Spirochetes Chapter Notes | Microbiology - NEET PG PDF Download
| Table of contents |

|
| Introduction |

|
| Syphilis |

|
| Nonvenereal Treponematoses |

|
| Borrelia |

|
| Leptospira |

|
Introduction
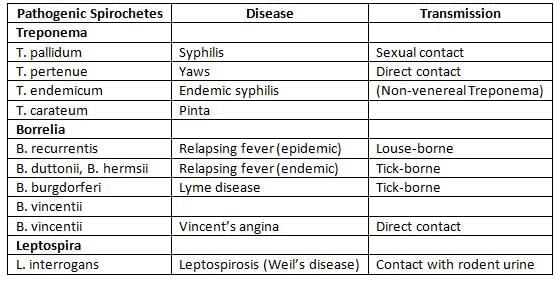
Spirochetes are long, thin bacteria that are flexible and have a spiral shape. The word "spirochete" comes from the Greek words "speira," meaning coil, and "chaite," meaning hair. Some types of these bacteria can cause diseases in people. Notable genera of spirochetes include Treponema, Borrelia, and Leptospira.
Syphilis
Syphilis is one of the oldest known sexually transmitted diseases. The name "syphilis" comes from a famous poem written in 1530 about a shepherd named Syphilus who suffered from this illness.
How Syphilis is Spread
- Sexual Contact: Syphilis is primarily spread through sexual contact.
- Non-Sexual Transmission: Syphilis can also be transmitted through non-sexual means, including:
- Direct contact with an infected person
- Blood transfusion
- Transmission from mother to child during pregnancy
The time it takes for symptoms to appear after infection, known as the incubation period, can vary from 9 to 90 days. The incubation period is shorter when a larger number of organisms are introduced into the body.
Clinical Manifestations of Syphilis
Syphilis is a sexually transmitted infection that progresses through different stages, including primary, secondary, latent, and tertiary (or late) stages. Approximately 30% of individuals who have sexual contact with an infected partner may develop syphilis.
Primary Syphilis
- Primary (or hard) chancre: A single painless ulcer that is firm and raised. The most common locations for this ulcer are the penis in males and the cervix or labia in females.
- Regional lymphadenopathy: This usually affects the inguinal (groin) area. The lymph nodes are painless, firm, do not produce pus, and are often found on both sides.
- If syphilis is acquired through non-venereal means:
- If transmitted by direct contact, the primary chancre may appear in an extragenital location, often on the fingers.
- If transmitted through blood transfusion, a primary chancre does not occur.
Secondary Syphilis
- Secondary syphilis is the stage that follows the primary infection of syphilis, characterized by the healing of the initial lesion.
- This stage typically develops 4 to 8 weeks after the primary lesion has healed.
- Key Features of Secondary Syphilis:
- Skin Rashes: One of the hallmark signs of secondary syphilis is the presence of skin rashes. These rashes are often found on the palms of the hands and the soles of the feet.
- Condylomata Lata: Condylomata lata are mucocutaneous lesions that occur during secondary syphilis. These lesions are a result of the infection spreading and are characterized by their appearance on mucous membranes and skin.
- Mucous Patches: In secondary syphilis, mucous patches may develop, which are superficial erosions of the mucosal tissue. These patches are a sign of the ongoing infection and can occur in various mucosal areas.
- Generalized Lymphadenopathy: Another significant feature of secondary syphilis is generalized lymphadenopathy, which refers to the swelling of lymph nodes throughout the body. This occurs as the body’s immune response is activated to combat the infection.
Latent Syphilis
- It is marked by the lack of visible symptoms of syphilis while having positive blood tests for the disease and normal findings in cerebrospinal fluid (CSF) in individuals with a history of primary and secondary syphilis in the past.
- There are two types of latent syphilis:
- Early latent syphilis occurs within the first year after the infection.
- Late latent syphilis happens after the first year.
- Individuals with latent syphilis can still spread the infection through the bloodstream or to an unborn child (in utero).
- Latent syphilis can lead to one of these outcomes:
- Persistent lifelong infection (this is common).
- Development of late syphilis (this is rare).
- Spontaneous cure where blood tests become negative (this is also rare).
Late or Tertiary Syphilis
- One-third of patients who do not receive treatment may develop tertiary syphilis after several decades.
- Gumma (late benign syphilis): This occurs in 15% of people.
- Cardiovascular syphilis (affecting 10%of people): This is marked by
- Aneurysm of the ascending aorta.
