Streptococcus, Enterococcus and Pneumococcus Chapter Notes | Microbiology - NEET PG PDF Download
Overview of Streptococci Classification
Streptococci are categorized into three groups based on their hemolytic properties:
- α Hemolytic: This type causes partial hemolysis, resulting in a greenish discoloration. Examples of α hemolytic streptococci include Streptococcus viridans and Streptococcus pneumoniae.
- β Hemolytic: This type leads to complete hemolysis, producing a yellowish discoloration. An example is β hemolytic Streptococcus.
- γ Hemolytic: In this type, no hemolysis occurs. An example is Enterococci.
Lancefield’s Grouping for β Hemolytic Streptococci
β Hemolytic streptococci can be further classified into twenty serogroups based on the carbohydrate antigen present in their cell walls. These groups include A to V, excluding I and J.
Carbohydrate antigens can be extracted using various methods:
- HCl (Lancefield’s method)
- Formamide (Fuller’s method)
- Enzymatic methods (Maxted’s method)
- Autoclaving
Streptococcus Group A (S. pyogenes)
Griffith Typing: This method classifies S. pyogenes based on the type of M protein present, with over 100 different M serotypes identified.
emm Typing: This method classifies S. pyogenes based on the gene coding for M protein, identifying more than 124 different emm genotypes.
Typing of Streptococcus
- Serogrouping (Lancefield’s method): This method categorizes streptococci into 20 groups based on carbohydrate antigens.
- Serotyping (Griffith typing): This method identifies over 100 M types based on the M protein.
- emm Genotyping: This method classifies streptococci into over 124 emm types based on the gene coding for M protein.
Streptococcus pyogenes (Group A)
Virulence Factors
Cell wall antigens:
- Inner thick peptidoglycan layer: Provides rigidity to the cell wall, triggers an inflammatory response, and has thrombolytic activity.
- C-carbohydrate antigen: Specific to the group, located in the middle layer.
- Outer layer: Consists of proteins (M, T, R) and lipoteichoic acid, which assist in adhesion.
- M protein:
- Mediates attachment to epithelial cells and prevents phagocytosis.
- Binds to fibrinogen and neutrophils, causing the release of inflammatory substances that lead to vascular leakage, resulting in streptococcal toxic shock.
- Divided into Class I and Class II; antibodies to Class I M protein are linked to rheumatic fever.
Capsule: Produced by mucoid strains, consists of hyaluronic acid. It aids in adhesion and is anti-phagocytic but is not antigenic.
Streptococcal Pyrogenic Exotoxins (SPE) are linked to:
- Scarlet fever
- Necrotizing fasciitis
- Streptococcal Toxic Shock Syndrome (TSS)
SPE:
- SPE A and C: Act as superantigens and are coded by bacteriophages.
- SPE B: Chromosomally mediated.
- Dick Test: Intradermal injection of SPE causes redness only in children susceptible to scarlet fever.
- Schultz Charlton Reaction: Blanching of rash after injecting anti-SPE antibodies; previously used for diagnosing scarlet fever.
Hemolysins: Streptolysin O and Streptolysin S.
Streptokinase: Fibrinolysin that activates plasminogen, enabling rapid spread by preventing fibrin barrier formation. Used therapeutically for coronary thrombosis.
DNase: Also known as Deoxyribonuclease or Streptodornase (four types: A, B, C, D).
- Diagnostic use: Anti-DNase B > 300–350 U is useful for retrospectively diagnosing skin infections (pyoderma) and acute glomerulonephritis when ASO titer is low.
- Therapeutic use: Preparations with streptodornase and streptokinase can liquefy thick exudates in empyema cases.
Other enzymes:
- Hyaluronidase: spreading factor expressed by non-capsulated strains, such as M type 4 and 22, that breaks down hyaluronic acid in tissues, aiding infection spread.
- Serum opacity factor: a lipoproteinase enzyme.
- NADase, C5a peptidase, and SpyCEP (inactivates IL-8).
Antistreptolysin-O antibodies (ASO):
- Elevated in most streptococcal infections.
- Standard marker for retrospectively diagnosing streptococcal infections, except in glomerulonephritis and pyoderma, where the ASO titer is low.
Streptolysin-O (SL-O) and Streptolysin-S (SL-S):
- SL-O: Oxygen labile and heat labile; strongly antigenic.
- SL-S: Oxygen stable and serum soluble; not antigenic.
- Hemolysis: SL-O causes hemolysis in deep colonies, while SL-S causes hemolysis on blood agar surfaces.
