Staphylococcus Chapter Notes | Microbiology - NEET PG PDF Download
Staphylococcus aureus
Staphylococcus aureus is a type of bacteria that is:- catalase positive
- coagulase positive
- facultative anaerobe
- non-motile
- non-sporing
- occasionally capsulated
In Greek, Staphyle means bunch of grapes.
Staphylococcus was identified by Sir Alexander Ogston, and S. aureus was named by Rosenbach.
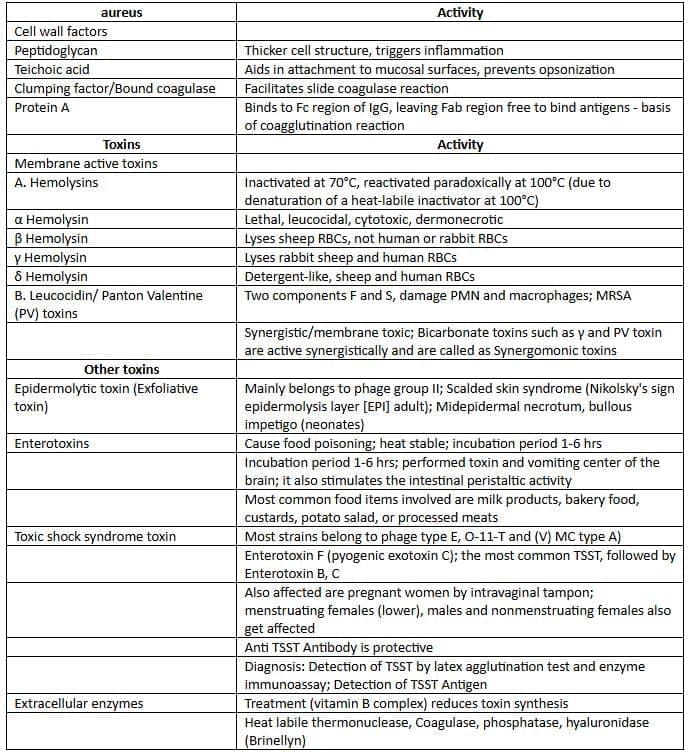
Virulence Factors of S. aureus
Pathogenesis
Staphylococcus aureus is the most common cause of:
- Skin and soft tissue infections
- Botryomycosis (a condition similar to mycetoma)
- Tropical pyomyositis: caused by Staphylococcus aureus (acute bacterial myositis linked to Group A Streptococcus)
- Osteomyelitis and septic arthritis (most often in the knee)
- Postoperative parotitis
- Paronychia
- Pyomyositis (infection of skeletal muscle): common in tropical regions and among HIV-infected individuals (Staphylococcus aureus is the main agent, except in acute bacterial myositis where Group A Streptococcus is predominant)
- Pneumatocele: thin-walled cavities in the lungs of newborns
- Abscess: including psoas abscess and epidural abscess
- Surgical wound infection
- Folliculitis, furuncle, carbuncle, and hidradenitis suppurativa
- Mastitis and breast abscess (in nursing mothers)
- Toxin-mediated diseases: including toxic shock syndrome, food poisoning, and scalded-skin syndrome
- Infections linked to community-acquired Methicillin Resistant Staphylococcus aureus (CA-MRSA)
- While skin and soft tissues are the most frequent sites for CA-MRSA strains, 5–10% of these strains are invasive and can lead to:
- Necrotizing pneumonia
- Sepsis with Waterhouse-Friderichsen syndrome or purpura fulminans (Staphylococcus aureus is a rare cause; sepsis is usually due to meningococci)
- Necrotizing fasciitis (Staphylococcus aureus is rare; Streptococcus pyogenes is more common)
Endocarditis:
The most frequent cause of native valve endocarditis is Staphylococcus aureus in hospital-acquired cases, while Streptococcus viridans is more common in community-acquired cases.
The most common cause of prosthetic valve endocarditis:
- Early prosthetic valve endocarditis (<12 months): Staphylococcus
- Late prosthetic valve endocarditis (>12 months): Streptococcus viridans
- Overall, the most common cause of prosthetic valve endocarditis: Staphylococcus epidermidis
The most common cause of endocarditis in IV drug users:
- Right-sided – Staphylococcus aureus
- Left-sided – Enterococcus. Staphylococcus aureus
- Overall – Staphylococcus aureus
- The most common cause of subacute endocarditis – Streptococcus viridans
Laboratory Diagnosis
- Direct smear microscopy: Pus cells reveal gram-positive cocci arranged in clusters.
- Culture:
- Nutrient agar: Yields golden yellow pigmented colonies due to the presence of beta carotene.
