Medicine and Disease | History for Year 6 PDF Download
| Table of contents |

|
| Ideas About the Cause of Disease in Modern Britain |

|
| Medical Treatments in Modern Britain |

|
| Prevention of Disease in Modern Britain |

|
| Lung Cancer: Case Study |

|
Ideas About the Cause of Disease in Modern Britain
Progress in Modern Ideas about the Causes of Disease - Timeline & Summary
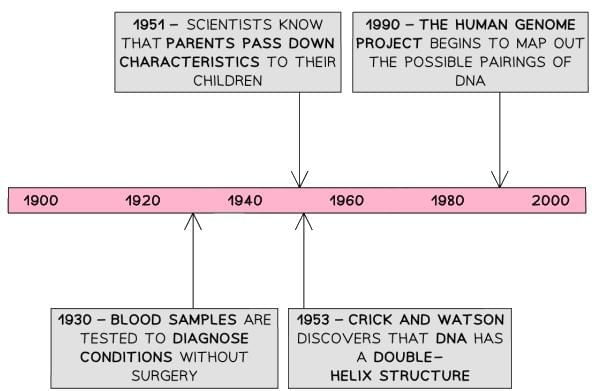
- The understanding of disease causation advanced significantly in the 20th century. Louis Pasteur’s Germ Theory established that microorganisms are a primary cause of many diseases, leading to the development of cures for epidemic diseases like diphtheria, which greatly reduced their prevalence and impact in the 20th and 21st centuries. In the 1950s, scientists recognized that not all diseases are caused by germs, identifying that some illnesses are congenital, passed down through genetics. The discovery of DNA’s double helix structure by Francis Crick and James Watson in 1953 was pivotal, enabling researchers to understand how genes are inherited and fueling ongoing studies into the human genome. These studies aim to uncover cures for complex diseases like cancer and potentially eliminate genetic disorders from society.
- Lifestyle also emerged as a significant factor in disease causation. Modern understanding echoes some medieval concepts, such as those in Regimen Sanitatis, emphasizing the importance of health maintenance. Scientific evidence now links habits like smoking and excessive sugar consumption to conditions such as heart disease and Type 2 diabetes, empowering individuals to adopt preventive measures. Technological advancements in the 20th century, including X-ray machines, CT scans, ECGs, and blood pressure monitors, have enhanced diagnostic accuracy by allowing non-invasive examination of internal organs and monitoring of vital signs. Blood tests and glucose monitoring further aid in detecting abnormal levels of substances in the body. Laboratories analyze biopsies and patient samples, improving diagnostic precision.
- Despite these advancements, some diseases, such as cancer, remain incompletely understood due to their complexity. Genetic analysis offers insights into disease causes but has limited practical applications for treatment or prevention. Epidemic diseases, like COVID-19 in 2020, continue to challenge society, highlighting the ongoing evolution of medical knowledge.
DNA & The Influence of Genetics on Disease
Watson, Crick, and the Discovery of the Human Genome
- In 1951, Rosalind Franklin and Maurice Wilkins produced an X-ray image of DNA, providing critical insights.
- Francis Crick (English) and James Watson (American) collaborated at Cambridge University, driven by a shared interest in human biology.
- Inspired by Franklin and Wilkins’ X-ray, Crick and Watson began studying DNA’s structure, with Franklin correcting their initial model and Wilkins providing clearer DNA photographs.
- In 1953, Crick and Watson identified DNA’s double helix structure and theorized its ability to “unzip” for replication, publishing their findings in April 1953.
The Human Genome Project
- Launched by Watson in 1990, the Human Genome Project involved eighteen global scientific teams mapping DNA combinations to understand hereditary diseases like haemophilia.
- The first draft was completed in 2000, enabling scientists to identify DNA sequences linked to diseases, such as the BRCA gene, which increases breast cancer risk (e.g., actress Angelina Jolie, who opted for a mastectomy due to carrying the BRCA gene).
Factors that Helped the Development of Genetics

The Limitation of DNA
- Most treatments do not yet utilize DNA knowledge, though understanding of disease causes has improved.