- Cytotoxic: SL-O is cytotoxic for neutrophils, platelets, and cardiac tissue; has leucocidal activity.
ASO and Streptolysin-O: ASO is a standard marker for diagnosing streptococcal infections.
Streptolysin-O is similar to:
- Tetanolysin of Clostridium tetani
- Pneumolysin of S. pneumoniae
- Theta toxin of Clostridium perfringens
- Listeriolysin O of Listeria
- Cereolysin of Bacillus cereus
Suppurative Manifestations
Respiratory Infections:
- Pharyngitis/Sore Throat: The most common cause, accounting for 20–40% of cases.
- Pneumonia and Empyema: Infections that can occur due to S. pyogenes.
- Scarlet Fever: Although now rare, it is characterized by Pastia’s lines and is a known manifestation of S. pyogenes infection.
Skin and Soft Tissue Infections:
- Impetigo (Pyoderma):
- This is the most common cause of skin infections due to S. pyogenes.
- Impetigo is prevalent in children, often linked to poor hygiene and warm climates.
- The infection presents with pustular lesions that eventually form honeycomb-like crusts.
- Notably, impetigo occurs without fever and is painless.
- The condition is associated with higher M types and nephritogenic strains of S. pyogenes.
- Cellulitis and Erysipelas:
- These are among the most common causes of skin infections.
- Cellulitis and erysipelas cause the skin to become tender, bright red, and swollen, with an indurated 'peau d’orange' texture due to superficial lymphatic involvement.
- Patients typically experience fever and chills.
- The malar area of the face is the most common site for these infections, particularly in older individuals.
Deep Soft Tissue Infections:
- Necrotizing Fasciitis:
- S. pyogenes is the leading cause, responsible for 60% of cases.
- This infection spreads rapidly, earning S. pyogenes the nickname "flesh-eating bacteria."
- However, the term "flesh-eating bacteria" applies to various bacteria causing necrotizing fasciitis, not just S. pyogenes.
- Toxic Shock Syndrome (TSS):
- While staphylococcal TSS is more common, bacteremia is more frequent in streptococcal TSS.
- Streptococcal Myositis:
- This condition is mostly caused by S. aureus, but S. pyogenes can also be a causative agent.
Complications:
- Puerperal Sepsis: This is most commonly caused by Group B Streptococcus.
- Other Complications: These include otitis media, quinsy, Ludwig’s angina, post-viral pneumonia, osteomyelitis, and meningitis.
Manifestations of Streptococcus Infections
Scarlet Fever:
- Caused by S. pyogenes, scarlet fever is now uncommon and is characterized by:
- Pharyngitis accompanied by sandpaper-like rashes
- A distinctive strawberry tongue
- Pastia’s lines, which are noticeable rashes found in skin folds
The SPE toxin is implicated in the cause of scarlet fever, as confirmed by a positive Dick test.
S. pyogenes is responsible for both suppurative and nonsuppurative conditions.
Nonsuppurative Complications
- Nonsuppurative complications occur due to the body's immune response to streptococcal infections.
- The immune system reacts to streptococcal antigens, which are similar to human antigens at the molecular level.
- This similarity, known as antigenic cross-reactivity, leads to a situation where antibodies produced against previous streptococcal infections mistakenly target human tissues, causing damage and lesions.
- As a result, several nonsuppurative complications can develop, including:
- Acute rheumatic fever: serious inflammatory condition that can affect the heart, joints, skin, and brain.
- Poststreptococcal glomerulonephritis (PSGN): condition that follows a Streptococcus infection, leading to inflammation of the kidneys and potentially impairing their function.
- Guttate psoriasis: type of psoriasis characterized by small, drop-shaped lesions on the skin, often triggered by infections.
- Reactive arthritis: An inflammatory joint condition that can occur in response to an infection, including streptococcal infections.
- Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcus pyogenes (PANDAS): condition in children where neuropsychiatric symptoms, such as obsessive-compulsive behaviors and tics, are triggered by a streptococcal infection.
