Short & Long Question Answers with Solution: Breathing and Exchange of Gases - NEET PDF Download
Short Answer Type Questions
Q1: What is Respiratory Quotient?
Ans: The ratio between the volume of carbon dioxide expelled and the volume of oxygen taken in during the process of cellular respiration is known as the respiratory quotient, often abbreviated as RQ. It is also referred to as the respiratory ratio.
The formula for calculating the Respiratory Quotient is as follows:
RQ = Volume of carbon dioxide eliminated / Volume of oxygen consumed.
Q2: Name the organs of respiration in cockroach, earthworm and birds?
Ans:
- Cockroaches breathe through tiny openings located on the sides of their bodies, known as spiracles.
- Earthworms engage in respiration through their skin.
- Birds carry out respiration primarily through their lungs.
Q3: List the following steps in a sequential manner for the completion of the respiration process.
(a) Diffusion of oxygen and CO2 across the alveolar membrane
(b) Transportation of gases by blood
(c) Utilization of oxygen for catabolic reactions by the cells and hence the resultant release of CO2
(d) Pulmonary ventilation through which atmospheric air is drawn in and carbon dioxide-rich alveolar air is given out
(e) Diffusion of oxygen and carbon dioxide between tissues and blood
Ans: (d) Pulmonary ventilation through which atmospheric air is drawn in and carbon dioxide-rich alveolar air is given out
(a) Diffusion of oxygen and CO2 across the alveolar membrane
(b) Transportation of gases by blood
(e) Diffusion of oxygen and CO2 between tissues and blood
(c) Utilization of oxygen for catabolic reactions by the cells and hence the resultant release of CO2.
Q4: Explain why the diffusion of carbon dioxide by the diffusion membrane per unit difference in partial pressure is much greater compared to oxygen.
Ans: The solubility rate of CO2 is 22-25 times more than oxygen.
Q5: Write the various modes of transportation of carbon dioxide in the blood.
Ans: Carbon dioxide is transported within the bloodstream in three different forms:
- In its dissolved state: Under typical pressure and temperature conditions, approximately 7% of carbon dioxide is transported in the blood through physical dissolution.
- As carbamino compounds: Carbon dioxide directly binds with hemoglobin (Hb) to create an unstable compound known as carbamino compounds.
- As bicarbonate ions: A significant portion of carbon dioxide is transported in the form of bicarbonate ions.
Long Answer Type Questions
Q1: State the differences between the following:
(a) Expiratory and inspiratory reserve volume
(b) Total lung capacity and vital capacity
(c) Occupational respiratory disorder and Emphysema
Ans: (a) Inspiratory reserve volume (IRV) vs. Expiratory reserve volume (ERV):
- Inspiratory reserve volume refers to the additional amount of air that can be forcefully inhaled by a person, typically ranging between 2500ml to 3000ml.
- Expiratory reserve volume, on the other hand, is the extra volume of air that can be forcefully exhaled through a vigorous expiration and usually falls within the range of 1000ml to 110ml.
(b) Vital Capacity vs. Total lung capacity:
- Vital capacity represents the maximum volume of air a person can inhale after a forced exhalation.
- Total lung capacity, conversely, refers to the overall volume of air that the lungs can hold after a forced inhalation.
(c) Emphysema vs. Occupational Respiratory Disorder:
- Emphysema is a chronic respiratory ailment characterized by damage to alveolar cells, leading to a reduced respiratory surface.
- Occupational respiratory disorders are caused by prolonged exposure to dust generated during activities like rock breaking or stone grinding. This exposure triggers inflammation, resulting in fibrosis and lung damage.
Q2: Explain the transport of O2 and CO2 between alveoli and tissue with a diagram.
Ans: Exchange of gases between the alveoli and tissues occurs primarily in the alveoli. This gas exchange process relies on simple diffusion and is influenced by several factors:
- Partial pressure gradient of gases across alveoli and tissues.
- Solubility of gases.
- The presence of a diffusion membrane.
The diffusion of oxygen (O2) across the alveoli takes place because the partial pressure of O2 in the alveoli is higher (about 104 mmHg) compared to the deoxygenated blood (approximately 40 mmHg). Consequently, O2 diffuses from the alveoli into the bloodstream through the diffusion membrane.
The transport of O2 to various parts of the body occurs through blood circulation and can be divided into two main methods:
- Transport via Red Blood Cells (RBCs) in the form of oxyhemoglobin, which accounts for approximately 97% of transported O2.
- Transport via plasma in a dissolved state, where the remaining 3% of oxygen-rich blood travels from the lungs to the left atrium through the pulmonary veins. From there, it is carried by the left ventricle through the systemic arteries to reach the body tissues.