- Aortic regurgitation.
- Neurosyphilis (also in 10% of people): This involves the CNS (central nervous system) in the first few weeks of infection, but symptoms appear only in the late stage. CNS and CVS (cardiovascular system) issues are referred to as quaternary syphilis:
- General paresis of the insane.
- Tabes dorsalis: This is the demyelination of the posterior columns of the spinal cord.
- Meningeal syphilis: This causes meningitis.
- Meningovascular syphilis: This is inflammation of the arteries that can lead to an embolic stroke.
Congenital Syphilis
- Placental transmission can happen at any point during pregnancy, but fetal harm typically occurs only after the fourth month of gestation. Symptoms of congenital syphilis include:
- The first signs appear within 2 years of age. Affected children can spread the infection and may experience:
- Rhinitis (also known as snuffles).
- Skin and mucous membrane lesions.
- Changes in bones.
- Hepatosplenomegaly (enlargement of the liver and spleen).
- Lymphadenopathy (swollen lymph nodes).
- Late congenital syphilis occurs after the age of 2 years and is not infectious. It is marked by:
- Interstitial keratitis (inflammation of the eye).
- Bilateral deafness (eighth-nerve deafness).
- Knee swelling (Clutton’s joints).
- Residual stigmatization may persist for a long time, including:
- Hutchinson’s teeth: Notched central incisors.
- Mulberry molar.
- Saddle nose and saber shins.
Laboratory Diagnosis of Syphilis
1. Microscopy:
- Dark Ground Microscopy:
- Treponema pallidum appears as slender, flexible, spirally coiled bacilli with tapering ends, exhibiting three types of movement:
- Flexion-extension
- Corkscrew motion
- Rotational bending in the middle
- Sensitivity is 80%, with a detection limit of 104 bacilli/ml.
- Treponema pallidum appears as slender, flexible, spirally coiled bacilli with tapering ends, exhibiting three types of movement:
- Direct Fluorescent Antibody Staining for T. pallidum (DFA-TP): This method has a sensitivity of 100%.
- Silver Impregnation Method:
- Levaditi stain for tissue sections
- Fontana stain for smears
2. Culture:
- Pathogenic treponemes cannot be grown in artificial culture media.
- They can only be maintained in rabbit testes.
- In contrast, nonpathogenic treponemes, such as Reiter treponemes, can be cultured.
- These nonpathogenic treponemes grow well in Smith-Noguchi media.
3. Serology (Antibody Detection)
- Nontreponemal or Nonspecific Tests: These tests detect reagin antibodies using a nonspecific cardiolipin antigen from bovine heart.
- Wassermann test
- CFT (Complement Fixation Test)
- Kahn Test
- Tube Flocculation
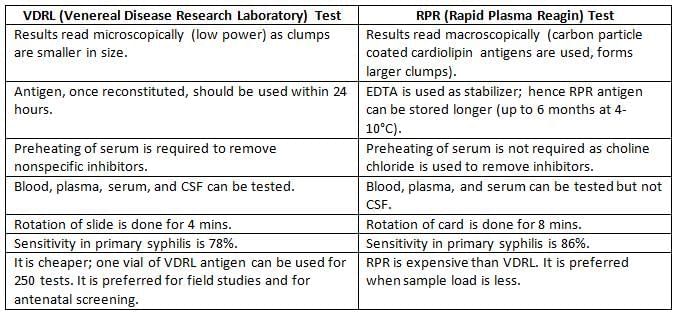
- VDRL (Venereal Disease Research Laboratory) Test
- Slide Flocculation
- RPR (Rapid Plasma Reagin)
- USR (Unheated Serum Reagin Test)
- TRUST (Toluidine Red Unheated Serum Test)
- Specific/Treponemal Tests: These tests detect specific antibodies using T. pallidum antigens.
- TPI (Treponema Pallidum Immobilization Test) uses live T. pallidum.
- FTA-ABS (Fluorescent Treponemal Antibody Absorption Test) uses killed T. pallidum.
- TPA (Treponema Pallidum Agglutination Test)
- TPIA (Treponema Pallidum Immune Adherence Test)
- TPHA (Treponema Pallidum Hemagglutination Test) uses an antigenic extract of T. pallidum.
- TPPA (Treponema Pallidum Particle Agglutination Test)
- Western Blot
- Enzyme Immunoassay (EIA)
- Group Specific: RP CFT (Reiter Protein Complement Fixation Test) uses the Reiter strain.