Antigenic Cross-Reactivity between Streptococcal Antigens and Human Antigens
Streptococcal Antigens:
- Cell Wall M Protein (of serotypes M1, M5, M6, and M19)
- Cell Wall C Carbohydrate
- Cytoplasmic Membrane
- Peptidoglycan
- Hyaluronic Acid
Human Antigens:
- Myocardium (Tropomyosin and Myosin)
- Cardiac Valves
- Glomerular Vascular Intima
- Skin Antigens
- Synovial Fluid
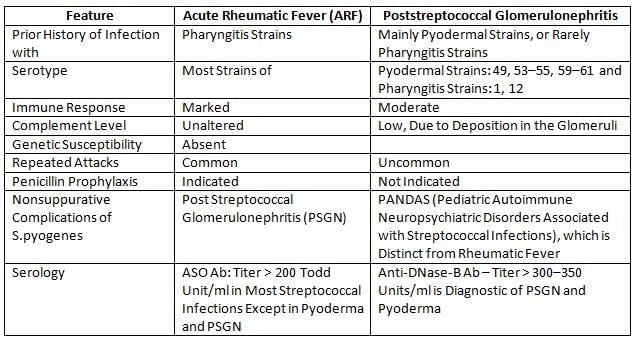
Differences between Acute Rheumatic Fever and Poststreptococcal Glomerulonephritis
Treatment of Necrotizing Fasciitis
- Surgical Debridement: This is the most crucial step in the treatment of necrotizing fasciitis. It involves the surgical removal of all necrotic and infected tissue to halt the spread of the infection.
- Antibiotic Therapy:The following antibiotics are commonly used:
- Penicillin G: This antibiotic is effective against a wide range of bacteria and is often used as a first-line treatment for serious infections.
- Clindamycin: This antibiotic is used in conjunction with penicillin G because it inhibits protein synthesis in bacteria, which can be particularly useful in treating infections caused by toxin-producing bacteria.
Treatment of Rheumatic Fever
- Initial Treatment:
- Benzathine Penicillin G: Administered as an intramuscular (IM) single dose.
- Oral Penicillin V: Given for a duration of 10 days.
- Long-term Maintenance Therapy:
- Penicillin G: Administered monthly.
- Duration of Therapy:
- For 5 years or until 21 years of age: Without Carditis
- For 10 years: With Carditis
- Up to 40 years of age/lifelong: With Residual Heart Disease
Course and Prognosis
- Acute Rheumatic Fever:
- Course: Progressive
- Prognosis: Variable
- Poststreptococcal Glomerulonephritis:
- Course: Spontaneous Resolution
- Prognosis: Good
Hypersensitivity Reaction Type
- Acute Rheumatic Fever: Type II
- Poststreptococcal Glomerulonephritis: Type III
Laboratory Diagnosis of Streptococcus Pyogenes
- Transport Medium: Pike’s medium is used for transporting samples.
- Direct Smear Microscopy: Microscopic examination of samples shows pus cells along with gram-positive cocci arranged in short chains.
- Culture:
- Blood Agar: Cultures on blood agar display pinpoint colonies surrounded by a broad zone of β-hemolysis.
- Selective Media: Uses such as Crystal violet blood agar and PNF media (polymyxin B, neomycin, fusidic acid) for isolation.
- Liquid Media: Granular turbidity with a powdery deposit is observed in liquid media cultures.
- Biochemical Identification: The organism is catalase negative, sensitive to bacitracin, and shows a positive Pyrrolidonyl Arylamidase (PYR) test.
- Typing:
- Lancefield Grouping: Identifies the organism as group A Streptococcus.
- Typing of Group A Streptococcus: Involves Griffith typing and emm typing for further identification.
- Serology:
- ASO (Anti-Streptolysin O) antibodies and Anti-DNase B antibodies are tested.
- ASO antibody titers are typically elevated (> 200 Todd units/ml) in most infections, although high titers may not be conclusive in all cases, such as in pyoderma and post-streptococcal glomerulonephritis (PSGN).
- Other elevated antibodies may include antihyaluronidase and antistreptokinase antibodies.
Treatment of Streptococcal Infection
Penicillin is the preferred treatment for all types of streptococcal infections.
Conditions/Treatment recommended:
- Benzathine penicillin G, IM single dose, or oral penicillin V for 10 days.
- Erysipelas/Cellulitis:
- For mild cases, Procaine penicillin is recommended.
- For severe cases, Penicillin G is recommended.
- Surgical debridement is essential, alongside Penicillin G and Clindamycin.
- Penicillin G plus drainage of empyema is also necessary.
- Penicillin G, Clindamycin, and immunoglobulin (to SPE) are advised.
- Long-term maintenance therapy:
- Monthly penicillin G for:
- 5 years or until 21 years of age, without carditis.
- 10 years with carditis.
- Up to 40 years or lifelong with residual heart disease.
- Monthly penicillin G for:
- Asymptomatic carriers: Benzathine penicillin G, IM single dose, or oral penicillin V for 10 days.