- Blood agar: Colonies exhibit a narrow zone of β-hemolysis.
- Selective media:
- Mannitol salt agar: Produces yellow colonies as a result of mannitol fermentation.
- Salt milk agar.
- Ludlam’s medium.
- Culture smear microscopy: Displays gram-positive cocci in clusters.
- Biochemical identification:
- Catalase test: Positive result.
- Tests distinguishing staphylococci from micrococci indicate a fermentative pattern.
- Tests differentiating S. aureus (positive) from Coagulase-Negative Staphylococci (CoNs) (negative):
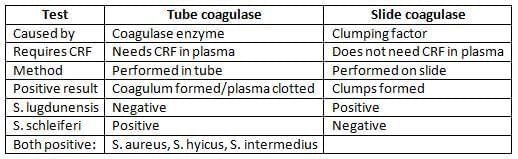
- Coagulase test (both slide and tube): Positive.
- Heat-stable thermonuclease test: Positive.
- DNase test: Positive.
- Phosphatase test: Positive.
- Mannitol sugar fermentation: Positive.
- Potassium tellurite agar: Black colonies indicative.
- Gelatin liquefaction: Positive.
- Protein A detection: Positive.
- Typing of S. aureus:
- Most Common (MC) method for typing: Phage typing using the pattern method.
- National reference centre for phage typing: Maulana Azad Medical College, Delhi.
- Epidemic strain of S. aureus: Phage type 80/81, associated with hospital outbreaks.
Treatment of Staphylococcus aureus Infections
Due to the rapid development of drug resistance in S. aureus, careful selection of antibiotics is crucial.
Parenteral Therapy for Serious Infections:
- Sensitive to penicillin:
- Drug of Choice: Penicillin G
- Sensitive to methicillin:
- Drug of Choice: Nafcillin or Oxacillin
- Resistant to methicillin (MRSA):
- Drug of Choice: Vancomycin (15–20 mg/kg bd)
- Alternate drugs: See text below
Empirical Therapy (When MRSA Status is Unknown):
- Vancomycin with or without an aminoglycoside.
- Vancomycin is recommended when the risk of MRSA is high or in serious situations, such as with a cardiac implant.
Oral Therapy for Skin and Soft Tissue Infections:
- Dicloxacillin, Cephalexin
- Resistant to methicillin (MRSA):
- Alternate drugs: Cotrimoxazole, Doxycycline, Linezolid. (Dosing details should be specified for these medications.)
Drug Resistance in S. aureus
Drug resistance in Staphylococcus aureus (S. aureus) is a significant concern due to its ability to acquire and develop resistance mechanisms, particularly against β-lactam antibiotics, which are commonly used to treat infections caused by this bacterium. Here’s an elaboration on the different types of drug resistance in S. aureus:
- Production of β-lactamase: This enzyme breaks the β-lactam ring, rendering the antibiotic ineffective. This type of resistance is plasmid-coded and can be transferred between S. aureus strains through transduction. More than 90% of S. aureus strains produce β-lactamase.
- Alterations of Penicillin Binding Proteins (PBPs): This mechanism is commonly seen in Methicillin Resistant Staphylococcus aureus (MRSA) strains. In MRSA, the mecA gene alters the PBP in the bacterial cell membrane to PBP-2a, which has a lower affinity for β-lactam antibiotics, making these strains resistant to all β-lactam drugs.
Methicillin Resistant Staphylococcus aureus (MRSA)
- MRSA is specifically mediated by the mecA gene located on the chromosome.
- The mecA gene alters the PBP on the S. aureus cell membrane to PBP-2a, which is crucial for bacterial cell wall synthesis.
- β-lactam drugs typically bind to PBP, blocking cell wall synthesis, but the altered PBP-2a in MRSA strains has a reduced affinity for these antibiotics, leading to resistance.
Community Associated Methicillin Resistant Staphylococcus aureus (CA-MRSA)
- CA-MRSA is characterized by the presence of mecA gene subtypes IV, V, and VI.
- These strains are more virulent and produce the Panton-Valentine (PV) toxin, which contributes to their pathogenicity.
- CA-MRSA is known to cause severe skin and soft tissue infections, including necrotizing fasciitis, which is a life-threatening condition.
Types of MRSA
Community Associated MRSA (CA-MRSA) :
- Mediated by mecA gene subtypes IV, V, VI.
- More virulent and produces PV toxin.
- Causes serious skin and soft tissue infections.
Hospital Associated MRSA (HA-MRSA) :
- Mediated by mecA gene subtypes I, II, III.
- Usually more virulent and produces several toxins like PV toxin.
- Multidrug resistant but generally less virulent.