4. Polymerase Chain Reaction (PCR)
VDRL (Venereal Disease Research Laboratory)
The VDRL test is a type of slide flocculation test, which involves a precipitation reaction to detect certain antibodies.
- Antigen Preparation: The antigen used in the VDRL test is prepared from cardiolipin extracted from bovine heart tissue, to which cholesterol and lecithin are added. This antigen needs to be reconstituted with a buffer and should be used within 24 hours of preparation.
- Patient’s Serum Preparation: To prepare the serum from the patient's sample, it is heated at 56°C for 30 minutes. This step is crucial to eliminate non-specific inhibitors that could interfere with the test results.
- VDRL Slides: The slides used for the VDRL test contain 12 concave rings, which are essential for conducting the test.
- Qualitative Test Procedure: drop of the inactivated serum is mixed with a drop of the VDRL antigen on the slide, which is then rotated for 4 minutes.
- Non-reactive Result: If the test is non-reactive, uniform fusiform crystals will be observed, indicating the presence of VDRL antigen only.
- Reactive Result: reactive result is indicated by medium to large clumps, suggesting the formation of antigen-antibody complexes.
- VDRL in CSF: The VDRL test can also be performed on cerebrospinal fluid (CSF) to detect antibodies, and in this case, preheating of the serum is not necessary.
Advantages of Non-Treponemal Tests:
Non-treponemal tests, such as VDRL, have several advantages, including:
- Monitoring the response to treatment: Reagin tests typically turn negative within 6 to 18 months after effective treatment for syphilis, depending on the stage at which the treatment is administered.
- For neurosyphilis, the VDRL test can be used to find CSF antibodies.
- The reagin antibody becomes detectable 7 to 10 days after the primary chancre appears (or 3 to 5 weeks after infection).
- The sensitivity of non-treponemal tests varies as follows:
- Primary stage: 78% to 85%
- Secondary stage: 100%
- Latent stage: 95% to 98%
Disadvantages of Nontreponemal Tests
- Biological false positive (BFP) reactions are defined as positive results from nontreponemal tests, accompanied by negative results from treponemal tests, without any technical errors or clinical symptoms. This situation happens in about 1% of cases.
- The BFP antibody is usually of the IgM type, while the antibody for syphilis, known as reagin, is mainly IgG.
- Types of BFP: BFP reactions can be categorized based on their duration:
- Acute BFP reactions last less than 6 months. Examples include:
- Acute infections
- Injuries
- Inflammatory conditions
- Chronic BFP reactions last longer than 6 months. Examples include:
- SLE (Systemic Lupus Erythematosus)
- Other collagen diseases such as rheumatoid arthritis
- Other conditions that may cause BFP include:
- Lepromatous leprosy
- Relapsing fever
- Malaria
- Tropical pulmonary eosinophilia
- Viral hepatitis
- Infectious mononucleosis
- HIV
- Pregnancy
- IV drug use
- Acute BFP reactions last less than 6 months. Examples include:
- The Prozone phenomenon can lead to a false negative result if the antibody titer in the patient’s serum is very high.
- The sensitivity of nontreponemal tests is lower in the late stages of syphilis.
- Screening tests: Nontreponemal tests are used as initial screening tools, but results should be confirmed with treponemal tests.
- If treponemal tests are positive, it confirms the presence of syphilis.
- If treponemal tests are negative, it indicates that the nontreponemal tests were false positives.
One-Liners for Serological Tests in Syphilis
- Monitoring Treatment: The Ideal test is VDRL > RPR
- Primary Syphilis: Most Sensitive: Western blot and EIA > TPPA > RPR > FTA-ABS
- Secondary Syphilis: All tests are equally sensitive (100%)
- Latent Syphilis: Most Sensitive: All treponemal tests
- Late Syphilis: Most Sensitive: FTA-ABS > TPHA
- Overall Most Specific: TPHA, EIA, USR, TRUST (All 99%) > TPPA
- First Test to be Positive: FTA-ABS
- Rapid and Mass Screening: VDRL
Diagnosis of Congenital Syphilis
Definitive diagnosis: This is confirmed by showing T.pallidum through direct examination of:
- umbilical cord
- placenta
- nasal discharge
- skin lesions
Presumptive diagnosis: This can be suggested if:
- An infant is born to a mother who had syphilis during delivery, no matter the infant's condition.
- The infant has a positive result on a treponemal test.
- One of the following additional criteria is met:
- There are clinical signs or symptoms of congenital syphilis.