- Pharyngeal carrier: Penicillin V plus rifampicin.
- Rectal carriers: Vancomycin plus rifampicin.
Prophylaxis
- Long-term maintenance therapy with penicillin (or sulfadiazine or erythromycin for those allergic) is essential for children showing early signs of rheumatic fever.
- This treatment helps prevent streptococcal reinfection and further heart damage.
Group B Streptococcus (S. agalactiae)
- Pathogenesis: About 30% of women carry group B Streptococcus in their vagina or rectum, making this infection common in newborns and during pregnancy.
- It is a leading cause of:
- Neonatal sepsis and meningitis: This can be classified as either early onset or late onset.
- Puerperal sepsis and peripartum fever
- Infections in the elderly with conditions like diabetes or cancer. Includes cellulitis, soft tissue infections, UTIs, pneumonia, and endocarditis.
- Laboratory Diagnosis: It can be distinguished from Group A Streptococcus using specific biochemical tests:
- CAMP positive, Hippurate hydrolysis test positive, Bacitracin resistant, and PYR test negative
- Orange pigment production in LIM's medium is typical for some strains.
- β hemolytic colonies are mucoid and slightly larger (2 mm).
- It has a capsular polysaccharide, typed into nine serotypes.
Early and late onset Group B Streptococcus disease in neonates
- Characteristics: Age of onset.
- Early-onset disease: 0–6 days after birth
- Late-onset disease: 7–90 days after birth
- Characteristics: Increased risk following obstetric complications.
- Prematurity and prolonged labour
- Not associated with late-onset disease
- Mode of transmission to the baby:
- During or before birth from the mother's colonised genital tract
- Contact with a colonised mother and nursing staff
- Common clinical manifestations:
- Pneumonia and/or respiratory distress syndrome followed by meningitis
- Bacteremia and meningitis (most common)
- Common serotypes:
- Ia, III, V, II, Ib
- III predominates
- Case fatality rate:
- 4.7% for early-onset
- 2.8% for late-onset
- Characteristics of S. agalactiae
- Bacitracin sensitivity test:
- Sensitive for early-onset
- Resistant for late-onset
- CAMP test:
- 0.5–1 mm, pinpoint for early-onset
- Mucoid, larger (2 mm) for late-onset
Enterococcus
Enterococci were initially grouped with Streptococcus as part of the group-D streptococci. However, they were later reclassified into their own genus, Enterococcus, within the family Enterococcaceae.These bacteria are a natural part of the human gastrointestinal tract. However, their significance as pathogens is growing, especially in hospital settings, primarily due to their ability to resist antibiotics.
Common Species of Enterococcus
- E. faecalis is the species most commonly found in clinical samples.
- E. faecium often exhibits higher levels of antibiotic resistance compared to E. faecalis, although the degree of resistance can vary among different strains.
Clinical Manifestations
- Urinary tract infections (including cystitis, urethritis, pyelonephritis, and prostatitis)
- Bacteremia and mitral valve endocarditis, particularly in IV drug users
- Infections in the abdomen, pelvis, and soft tissues
Group B Streptococcus Characteristics
All cocci are non-motile except for:
- Enterococcus gallinarum
- Enterococcus casseliflavus
Pathogenic Viridans Streptococci Characteristics:
- S. mutans: Known for causing dental caries and plaque formation.
- S. sanguis: Associated with subacute bacterial endocarditis.
- S. milleri group: Linked to the production of suppurative infections.
Laboratory Diagnosis
Enterococci Identification Characteristics:
- Gram-positive oval cocci arranged in pairs, resembling spectacles.
- Non-motile, with exceptions like E. gallinarum and E. casseliflavus.
- Blood agar: Forms non-hemolytic, translucent colonies, rarely showing α or β hemolysis.
- MacConkey agar: Produces small magenta-pink colonies.
- Bile aesculin hydrolysistest: Positive result.
- PYR test: Positive result.
- Growth in the presence of:
- 6.5% NaCl
- 40% bile
- pH 9.6
- Heat tolerance test: Ability to survive 60°C for 30 minutes.
Treatment
Antibiotic Resistance
- Most enterococci strains are resistant to: Penicillins, Aminoglycosides, and Sulfonamides.
- Intrinsic resistance to many antibiotics, although some Cephalosporins may be effective against certain strains, and Cotrimoxazole may also work.
Combination Therapy
- Combination therapy with Penicillin and Aminoglycoside can overcome resistance due to their synergistic effect.
