Volvulus
- West Africa
- Skin manifestations:
- Dermatitis (Sowda )
- Leopard skin
- Onchocercoma (subcutaneous nodules)
- Ocular involvement:
- River blindness
- Punctate keratitis
- Sclerosing keratitis
- Lymph Nodes: Hanging groin
- Detection of the microfilariae: Skin snips technique
- Mazzotti skin test (DEC patch test)
- Ivermectin: DOC
Trichinella Spiralis
- Host-Pig: Optimum host and reservoir, man is an accidental host and acts as dead end
- Infective stage: First stage (L1) larva
- Mode of transmission: By ingestion of raw or uncooked pork
- Larva penetrate intestine and migrate to muscle where it undergoes encystment
- MC muscle: Extraocular muscles followed by the biceps; and the muscles of the jaw, neck
- Diagnosis: Demonstration of larvae in muscle biopsy taken near tendon insertions of deltoid
- Antibody detection: Confirms the diagnosis but cannot differentiate past and present infection
- Bachman intradermal test: Persists for life, hence cannot differentiate past and present infection
Dracunculus Medinensis
- Causes Guinea worm disease or dracunculiasis
- It is eliminated from India since 2000 (and also from Pakistan), incidence is reduced in Asia
- Last case was reported from July 1996
- Currently: Limited to few countries in sub-Saharan Africa
- Host: Man is the definitive host and Copepods (Cyclops) are the intermediate host
- Infective form: Third stage filariform larvae
- Mode of transmission: Drinking fresh water from stagnant pools containing minute fresh water crustaceans (Cyclops) infected with L3 larvae
- Presentation: Starts as painful papule , becomes blister from which the worm emerges
- Seasonal (June–September); Disease is a strong indicator of poor socioeconomic development
- Microscopic detection of L1 larvae and adults: On contact with cold water placed on the leg ulcer
- Treatment: Worm removal and symptomatic treatment
- Reasons for Eradication of Guinea worm disease from India:
- d/t National Guinea worm eradication programme (1984)
- Provision of safe drinking water: Filtration of drinking, installing hand pumps and pipes
- Cyclops control: By application of Abate larvicide
- Provision of clean drinking water from boreholes or wells
- Health education of people in matter related to boiling or filtering of drinking water
- Treatment of cases
Larva Migrans
- The life cycle of most of the human nematodes involves penetration of the skin by the larval stage followed by migration of the larvae to intestine, lungs or other organs
- However, the larvae of lower animal nematodes when accidentally infect man, they are not able to complete their normal development (because humans are the unusual host for them) and their life cycle gets arrested. The larvae wander around aimless way in the body. This is called as larva migrans
- Two types of larva migrans exists:
- Cutaneous larva migrans: Also called as creeping eruption. Larva migration occurs in skin and subcutaneous tissue
- Visceral larva migrans: Larva migration takes place in viscera

Miscellaneous Topics
- Capillaria philippinensis: Eggs resemble like Trichuris
- Trichostrongylus spp. (Pseudo hookworm): Eggs resemble to that of hookworm. Rhabditiformslarva’s tail end has a bead-like swelling
- Non bile stained eggs (NEHA)
- Necator americanus
- Enterobius vermicularis
- Hymenolepis nana
- Ancylostoma
- Autoinfection is seen in
- Cryptosporidium
- Hymenlepis nana
- Taenia solium
- Strongyloides
- Enterobius
- Does not float in saturated salt solution (ULTO)
- Unfertilized egg of Ascaris
- Larva of Strongyloides
- Taenia egg
- Operculated egg of trematodes
The document Nematodes Chapter Notes | Microbiology - NEET PG is a part of the NEET PG Course Microbiology.
All you need of NEET PG at this link: NEET PG
|
75 docs|5 tests
|
FAQs on Nematodes Chapter Notes - Microbiology - NEET PG
| 1. What are the main classifications of nematodes based on their habitat? |  |
Ans. Nematodes can be classified according to their habitat into two primary categories: free-living and parasitic nematodes. Free-living nematodes typically inhabit soil, freshwater, and marine environments, playing important roles in nutrient cycling and soil health. In contrast, parasitic nematodes live in or on a host organism, often causing disease. This group can be further divided into those that inhabit the intestines, tissues, or blood of their hosts.
| 2. How do Necator and Ancylostoma differ in terms of their life cycle and pathogenesis? |  |
Ans. Necator americanus and Ancylostoma duodenale are both hookworms but differ in their life cycles and pathogenic effects. Necator americanus primarily infects humans through skin penetration and can cause iron-deficiency anemia due to blood loss. Its larvae develop in the soil before infecting a host. Ancylostoma duodenale can also penetrate the skin but has an additional transmission route through ingestion of larvae. It is capable of causing more severe anemia and has a higher potential for reinfection due to its ability to survive longer in the environment.
| 3. What is lymphatic filariasis, and what is the role of Brugia malayi in this condition? |  |
Ans. Lymphatic filariasis is a tropical disease caused by parasitic infections that affect the lymphatic system, leading to severe swelling and disability. Brugia malayi is one of the filarial species responsible for this condition. It is transmitted through the bite of infected mosquitoes and can cause lymphedema and hydrocele. The adult worms reside in the lymphatic vessels, leading to chronic inflammation and damage if not treated.
| 4. What methods are commonly used for the laboratory diagnosis of nematode infections? |  |
Ans. Laboratory diagnosis of nematode infections typically involves stool examination for eggs or larvae, blood tests for filarial antigens, and serological tests. In cases of tissue-dwelling nematodes, tissue biopsies may be analyzed. Microscopic identification of specific eggs or larvae is crucial for accurate diagnosis and often requires skilled technicians to distinguish between species.
| 5. What are the standard treatments for infections caused by nematodes? |  |
Ans. The treatment for nematode infections generally involves the use of anthelmintic medications. Commonly prescribed drugs include albendazole and mebendazole for intestinal nematodes, which work by disrupting the worm's metabolism. For lymphatic filariasis caused by Brugia malayi, diethylcarbamazine (DEC) is often used to eliminate the adult worms. It's important to note that treatment regimens may vary based on the specific nematode and the severity of the infection.
Related Searches



