- There are abnormal findings in the cerebrospinal fluid (CSF) with no other explanation.
- The VDRL test of the CSF comes back positive.
- The infant has a positive IgM antibody test specifically for syphilis (either IgM FTA ABS or IgM ELISA).
- Note: Since IgM cannot cross the placenta, its presence in the baby's blood confirms congenital syphilis.
Screening for Congenital Syphilis Based on VDRL Test (IgG)
Serial IgG in Baby (VDRL):
- If maternal transfer occurs, the titer will decrease within 3 months.
- If congenital infection is present, the titer will increase within 3 months.
Simultaneous VDRL Test of Mother and Baby:
- If the mother’s titer is greater than the baby’s titer, it indicates maternal transfer.
- If the baby’s titer is greater than the mother’s titer, it indicates congenital infection.
- Sample Collection: Baby serum is the most appropriate sample, followed by cord blood and maternal serum.
Treatment for Syphilis
- Penicillin is the preferred treatment for all stages of syphilis:
- Primary, secondary, or early latent syphilis: a single dose of Penicillin G is sufficient.
- Late latent, cardiovascular, or benign tertiary syphilis: Penicillin G administered weekly for 3 weeks.
- Neurosyphilis or co-infection with HIV: Aqueous crystalline or procaine penicillin G for 10 to 14 days.
- Alternative Treatment for Penicillin-Allergic Patients:
- Primary, secondary, latent, cardiovascular, or benign tertiary syphilis: Tetracycline may be used.
- Neurosyphilis, pregnancy, or co-infection with HIV: Desensitization to penicillin is necessary, followed by penicillin treatment.
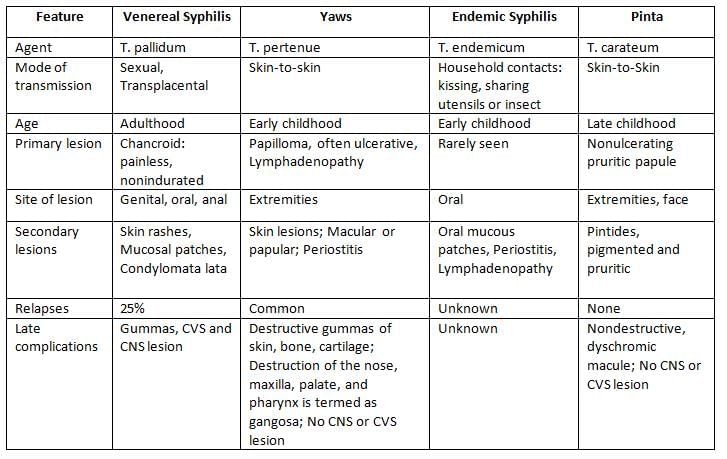
Nonvenereal Treponematoses
Endemic treponematoses can be distinguished from venereal syphilis by several factors:
- Mode of transmission: Endemic treponematoses are transmitted through direct contact, not through sexual means.
- Age of acquisition: These infections are usually acquired during childhood.
- Geographic distribution: Endemic treponematoses are found in rural areas of developing nations and among travelers in developed countries.
- Associated with: Poor hygiene is a common associated factor.
- Clinical features: The clinical features are described in the relevant text.
Borrelia
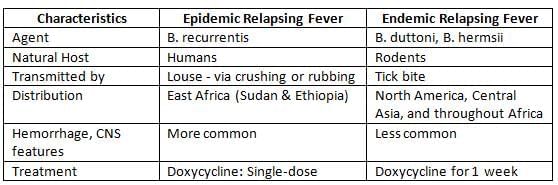
Relapsing Fever
- Relapsing fever gets its name because it involves alternating times of having a fever and not having a fever.
- The reason for these relapses is due to antigenic variation, which is a characteristic of the germ that causes this illness, known as B. recurrentis.
Borrelia is a genus of bacteria that can cause various diseases, primarily transmitted through vectors like lice and ticks.
- B. recurrentis is responsible for epidemic relapsing fever and is spread by lice.
- B. duttonii and B. hermsii cause endemic relapsing fever and are transmitted by ticks.
- B. burgdorferi is the causative agent of Lyme disease, which is also transmitted by ticks.
- B. vincentii is often mistakenly associated with Vincent’s angina, which is actually linked to Bacteroides and Fusobacterium species.
Laboratory Diagnosis
- Microscopic Examination of Blood:
- Wet film analysis using dark field or phase contrast microscopy.