- This combination is the standard treatment for life-threatening enterococcal infections.
- Urinary Tract Infections (UTIs): Monotherapy with Ampicillin or Nitrofurantoin is usually sufficient.
- Vancomycin is typically indicated for resistant cases, but there have been reports of resistance to Vancomycin as well.
Vancomycin Resistant Enterococci (VRE)
Vancomycin resistance in enterococci has been increasingly reported.
- VRE is caused by the Van gene, which alters the target site in the cell wall for vancomycin. This means the D-alanyl-D-alanine side chain of the peptidoglycan layer changes to either D-alanyl-D-serine or D-alanyl-D-lactate, reducing the binding affinity for vancomycin.
- The Van gene has nine genotypes, with the key ones being VanA to VanE.
- Strains with the VanA gene exhibit high-level resistance to both glycopeptides:vancomycin and teicoplanin.
- Strains with the VanB gene show low-level resistance to vancomycin, but some may have varying levels of resistance to teicoplanin.
- E. gallinarum and E. casseliflavus have VanC genes that are chromosomally coded, showing intrinsic resistance to both glycopeptides.
- VRE screening in patients is done using rectal swab cultures on Bile Esculin Azide Agar supplemented with 6 μg/ml vancomycin.
Viridans Streptococci
Viridans streptococci are a group of α-hemolytic bacteria that are generally harmless and commonly found in the mouth. While they are part of the normal oral flora, certain species can be associated with specific health issues.
- S. mutans: This bacterium is a primary contributor to dental caries (tooth decay) and plaque formation in the mouth. It metabolizes sugars and produces acids that can erode tooth enamel, leading to cavities.
- S. sanguis: This species is linked to subacute bacterial endocarditis, a condition where the inner lining of the heart becomes inflamed due to bacterial infection. S. sanguis can enter the bloodstream and settle in the heart, especially in individuals with pre-existing heart conditions.
- S. milleri group: This group of streptococci is known to cause suppurative infections, which are characterized by the formation of pus. Different species within this group can have varying hemolytic patterns, meaning they may break down red blood cells at different rates when grown in a laboratory setting.
Treatment: In general, viridans streptococci are sensitive to penicillin, which is commonly used to treat infections caused by these bacteria. However, in cases of bacteremia (the presence of bacteria in the blood) in neutropenic patients (those with low levels of neutrophils, a type of white blood cell), vancomycin is used as an alternative treatment.
Streptococcus Pneumoniae or Pneumococcus
Virulence Factors and Pathogenesis
S. pneumoniae has various virulence factors, such as:
- Capsular polysaccharide: This component shields the bacteria from being engulfed by immune cells.
- There are more than 90 different capsular serotypes, which can be identified using the Quellung reaction.
- Quellung reaction: This reaction causes the capsule to expand when type-specific antiserum is added to the bacteria along with methylene blue dye.
- The capsule can dissolve into the culture media, tissues, and fluids, which is why it is called a soluble specific substance.
- C-carbohydrate antigen (C-polysaccharide or C-substance): This antigen is specific to the species. C-reactive protein (CRP), found in the blood of patients with acute inflammation, is named because it reacts with pneumococcal C-antigen.
- Pneumolysin: This toxin damages cell membranes and impedes the movement of immune cells towards the site of infection.
- Autolysin: This enzyme breaks down peptidoglycan, leading to the self-destruction of the bacteria. This characteristic results in bile solubility and the distinctive doughnut shape of pneumococcal colonies.
Clinical Manifestation
S. pneumoniae is the primary cause of:
- Lobar pneumonia
- Pyogenic meningitis in individuals of all ages (except newborns)
- Non-invasive conditions such as otitis media and sinusitis.
- Other serious infections that may occur include:
- Osteomyelitis and septic arthritis, which are relatively uncommon.
- Complications arising from pneumonia, including empyema and parapneumonic effusion.
Epidemiology of S. pneumoniae
- Source of Infection: Primarily from the upper respiratory tract of carriers, although patients can also be a source.
- Carrier Rate: Over 90% of children aged 6 months to 5 years carry S. pneumoniae in their nasopharynx.
- Mode of Spread: Mainly through inhaling contaminated droplet nuclei.
Risk Factors:
- Age: Children under 2 years old are at higher risk.
- Medical Conditions: Conditions such as splenectomy, sickle cell disease, and other blood disorders increase the risk due to the spleen's role in clearing bacteria.
- Other Underlying Diseases: Chronic lung, heart, kidney, and liver issues, as well as cochlear implants, diabetes, and immunosuppression (e.g., HIV).