- Genetic therapy, which explores DNA-based treatments, is a rapidly evolving field but remains in early development stages.
The Influence of Lifestyle on Disease
By the 1950s, scientists linked lifestyle to health outcomes, a connection still being researched as new habits emerge in the 21st century.
Smoking
- Smoking was fashionable in the 1920s, but a 1950 study confirmed its link to increased lung cancer rates, particularly among men who smoked more frequently.
- Smoking is now known to increase risks of high blood pressure, lung, throat, and mouth cancers, heart disease, and dental issues.
- Late 1990s/early 2000s studies highlighted second-hand smoke risks, showing that non-smokers exposed to tobacco smoke are more likely to develop asthma and lung cancer.
Diet
- Medieval texts like Regimen Sanitatis and the Four Humours theory recognized diet’s importance, warning against overeating and noting certain foods’ healing properties.
- Modern science explains why diet matters: excessive sugar can cause Type 2 diabetes, high saturated fat intake leads to heart disease, and deficiencies in vitamins or minerals (e.g., iron from meat, beans, or leafy greens) can cause conditions like iron deficiency anemia.
The Influence of Other Lifestyle Factors
- Alcohol: Excessive drinking can damage the liver and kidneys.
- Sharing Bodily Fluids: Unprotected sex or using contaminated needles increases the risk of STIs like HIV.
- Tanning: Overexposure to sun or tanning beds heightens the risk of skin cancer.
Medical Scans & Blood Tests
Technological advancements since 1900 have improved disease diagnosis:

Self-Monitoring of Health
- 21st-century technology enables self-monitoring, such as blood sugar checks for diabetes management via injections or automated insulin pumps.
- Knowledge of disease transmission has led to preventive measures like antibacterial hand gels, masks, and gloves, widely used during COVID-19.
- Awareness of lifestyle’s impact allows individuals to take preventive actions to reduce disease risk.
Medical Treatments in Modern Britain
Approaches to Treatment in the 20th Century - Summary
Since the Renaissance, chemical experimentation has driven medical treatment development, aided by technological advances that allow study of molecular structures, leading to more effective chemical cures. Early 20th-century scientists sought treatments targeting harmful microorganisms without damaging the body, with Paul Ehrlich and Gerhard Domagk pioneering “magic bullets” for diseases like syphilis and blood poisoning. This concept spurred antibiotic development, notably Alexander Fleming’s accidental discovery of penicillin in 1928, which Howard Florey and Ernst Chain mass-produced by 1941 with government support during World War II. This marked a shift from laissez-faire attitudes, as governments recognized medicine’s strategic importance. Before 1945, minor infections often led to death; today, such outcomes are rare in Britain.
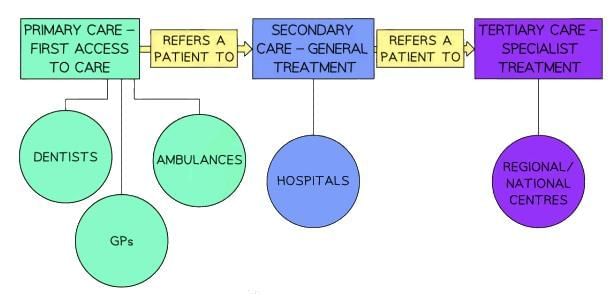
The establishment of the National Health Service (NHS) in 1948 transformed healthcare access, ensuring free care for all and integrating general practitioners (GPs) and hospitals. Advances in surgery, supported by X-rays, robotic surgery, and hypodermic needles, enhanced NHS care. However, challenges persist: some cancers lack specialized treatments, microbes develop drug resistance, NHS access issues remain, and new diseases like COVID-19 demand ongoing innovation.
Antibiotics - Ehrlich & Domagk
‘Magic Bullets’
- By the 20th century, the concept of antibodies was understood, with vaccinations triggering immune responses.
- Scientists hypothesized that the body could produce antibodies to chemical compounds.
- A “magic bullet” was a chemical treatment targeting harmful bacteria without harming the body.
