NEET Exam > NEET Notes > Biology Class 12 > The Male Reproductive System
The Male Reproductive System | Biology Class 12 - NEET PDF Download
Location and Components
- The male reproductive system is found in the pelvis and comprises a pair of testes along with accessory ducts, glands, and external genitalia.
- The testes are located outside the abdominal cavity in a pouch called the scrotum, which helps maintain a temperature 2–2.5°C lower than the normal body temperature, essential for sperm production.
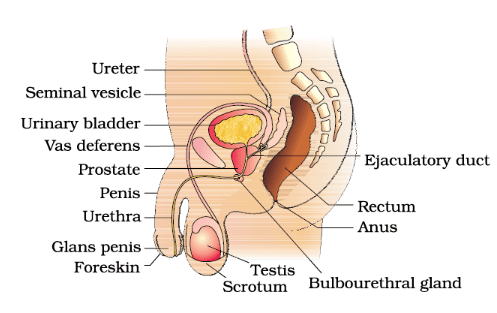 Diagrammatic sectional view of male pelvis showing reproductive system
Diagrammatic sectional view of male pelvis showing reproductive system
Testes Structure
- Each testis is oval-shaped, measuring about 4 to 5 cm in length and 2 to 3 cm in width.
- The testis is covered by a dense covering and contains approximately 250 compartments called testicular lobules.
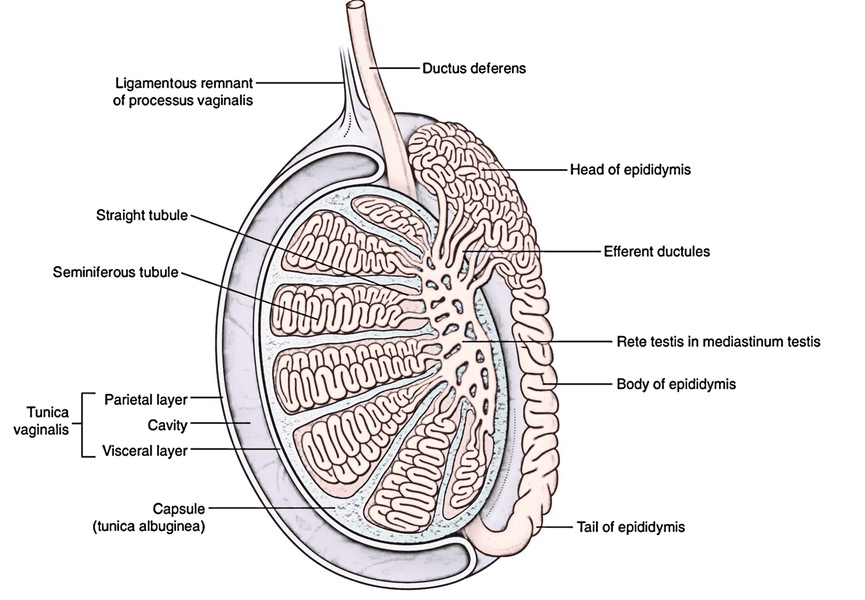 Testes Structure in Detail
Testes Structure in Detail
- Each lobule houses one to three seminiferous tubules, where sperm are produced.
- These tubules are lined with male germ cells(spermatogonia) and Sertoli cells.
- The germ cells undergo meiosis to form sperm, while Sertoli cells provide nutrients to the germ cells.
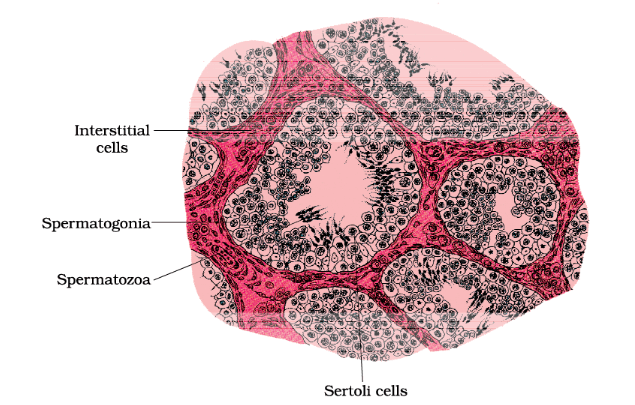 Diagrammatic sectional view of seminiferous tubule
Diagrammatic sectional view of seminiferous tubule
- The spaces between the tubules, called interstitial spaces, contain small blood vessels and Leydig cells, which produce androgens, a type of testicular hormone.