- Viral Infections: Existing viral upper respiratory infections, such as influenza, elevate the risk.
Nature of Infecting Serotypes:
- In Children: Common serotypes include 4, 6B, 9V, 14, 18C, 19F, and 23F.
- In Adults: Common serotypes are 1–8.
- Most Virulent Serotypes: Serotype 3 and Serotype 7, known for forming mucoid colonies.
Virulence Factors of S. pneumoniae:
- Capsule: Detected by the Quellung reaction.
- C carbohydrate antigen: The basis for CRP.
- Autolysin: Responsible for bile solubility and the formation of mucoid colonies.
Common Causes of S. pneumoniae:
- Noninvasive Conditions: Otitis media and sinusitis are commonly caused by S. pneumoniae.
Treatment of Pneumococcal Infections:
- Preferred Treatment: Penicillin G is the first choice for pneumococcal infections.
- Alternative: Ceftriaxone can be used as an alternative treatment.
- Pediatric Treatment: Oral amoxicillin is recommended for children with acute otitis media.
Contraindications to PPV-23:
- Malignancies
- Pregnancy
- Children under 3 years of age
Laboratory Diagnosis
Distinguishing S. pneumoniae from Viridans Streptococci:
- Properties: Morphological and cultural characteristics.
- Morphology: S. pneumoniae are lanceolate or flame-shaped, while viridans streptococci are round or oval.
- Arrangement: S. pneumoniae are gram-positive cocci in pairs, whereas viridans streptococci form long chains.
- On Blood Agar: S. pneumoniae form mucoid or doughnut colonies, while viridans streptococci produce convex-shaped colonies.
- Liquid Medium: S. pneumoniae show uniform turbidity.
- Bile Solubility: S. pneumoniae are bile soluble, while viridans streptococci are bile insoluble.
- Inulin Fermentation: S. pneumoniae are fermenters, whereas viridans streptococci are nonfermenters.
- Optochin: Sensitivity testing differentiates the two.
- Mice Pathogenicity: S. pneumoniae are pathogenic, while viridans streptococci are nonpathogenic.
Current Treatment Guidelines:
- Penicillin G remains the primary treatment choice for pneumococcal infections.
- Cephalosporins, such as ceftriaxone, are viable alternative options for treatment.
Prevention (Capsular Polysaccharide Vaccines)
Pneumococcal Vaccines
There are two types of pneumococcal vaccines available.
23-Valent Pneumococcal Polysaccharide Vaccine (PPV23)
- PPV23 contains polysaccharides from 23 types of pneumococci. It offers protection for around 5 years.
- Indication: It is recommended for individuals with:
- Asplenia or splenic dysfunction
- Diabetes mellitus
- Sickle cell disease or celiac disease
- Cochlear implants
- Chronic lung, heart, kidney, and liver diseases
- Cerebrospinal fluid leaks
- Immunocompromised conditions (e.g., HIV)
- Individuals aged over 65 years
Contraindications to PPV-23 include:
- Malignancies: PPV-23 is not recommended for individuals with certain types of cancer.
- Pregnancy: Pregnant women should not receive this vaccine.
- Children under 3 years: PPV-23 is not effective in young children because their immune systems do not respond well to T-independent antigens.
7-Valent Polysaccharide Conjugate Vaccine (PCV-7)
- This vaccine includes polysaccharides from 7 serotypes, combined with a protein conjugate. It mainly covers childhood serotypes such as 6B, 9V, 14, 19F, 23F, and 18C:
- The addition of a protein conjugate enhances the immune response to the polysaccharides, making it suitable for children under 3 years.
- Schedule:. doses are given at 2, 4, 6, and 12–15 months of age.
- As antibiotic resistance is commonly observed in pneumococcal serotypes 6, 9, 14, 19, and 23, the use of PCV-7 has been effective in reducing this resistance.
|
75 docs|5 tests
|
FAQs on Streptococcus, Enterococcus and Pneumococcus Chapter Notes - Microbiology - NEET PG
| 1. What are the main virulence factors of Streptococcus pyogenes? |  |
| 2. What are some nonsuppurative complications associated with Streptococcus pyogenes infections? |  |
| 3. How is Streptococcus pyogenes diagnosed in the laboratory? |  |
| 4. What treatments are available for streptococcal infections? |  |
| 5. What measures can be taken for the prophylaxis of streptococcal infections? |  |




















