MCAT Exam > MCAT Notes > Psychology and Sociology for MCAT > What is obsessive compulsive disorder (OCD)?
What is obsessive compulsive disorder (OCD)? | Psychology and Sociology for MCAT PDF Download
| Table of contents |

|
| Obsessive Compulsive Disorder (OCD) |

|
| Communication Breakdown in OCD |

|
| Symptoms of OCD |

|
| Risk Factors and Causes |

|
| Prevalence of OCD |

|
| Recent Discoveries and Future Prospects |

|
Obsessive Compulsive Disorder (OCD)
Obsessive Compulsive Disorder (OCD) is a complex mental health condition that is often misunderstood in today's society. Contrary to popular belief, simply liking cleanliness or having a unique way of organizing things does not equate to having OCD. OCD is characterized by a disturbance in thought patterns, leading to negative emotions and impacting a person's ability to function normally. It involves uncontrollable intrusive thoughts, negative emotions such as guilt and anxiety, and repetitive ritualistic behaviors or actions.Understanding Information Processing in the Brain
The human brain can be likened to a supercomputer, constantly receiving and processing new data from our experiences to help us make sense of the world. Different regions of the brain are responsible for various aspects of information processing. For instance, one area may handle sensory input, while another prioritizes thoughts and emotions. When these components work harmoniously, we can effectively process information.
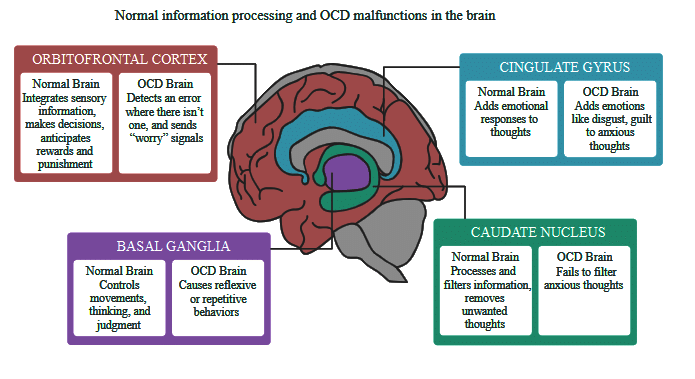
Communication Breakdown in OCD
In individuals with OCD, there can be a breakdown in communication between different parts of the brain responsible for translating information into thoughts and actions. Key regions involved in this process include the orbitofrontal cortex, caudate nucleus, cingulate gyrus, and basal ganglia. Malfunctioning in these areas leads to inappropriate information passing through the system, overwhelming the individual with intrusive thoughts and compulsive behaviors.
Symptoms of OCD
Those diagnosed with OCD typically experience two main symptoms: obsessions and compulsions.
- Obsessions are recurring thoughts, ideas, mental images, or beliefs that are intrusive and often disturbing, causing significant emotional distress and dysfunction. These obsessive thoughts can interfere with daily tasks, making it challenging for individuals to focus. Unlike most people who can dismiss upsetting thoughts, those with OCD struggle to control their obsessions. Common obsessions include fears of contamination, forgetting something important, or causing harm to oneself or others. Additionally, excessive beliefs regarding perfection, symmetry, morality, or superstitions can also manifest.
- Compulsions are repetitive behaviors or rituals that individuals feel compelled to perform. They are usually attempts to alleviate the anxiety and distress caused by obsessions. For example, someone with an obsessive fear of germs might engage in compulsive hand washing. These behaviors can be mental, such as repeating words in one's head, or physical, like tapping a surface a specific number of times. Compulsions often lack rationality and do not directly address the person's concerns. Common compulsions include counting, checking, cleaning excessively, and following strict routines or rituals.
- Although individuals with OCD often recognize that their obsessions and compulsions are irrational, they still struggle to control them. As the symptoms become more complex, rituals can consume hours of their day, severely impacting their daily lives, relationships, work, and school.
Risk Factors and Causes
The development of OCD is usually not attributable to a single cause. Instead, it arises from a combination of various risk factors:
- Genetics: Having a close family member with OCD increases an individual's likelihood of developing the disorder.
- Psychological factors: People with symptoms of other mental illnesses, especially anxiety disorders and mood disorders like depression, have an increased risk of developing OCD. Certain personality traits like perfectionism, high moral standards, and a strong sense of responsibility are also associated with OCD.
- Illnesses during childhood: In children, an infection with streptococcus, the bacteria causing strep throat, can trigger the sudden onset of OCD.
- Other illnesses or injuries: Physical illnesses or brain injuries can also induce symptoms of OCD. Traumatic brain injuries, specific viruses, and brain tumors have been linked to the disorder.
Prevalence of OCD
OCD is one of the most common mental disorders, affecting approximately 2% of adults in the United States at some point in their lives. More than half of those diagnosed with OCD experience severe symptoms that significantly disrupt their daily functioning. While men and women are diagnosed with OCD at similar rates, males often exhibit symptoms during childhood. Around 25% of OCD cases occur in children under the age of 18, and one-third of adults with OCD developed the disorder in their youth.
Managing OCD and Available Treatments
While the initial onset of OCD is not preventable, patients can manage their symptoms through appropriate treatments. Recognizing triggering situations or events and maintaining a symptom diary can help individuals seek timely treatment if symptoms worsen. It is crucial for patients to continue taking their prescribed medications as instructed. Prematurely stopping medication can be dangerous, as approximately 20% of patients become unresponsive to previously effective medications due to discontinuation.
Treatment for OCD often involves a combination of medication and psychotherapy tailored to each patient's specific needs and symptoms.
- Medications: Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), are commonly used to treat OCD. These medications aim to restore proper communication between the brain regions involved in OCD, such as the orbitofrontal cortex, caudate nucleus, cingulate gyrus, and basal ganglia. SSRIs increase serotonin levels, enhancing information processing in these areas. On average, antidepressants can reduce OCD symptoms by 40-60%.
- Psychotherapy: Cognitive Behavioral Therapy (CBT) is one of the most effective psychotherapeutic approaches for OCD. CBT focuses on identifying and challenging maladaptive thoughts, emotions, beliefs, and behaviors, replacing them with more adaptive ones. Exposure and Response Prevention (ERP), a specific form of CBT, helps patients confront situations that trigger their obsessions and resist engaging in compulsive behaviors. CBT and ERP typically lead to a significant reduction of 60-80% in OCD symptoms.
Recent Discoveries and Future Prospects
Scientists have recently made an intriguing connection between a gene responsible for certain kidney disorders and symptoms of OCD. This discovery holds promise for the development of a urine test that could identify babies and young children at risk of developing OCD due to genetic factors. Early identification could facilitate timely intervention and potentially lead to better outcomes for children with a genetic predisposition to the disorder.
Conclusion
OCD is a complex mental health condition characterized by intrusive thoughts, negative emotions, and repetitive ritualistic behaviors. Understanding the interplay between brain regions involved in information processing sheds light on the communication breakdown observed in individuals with OCD. Proper diagnosis and tailored treatments, such as medication and psychotherapy, can significantly alleviate symptoms and improve daily functioning. Ongoing research and discoveries provide hope for further advancements in identifying and managing OCD, offering individuals a better quality of life.
The document What is obsessive compulsive disorder (OCD)? | Psychology and Sociology for MCAT is a part of the MCAT Course Psychology and Sociology for MCAT.
All you need of MCAT at this link: MCAT
|
339 videos|14 docs|42 tests
|
Related Searches





