- Causes serious skin and soft tissue infections and perioperative wound infections in hospitals.
Note: The distinction between CA-MRSA and HA-MRSA is becoming less clear, with many CA-MRSA strains being found in hospitals.
Detection of MRSA
Antimicrobial susceptibility tests such as the disk diffusion test using cefoxitin or oxacillin disks.Treatment of MRSA
- Cefoxitin is the recommended disk.
- Oxacillin screen agar by adding oxacillin 6 µg/ml and NaCl (2–4%) to the medium.
- Polymerase Chain Reaction (PCR) to detect the mecA gene.
- Latex agglutination test to detect PBP-2a.
- Vancomycin is the drug of choice for treating MRSA infections.
- Alternative treatments include:
- Teicoplanin, Linezolid, Quinupristin-dalfopristin, Tigecycline, Oritavancin
- Daptomycin (specifically for endocarditis and complicated skin infections)
- Mupirocin 2% ointment for nasal carriers of MRSA
- In some cases, simple oral antibiotics like tetracycline, erythromycin, or cotrimoxazole may be effective for non-serious infections caused by CA-MRSA strains if they are found to be susceptible.
- It is important to avoid all β-lactam drugs for MRSA treatment. However, some 5th generation cephalosporins like Ceftobiprole, Ceftaroline, and Ceftolozane may be effective against MRSA.
Vancomycin Resistant Staphylococcus aureus (VRSA)
Erroneous and overuse of vancomycin may lead to emergence of resistance to vancomycin, which may be of two types:
- VRSA is characterized by high-grade resistance to vancomycin with a Minimum Inhibitory Concentration (MIC) of ≥ 16 µg/ml.
- VISA exhibits low-grade resistance with an MIC of 4-8 µg/ml.
- VRSA is mediated by the van gene, often acquired from a vancomycin-resistant strain of Enterococcus faecalis through horizontal gene transfer.
- VISA results from an increase in cell wall thickness in S. aureus, which reduces vancomycin efficacy.
Treatment of VRSA/VISA
Effective treatment options for VRSA and VISA include:
- Linezolid
- Telavancin
- Daptomycin
- Quinupristin/dalfopristin
- Vancomycin and teicoplanin are generally not effective for treating VRSA and VISA infections.
S. aureus Carriers
- Healthy individuals, about 25–50% of them, are carriers of S. aureus.
- This bacterium commonly resides in the nose, skin, perineum, armpits, and groin.
- In hospital settings, the primary mode of infection spread is through the hands of healthcare workers.
- The most effective way to prevent infections in hospitals is through proper handwashing.
- For nasal carriers of MRSA, the recommended treatment is Mupirocin 2% ointment.
Resistance to Vancomycin:
- S. epidermidis is recognized for its resistance to vancomycin.
- VRSA (Vancomycin-Resistant Staphylococcus aureus): Minimum Inhibitory Concentration (MIC) ≥ 16 µg/ml, attributed to the Van gene.
- VISA (Vancomycin-Intermediate Staphylococcus aureus): MIC 4-8 µg/ml, resulting from cell wall thickening
Coagulase-Negative Staphylococcus (CoNS)
- Coagulase-negative staphylococci (CoNS) are primarily found as normal flora on the skin.
Staphylococcus Epidermidis
- Most Common Coagulase-Negative Staphylococcus (MC CoNS). Constitutes 60–70% of CoNS.
- Produces a polysaccharide glycocalyx (slime) that facilitates biofilm formation.
- Staphylococcus epidermidis has the ability to adhere to implanted foreign bodies such as valvular shunts and prosthetic devices.
- Infections:
- Endocarditis can occur following the insertion of a valvular prosthesis.
- Infections may also arise in ventricular shunts and lead to the development of stitch abscesses.
Staphylococcus Saprophyticus
- Responsible for urinary tract infections (UTIs) in young sexually active females.
- Resistant to novobiocin.
S. epidermidis Infections:
- Infections caused by S. epidermidis can result in severe health complications.
|
75 docs|5 tests
|
FAQs on Staphylococcus Chapter Notes - Microbiology - NEET PG
| 1. What are the main virulence factors of Staphylococcus aureus that contribute to its pathogenicity? |  |
| 2. How is Staphylococcus aureus typically diagnosed in the laboratory? |  |
| 3. What is the mechanism of resistance in Staphylococcus aureus to β-lactam antibiotics? |  |
| 4. What are VRSA and VISA, and how do they differ in terms of vancomycin resistance? |  |
| 5. What is the significance of Staphylococcus epidermidis and Staphylococcus saprophyticus in clinical settings? |  |
