In the tissues, O2 diffuses across the membranes because the partial pressure of O2 is higher in oxygenated blood (around 95 mmHg) than in the tissues (approximately 40 mmHg). Consequently, O2 moves from the blood into the tissues through diffusion.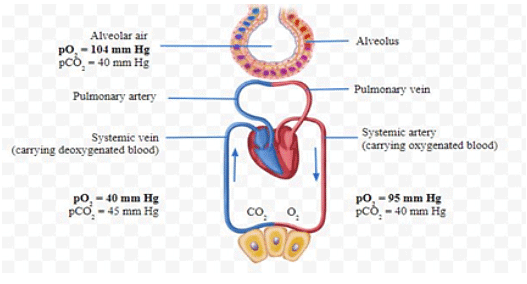
Q3: Describe the role of the neural system in controlling respiration.
Ans: The neural system plays a crucial role in regulating and adjusting the respiratory rhythm based on the body's needs. This regulation is overseen by the respiratory rhythm center located in the brain. Additionally, the pneumotaxic center, situated in the brain's pons region, helps modulate the functions of the respiratory rhythm center. Signals from this center can shorten the duration of inhalation, thus influencing the respiratory rate.
There is also a chemosensitive area adjacent to the rhythm center that is highly sensitive to hydrogen ions and carbon dioxide (CO2). When the levels of these substances increase, they activate this chemosensitive area, which then sends signals to the rhythm center. These signals prompt necessary adjustments in the respiratory process to eliminate excess hydrogen ions and CO2.
Changes in the levels of CO2 and hydrogen ions are detected by receptors connected to the aortic arch and carotid artery. These receptors send signals to the rhythm center, triggering corrective actions to maintain proper respiratory function.
Q4: What happens to the respiratory process in someone going uphill?
Ans: When a person ascends uphill, the elevation gradually rises, leading to a decrease in atmospheric oxygen levels. Consequently, as the individual climbs higher, each breath they take contains less oxygen. This uphill journey results in a reduction in the oxygen content within the bloodstream. In response to this decline in blood oxygen levels, the respiratory rate of the person increases. At the same time, the heart rate also elevates to enhance the delivery of oxygen to the blood, ensuring that the body receives an adequate oxygen supply despite the lower atmospheric oxygen concentration.
Q5: Write a note on the mechanism of breathing
Ans: (a) Inhalation: The process of inhalation is initiated by the contraction of the diaphragm, which elevates the volume of the thoracic chamber along the front-to-back axis. Simultaneously, the intercostal muscles contract, leading to an outward movement of the sternum and ribs, further expanding the thoracic chamber in the top-to-bottom direction. This expansion in thoracic volume results in a corresponding increase in pulmonary volume. As a consequence, the intra-pulmonary pressure drops below atmospheric pressure, facilitating inhalation.
(b) Exhalation: Exhalation occurs as the intercostal muscles and diaphragm return to their original positions, reducing the thoracic volume and, subsequently, the pulmonary volume. The expulsion of air takes place when the intra-pulmonary pressure rises slightly above atmospheric pressure, prompting the process of exhalation.
Q6: What are the major transport mechanisms for CO2? Explain.
Ans: Carbon dioxide is released by actively functioning tissues into the bloodstream. On average, approximately 3.7ml of carbon dioxide is absorbed by every 100ml of blood from these tissues.
Carbon dioxide in the blood is carried in three different forms:
- Dissolved carbon dioxide: About 5-10% of the total volume of carbon dioxide in the blood is dissolved directly in the plasma. It is transported as a simple physical solution.
- Bicarbonate ion: In tissues, where catabolism leads to a high partial pressure of carbon dioxide, carbon dioxide diffuses into the blood and combines with water to form carbonic acid. This reaction is facilitated by the enzyme carbonic anhydrase. Carbonic acid then dissociates into hydrogen ions (H+) and bicarbonate ions (HCO3-). Some of the bicarbonate ions are required to maintain the pH of the blood, while the remaining are taken up by plasma.
- Carbamino-hemoglobin: In tissues where the partial pressure of oxygen is lower and the partial pressure of carbon dioxide is higher, carbon dioxide loosely binds to the globin part of deoxygenated hemoglobin, forming carbamino-hemoglobin. When the partial pressure of oxygen is higher and the partial pressure of carbon dioxide is lower, such as in the alveoli, carbon dioxide dissociates from carbamino-hemoglobin and is released into the airspaces of the lungs.
In summary, carbon dioxide is transported in the blood in these three forms to efficiently regulate its levels and maintain proper pH balance in the body.
Q7: Define vital capacity. What is its significance?
Ans: Vital capacity refers to the maximum volume of air a person can exhale after taking a deep breath or maximum inspiration. In the human body, it typically ranges from 3.5 to 4.5 liters. This capacity allows for the intake of a maximum amount of fresh air and the expulsion of stale or foul air in a single breath. Consequently, it enhances the exchange of gases between different tissues in the body, resulting in an increased availability of energy for various bodily functions.




