Ehrlich and Syphilis
- Syphilis was a persistent issue in the 19th and 20th centuries, affecting military recruitment during the Boer War (1880–1902) and World War I (1914–1918).
- Traditional mercury treatments were outdated, prompting Paul Ehrlich to test over 600 arsenic compounds by 1907.
- In 1909, Japanese scientist Hata identified compound 606 (Salvarsan 606) as a cure for syphilis, the first “magic bullet.”
Domagk and Antibiotics
- In 1932, Gerhard Domagk found that Prontosil, a red dye, killed infections in mice and later saved his daughter from blood poisoning.
- At Queen Charlotte’s Maternity Hospital, Prontosil reduced puerperal fever mortality from 20% to 4.7%, encouraging further antibiotic research.
Fleming and Penicillin
Fleming’s Discovery of Penicillin
- Alexander Fleming, a Scottish doctor at St. Mary’s Hospital, London, pioneered Salvarsan 606 for syphilis and worked in World War I battlefield hospitals.
- In the 1920s, he studied Staphylococcus, a deadly bacterium resistant to existing treatments.
- In 1928, Fleming accidentally discovered penicillin when mould in a petri dish prevented Staphylococcus growth, echoing medieval observations of mould’s healing properties.
- His 1929 publication was overlooked, as scientists prioritized chemical cures and his initial tests showed penicillin’s ineffectiveness in blood.
Florey Chain and the Development of Penicillin
- Howard Florey (Australian) and Ernst Chain (German) at Oxford Medical School rediscovered Fleming’s work in 1939.
- In 1940, they successfully tested penicillin on mice, saving four treated mice infected with Staphylococcus while untreated mice died.
- World War II prompted British government funding (£25, equivalent to £1100 today) for their research, driven by the need to prevent infection-related deaths.
- In 1941, a human trial on policeman Albert Alexander, suffering from septicaemia, showed recovery until penicillin supplies ran out, leading to his death, but proving penicillin’s efficacy.
Mass Production of Penicillin
- In 1941, Florey sought American pharmaceutical support, as British companies lacked resources during World War II.
- Penicillin production involved growing mould in beer vats, a slow process initially yielding only ten doses after a year.
- The U.S. government funded 21 pharmaceutical companies, and British firms began production in 1943, making penicillin vital by the war’s end.
Factors in Penicillin Development
- Government: British and U.S. funding supported Florey and Chain’s research.
- Technology: Beer vats and milk churns enabled mass production.
- Attitudes: World War II urgency reduced the need for extensive trials.
- Science: Observations of penicillin’s effects on Staphylococcus and collaborative research at Oxford were key.
- Individuals: Fleming’s discovery, Florey and Chain’s human trials, and Florey’s advocacy for mass production were critical.
Modern Development of Antibiotics
- Penicillin inspired research into other moulds, with Selman Waksman discovering Streptomycin for tuberculosis in 1943.
- Dorothy Hodgkin mapped penicillin’s structure in 1945, enabling synthetic antibiotics, with John C. Sheehan creating the first synthetic penicillin in 1957.
- Antibiotics are now administered via capsules or hypodermic needles for precise dosing.
- Overprescription in the 1950s led to resistance, with penicillin-resistant strains emerging in 1942. A 2018 report noted 20% of antibiotic prescriptions in England were incorrect, and MRSA remains a public health threat, though treatable with alternative antibiotics.
Modern Surgery - Transplants, Transfusions & Keyhole Surgery
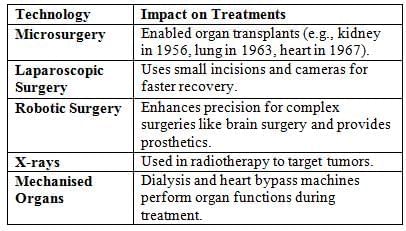
Modern surgery is safer and more diverse, addressing blood loss, pain, and infection (resolved by Lister and Simpson’s work and mid-20th-century blood transfusions). Complex procedures like brain surgery and organ transplants are now possible.