- Staining methods like Giemsa and Leishman, or techniques like Quantitative Buffy Coat (QBC).
- Polymerase Chain Reaction (PCR): a more sensitive method that also allows for species identification.
- Serology (Antibody Detection):
- Enzyme-Linked Immunosorbent Assay (ELISA) and Indirect Immunofluorescence Assay (IFA) can occasionally produce false positives but are useful when combined with clinical assessment.
- GlpQ Assay: This is the most dependable serological technique, identifying antibodies against the GlpQ antigen (Glycerophosphodiester phosphodiesterase).
- Inoculation of Animals: Inoculating animals like mice may result in intraperitoneal infection.
- Molecular Methods: Multiplex Real-time PCR has been developed targeting the 16SrRNA and glpQ genes.
Lyme Disease
- Agent: B. burgdorferi
- Transmission: Tick-borne, specifically by Ixodes ricinus
- Clinical Manifestation: Characterized by a triad of stages:
- Stage 1: Erythema migrans, presenting as annular skin lesions.
- Stage 2: Disseminated infection involving skin lesions, meningitis, neuritis, nodal block, and joint pain. Neurological complications occur in 15% of cases, including meningitis, encephalitis, and a specific lymphocytic meningoradiculitis known as Bannwarth’s syndrome, prevalent in Europe and Asia.
- Stage 3: Persistent infection leading to arthritis, encephalopathy, or acrodermatitis.
- Lab Diagnosis:
- Diagnosis is primarily based on clinical symptoms.
- Isolation from skin lesions or blood using modified Kelley’s medium.
- Microscopic detection methods such as dark ground, phase contrast, immunofluorescence, and silver staining.
- Detection of antigens in urine can also aid in diagnosis.
- Antibody Detection:
- ELISA and western blot: During the first month, both IgM and IgG antibodies are present; later, IgM levels decrease.
- Limitations: Antibodies can persist for an extended period and may produce false positives in unrelated infections. A fourfold increase in antibody levels is more significant.
- Two-test approach: The CDC recommends performing ELISA first and confirming with western blot.
- C6 peptide IgG ELISA.
- Presence of polymorphonuclear cells (PMNs) in joint fluid but lymphocytosis in cerebrospinal fluid (CSF).
- Treatment:
- Drug of Choice (DOC) for all cases: Oral doxycycline is preferred over amoxicillin.
- DOC for Central Nervous System (CNS) or Atrioventricular (AV) block cases: Intravenous ceftriaxone is preferred over cefotaxime.
Borrelia Vincentii
- This bacterium is a commensal organism found in the mouth.
- Vincent’s angina is characterized by ulcerative gingivostomatitis, and predisposing factors include malnutrition and viral infections.
- Vincent’s angina is often associated with fusiform bacillus, now known as Leptotrichia, which was previously referred to as Fusobacterium fusiformis.
Leptospira
Classification
Species: Leptospira includes two species:
- L. interrogans (pathogenic for humans): Causes leptospirosis or Weil’s disease, affecting the liver and kidneys.
- L. biflexa (saprophyte)
Serovars and serogroups:
- L. interrogans contains 25 serogroups, which are made up of over 250 serovars.
- Although all serogroups and serovars look the same and cause similar symptoms, they vary in where they are found and how severe the illness can be.
Epidemiology
- Mode of transmission: The disease is zoonotic, meaning it can be passed from animals to humans. It does not spread directly between humans. It is transmitted by:
- Indirect contact with water, damp soil, and wet surfaces that have been contaminated by animal urine.
- Direct contact with the urine and products from birthing or the placenta of infected animals.
- Source: More than 100 animals can carry the bacteria, but the main sources of infection are:
- Rats
- Dogs
- Cattle
- Pigs
- Three key factors for leptospirosis outbreaks include exposure to rodents, rainfall, and rice fields.
- Global distribution: Leptospirosis is found worldwide, with the highest rates in Brazil, India, and Thailand.
- In India, the disease is common in Tamil Nadu, Kerala, and the Andaman Islands, where it may also be known as Andaman haemorrhagic fever.
- The Regional Medical Research Centre in Port Blair is the national reference centre for leptospirosis in India.
- Classic serovar: Animal associations include:
- Icterohemorrhagiae and Copenhageni in domestic rats ( Rattus norvegicus , R. rattus ): Most common serovar in India.