Question for The Male Reproductive SystemTry yourself: Which cells in the testes provide nutrients to the germ cells during sperm production?View Solution
Accessory Ducts
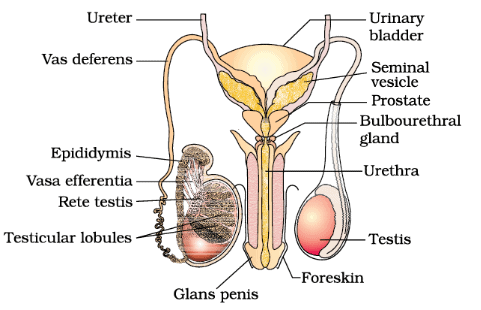 Male reproductive system (part of testis is open to show inner details) and Accessory Ducts
Male reproductive system (part of testis is open to show inner details) and Accessory Ducts
- The male sex accessory ducts include the rete testis, vasa efferentia, epididymis, and vas deferens.
- The seminiferous tubules connect to the vasa efferentia through the rete testis.
- The vasa efferentia lead to the epididymis, located on the posterior surface of each testis.
- The epididymis connects to the vas deferens, which ascends into the abdomen, loops over the urinary bladder, and eventually opens into the urethra as the ejaculatory duct.
Urethra and Penis
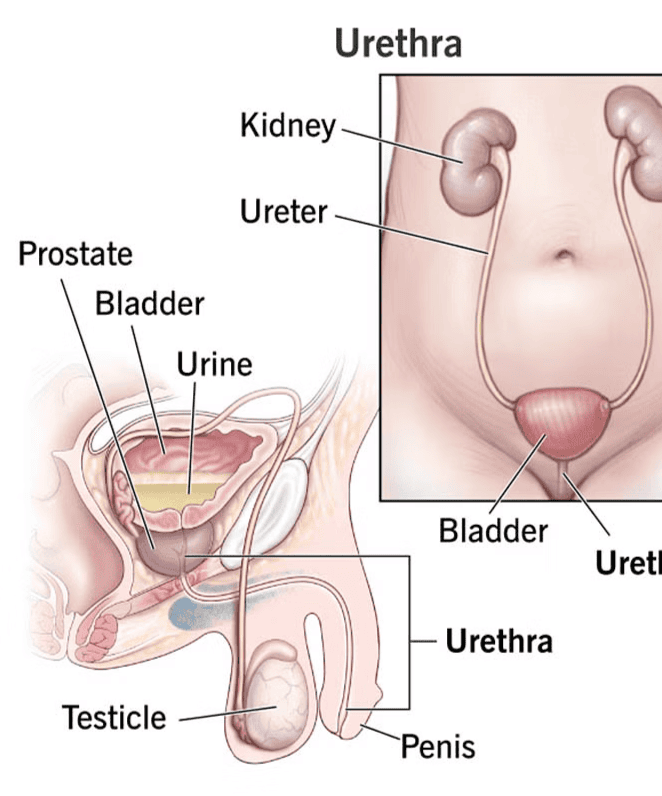 Urethra and Penis
Urethra and Penis
- The urethra originates from the urinary bladder and extends through the penis to its external opening, the urethral meatus.
- The penis, the male external genitalia, is made of special tissue that enables erection to facilitate insemination.
- The enlarged end of the penis, called the glans penis, is covered by a loose fold of skin known as the foreskin.