New Surgical Technology
Medical Care: The Impact of the NHS
- In the 1906 general election, the Liberal Party secured victory and introduced several reforms to enhance medical care. In 1907, free medical inspections were provided for schoolchildren.
- The National Insurance Act of 1911 offered health insurance to male workers earning less than £160 annually, granting them up to 25 weeks of sick pay. By 1912, school-aged children gained access to free medical treatments. However, many people still lacked adequate medical care. Healthcare provision varied by local authority, and the National Insurance Act excluded women and workers’ families.
- Outside London and South East England, hospital availability was limited, and existing 19th-century facilities needed modernization. Many individuals continued to pay for doctor visits, leading them to rely on herbal remedies like Beechams from pharmacies.
Structure of the NHS
- In 1948, Aneurin Bevan’s Labour government established the National Health Service (NHS), offering free healthcare to all.
- The NHS was financed through workers’ National Insurance contributions, a tax that remains in place.
- The government centralized existing hospitals and medical services under its control to deliver this universal healthcare system.
The Impact of the NHS

The Extent of Change in Care & Treatment
Improved Access to Care
- The 1919 Ministry of Health reflected government commitment to healthcare standards.
- The NHS ensured free care for all, shifting hospitals from elderly care to disease treatment.
Improvements to Treatments
- Infectious disease deaths dropped from 25% in 1900 to under 1% by 1990.
- Herbal remedies were replaced by chemical “magic bullets” post-1945.
Issues with Treatments
- Viruses are hard to vaccinate against, requiring annual flu vaccines.
- Microbes develop resistance, as seen with COVID-19 strains.
- Complex diseases like cancer lack specialized treatments, and lifestyle-related diseases like heart disease are rising.
Prevention of Disease in Modern Britain
Modern Approaches to the Prevention of Disease - Timeline & Summary
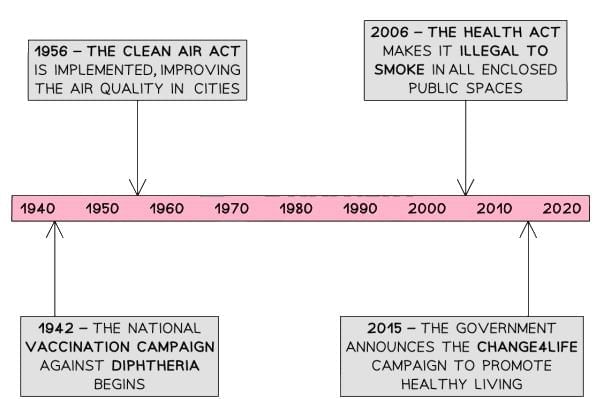
In the 20th and 21st centuries, governments adopted proactive roles in disease prevention, driven by clearer scientific understanding and public demand. The success of smallpox vaccination led to compulsory programs for diseases like diphtheria and tetanus, now rare in Britain. Building on the 1875 Public Health Act, laws addressed air pollution and second-hand smoke (e.g., 2006 anti-smoking laws). Campaigns like Change4Life promoted healthy lifestyles. However, hereditary diseases remain difficult to prevent, and resistance to government intervention, such as vaccine refusal, has increased childhood diseases like measles. Obesity rates suggest limited success of healthy living campaigns.
End of Laissez-Faire Attitudes
Governments abandoned laissez-faire approaches due to:
- Understanding Disease Causes: Germ Theory’s acceptance in the late 19th century clarified disease mechanisms.
- Prevention Methods: Compulsory vaccinations, public health laws, and campaigns educated the public.
New Approaches to Prevention: Mass Vaccinations
- Smallpox’s success inspired vaccination programs for:
- Diphtheria (1942): Eliminated as a major disease by the mid-20th century.
- Polio (1962): Reduced from 8000 annual cases in the 1950s to none by 1984.
- HPV (2008): Reduced cervical cancer cases by 87% by 2021.
- Vaccine refusal stems from distrust in government, medical professionals, or vaccine safety, reducing herd immunity.