- Grippotyphosa in opossums and raccoons (growing concern in the USA)
- Canicola in dogs
- Hardjo in cattle and buffalo
- Pomona in pigs
Clinical Menifestations
The incubation period is about 5–14 days. The clinical signs can be grouped into two main types.
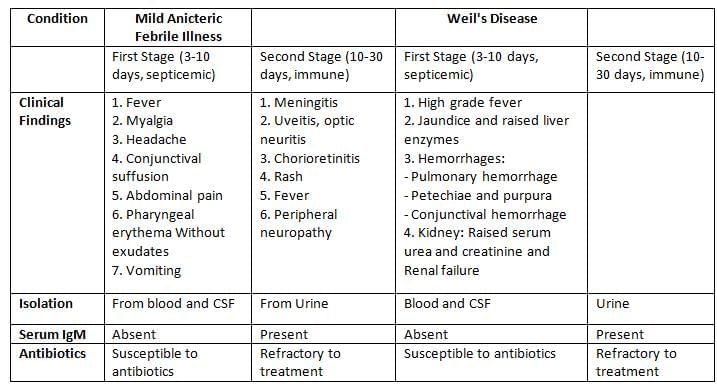
- Mild anicteric febrile illness: Seen in 90% of cases; it has two phases: septicemic followed by immune.
- Weil’s disease (Hepato-renal-hemorrhagic syndrome): A severe form of the illness, affecting 10% of patients. It may not show the typical biphasic pattern and is more serious.
Laboratory Diagnosis
- Specimens: CSF and blood (during the first 10 days of infection) and urine (between 10–30 days of infection).
- Microscopy: Leptospira are very thin and can be viewed under dark ground microscopy. They are tightly coiled with characteristic hooked ends, resembling an umbrella handle. They are highly mobile and show spinning and translational movements.
- Isolation:
- Culture condition: Leptospira needs oxygen to grow and grows slowly. Incubated at 30°C for 4–6 weeks.
- Culture media: Leptospira requires enriched media such as:
- EMJH medium (Ellinghausen, McCullough, Johnson, Harris) - the most common media.
- Korthof’s media with rabbit blood and Fletcher’s semisolid media.
- Advantages:
- Isolation confirms the diagnosis.
- Useful for maintaining the stock culture of Leptospira in labs.
- Disadvantages:
- The culture technique is laborious, technically demanding, and time-consuming.
- False positive results may occur due to contamination of culture media.
- False negative results may happen due to prior antibiotics or incorrect temperature and pH during incubation.
- Animal Inoculation: Hamsters (4–6 weeks old) and young guinea pigs.
- Serology for antibody detection:Tests for finding antibodies can be divided into two main types:
- Genus specific tests:These tests use a general antigen that is made from the nonharmful L. biflexa Patoc 1 strain. However, they cannot identify the specific serovar that is causing the infection.
- Macroscopic slide agglutination test
- Microcapsule agglutination test (MCAT)
- Latex agglutination test
- ELISA
- ICT
- Serovar specific test: The Microscopic agglutination test (MAT) is used to find antibodies against specific serovars of L. interrogans. It is considered the gold standard and reference test for diagnosing leptospirosis.
- Genus specific tests:These tests use a general antigen that is made from the nonharmful L. biflexa Patoc 1 strain. However, they cannot identify the specific serovar that is causing the infection.
- Molecular methods:
- Different genes, like 16S or 23S rRNA or the IS1533 insertion sequence, are targeted.
- PCR: This method can detect the infection early, even before antibodies are formed. However, it does not identify the specific serovar.
- PCR-RFLP or PFGE are techniques used to identify the genomospecies of Leptospira.
- Faine’s criteria: This is a guideline approved by WHO for diagnosing leptospirosis, based on clinical, epidemiological, and laboratory information.
- Nonspecific findings: These can include changes in kidney function and liver function test results.
Treatment
- For mild leptospirosis, the recommended treatment is to take doxycycline by mouth. An alternative option is amoxicillin.
- In cases of severe leptospirosis, the preferred medication is penicillin. Other possible treatments include ceftriaxone or cefotaxime.
|
75 docs|5 tests
|
FAQs on Spirochetes Chapter Notes - Microbiology - NEET PG
| 1. What are the clinical manifestations of syphilis? |  |
| 2. How is syphilis diagnosed in the laboratory? |  |
| 3. What is the treatment protocol for syphilis? |  |
| 4. What is relapsing fever and how is it related to spirochetes? |  |
| 5. What are the key epidemiological factors associated with Lyme disease? |  |



