Accessory Glands
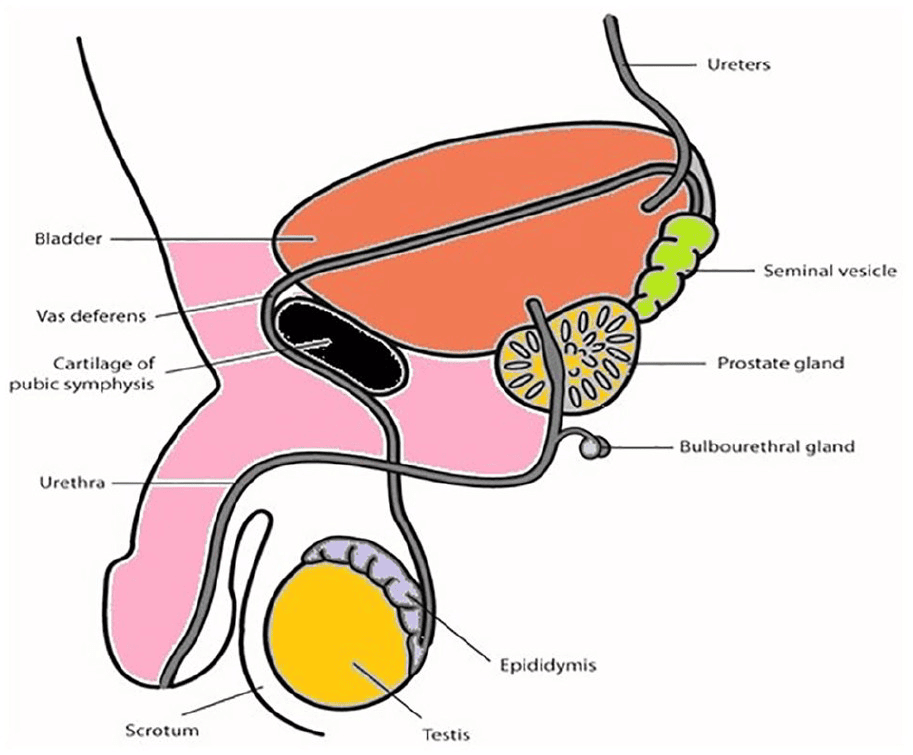 Accessory Glands of Male Reproductive system
Accessory Glands of Male Reproductive system
- The male accessory glands include seminal vesicles, prostate, and bulbourethral glands.
- Their secretions form the seminal plasma, which is rich in fructose, calcium, and various enzymes.
- The secretions from the bulbourethral glands also aid in the lubrication of the penis.
The document The Male Reproductive System | Biology Class 12 - NEET is a part of the NEET Course Biology Class 12.
All you need of NEET at this link: NEET
|
59 videos|290 docs|168 tests
|
FAQs on The Male Reproductive System - Biology Class 12 - NEET
| 1. What are the main components of the male reproductive system? |  |
Ans.The main components of the male reproductive system include the testes, which produce sperm and hormones; the epididymis, where sperm mature; the vas deferens, which transports sperm; the seminal vesicles and prostate gland, which produce seminal fluid; and the penis, which delivers sperm during intercourse.
| 2. How does sperm production occur in the male reproductive system? |  |
Ans.Sperm production, or spermatogenesis, occurs in the seminiferous tubules of the testes. It involves the division and maturation of germ cells into sperm cells, which takes about 64 to 72 days, followed by storage in the epididymis until ejaculation.
| 3. What is the role of testosterone in the male reproductive system? |  |
Ans.Testosterone is the primary male sex hormone produced by the testes. It plays a crucial role in the development of male reproductive tissues, the production of sperm, and the maintenance of secondary sexual characteristics such as muscle mass, body hair, and voice depth.
| 4. What are common disorders of the male reproductive system? |  |
Ans.Common disorders of the male reproductive system include erectile dysfunction, infertility, prostate enlargement (benign prostatic hyperplasia), prostatitis (inflammation of the prostate), and testicular cancer. These conditions can affect sexual health and reproductive capabilities.
| 5. How can men maintain a healthy reproductive system? |  |
Ans.Men can maintain a healthy reproductive system by adopting a balanced diet, exercising regularly, avoiding tobacco and excessive alcohol use, managing stress, practicing safe sex, and having regular check-ups with a healthcare provider for early detection of any potential issues.
Related Searches