New Approaches to Prevention: Government Legislation
- Clean Air Acts (1956, 1968): Addressed smog from coal burning, creating smokeless zones and subsidizing gas/electricity use. Air pollution persists, with cases like Ella Adoo-Kissi-Debrah’s 2020 death linked to excessive pollution.
- Anti-Smoking Laws (2006): Banned smoking in public spaces, reducing second-hand smoke exposure by nearly 70% (1996–2007).
- Other Measures: Fluoride in water to prevent tooth decay and ULEZ in London (2019) to limit car emissions.
New Approaches to Prevention: Government Lifestyle Campaigns
- 21st-century science linked lifestyle to disease, prompting campaigns to reduce NHS strain.
- Initiatives include anti-smoking (Stoptober), anti-binge drinking, and healthy eating campaigns (Change4Life, 2015).
- Technology like TV, radio, and apps (e.g., SugarSmart) spreads these messages.
- Public Health England (now the Office for Health Improvement and Disparities and UK Health Security Agency) supports these efforts.
Lung Cancer: Case Study
The Fight Against Lung Cancer in the 21st Century - Summary
Lung cancer is Britain’s second most common cancer, primarily affecting those over 40, with the 70–74 age group most impacted. Between 2016–2018, over 48,000 cases were reported, with a 10% ten-year survival rate. Approximately 85% of cases are linked to smoking, with rare cases caused by chemicals like radon gas. Lung cancer was rare in the 19th century (1% of tumors), rising to 10% by 1918 and 14% by 1927 due to increased smoking, fueled by tobacco companies’ aggressive marketing. By 1950, 80% of British men smoked, and a 1950 study confirmed smoking’s link to lung cancer, with 26,000 deaths by 1973. The government now uses advanced diagnostics, treatments, and laws to combat lung cancer, though it remains a public health challenge.
Diagnosis of Lung Cancer
- Lung cancer is difficult to diagnose due to symptom misidentification and late tumor detection.
- No national screening program exists; early diagnosis relied on X-rays, which were inaccurate due to low detail.
- Modern diagnosis involves:
- CT Scan: Uses dye for clearer lung images.
- PET-CT Scan: Injects radiation to identify cancerous cells.
- Bronchoscopy: A camera collects lung cell biopsies.
- Cancer is staged from 1 (small, localized) to 4 (advanced, spread), guiding treatment plans.
Treatment of Lung Cancer: Science & Technology
- Radiotherapy: Targets tumors with radiation to shrink or destroy them, effective for various tumor sizes.
- Chemotherapy: Uses drugs over months to kill tumors or manage symptoms, with side effects like sickness, hair loss, and infection risk.
- Transplants: Replace cancerous lungs with donor lungs, though one lung is sufficient for survival.
- Genetic Research: Explores pharmacogenomics to tailor treatments to individual DNA, as tumors respond variably to chemotherapy.
Prevention of Lung Cancer: Government Action
- The British government was initially reluctant to confront the tobacco industry due to the £4 billion in tax revenue it generated and the employment provided by tobacco companies.
- Having never previously urged citizens to abandon a habit, the government faced a challenge. However, with smoking-related deaths costing the NHS £165 million annually, action became necessary.
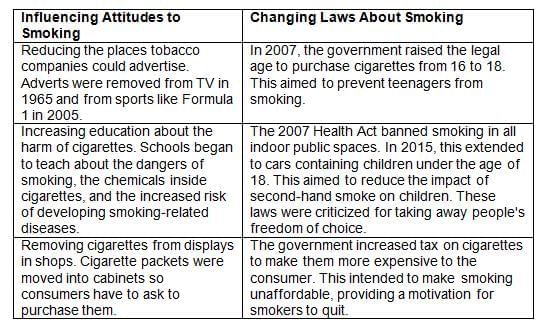
- The government adopted a two-pronged approach to prevent lung cancer: first, by raising public awareness about the health risks of smoking, and second, by enacting laws to enforce behavioral changes with penalties for non-compliance.
How Did the Government Influence and Change the Behaviour Around Smoking in the 21st Century?
|
3 videos|69 docs
|