Short & Long Question Answers with Solution: Excretory Products and their Elimination - NEET PDF Download
Short Answer Type Questions
Q1: Why is the hemodialysis unit called an artificial kidney? Explain.
Ans: It serves as an artificial kidney by removing urea from the blood of patients who have kidney failure. The process involves taking blood from an artery, adding heparin to it, and then pumping it into a dialyzing unit. This unit contains a coiled cellophane tube surrounded by a dialyzing fluid that mimics the composition of plasma but lacks nitrogenous waste. The cellophane membrane of the tube is permeable, allowing molecules to pass through based on their concentration gradient. Since the dialyzing fluid does not contain nitrogenous wastes, these wastes can freely move out of the blood. After the blood is cleansed, it is returned to the body through a vein, with anti-heparin supplementation.
Q2: Why is urine yellow in colour?
Ans: The yellow color of urine is a result of the pigment urochrome, which is formed through the breakdown of hemoglobin.
Q3: What is the remedial measure advised for the correction of acute renal failure? Explain briefly.
Ans: Kidney transplantation is the most effective approach for treating acute renal failure. In this procedure, a functional kidney is transplanted from a preferably closely related donor to minimize the risk of rejection by the recipient's immune system.
Q4: What is the composition of urine?
Ans: Urine is primarily composed of 95% water, 2% salt, 2.6% urea, 0.3% uric acid, and small traces of substances such as ammonia, creatinine, and others.
Q5: Explain why the composition of glomerular filtrate is not the same as urine.
Ans: When comparing the volume of the initial filtrate, which is approximately 180 liters per day, to the volume of urine ultimately formed, which is about 1.5 liters per day, it becomes evident that approximately 99% of the filtrate needs to be reabsorbed by the renal tubules. This process is known as reabsorption. Certain substances, such as amino acids, sodium ions (Na+), and glucose, are actively reabsorbed from the filtrate and, as a result, are not typically found in the urine.
Q6: What are the functions of the kidney?
Ans: The functions of the kidney are:
- Removal of metabolic waste from the body.
- Maintenance of water and electrolyte balance.
- Hormonal secretory function like renin secretion.
- Regulation of arterial pressure.
Q7: Give reason why aquatic animals ate mostly ammonotelic in nature whereas terrestrial forms are not.
Ans: To efficiently eliminate ammonia, which is highly toxic, terrestrial organisms have evolved to produce less toxic nitrogenous waste products like uric acid and urea. Ureotelic animals, for example, have developed a mechanism in which ammonia generated during metabolic processes is transformed into urea within their liver. This urea is then released into the bloodstream, filtered by the kidneys, and ultimately excreted from the body. This adaptation helps these animals conserve water while effectively disposing of nitrogenous waste.
Q8: Explain podocytes.
Ans: These cells make up the lining of Bowman's capsule. The inner wall of the glomerulus contains unique cells known as podocytes, which are less flattened in shape. Between these podocytes, there are extremely small gaps referred to as filtration slits or slit pores.
Q9: Describe the role of Renin-Angiotensin in the management of Kidney function.
Ans: The Juxta-Glomerular Apparatus (JGA) becomes active when there is a decrease in blood flow within the glomerulus. When activated, it releases renin. Renin, in the blood, converts angiotensinogen into angiotensin I and subsequently into angiotensin II. Angiotensin II acts as a vasoconstrictor, leading to an elevation in blood pressure within the glomerulus and an increase in the Glomerular Filtration Rate (GFR). Additionally, angiotensin II stimulates the adrenal cortex to produce aldosterone. Aldosterone, in turn, promotes the reabsorption of water and sodium ions from the distal parts of the tubule. This further enhances the GFR and blood pressure. This regulatory process is known as the Renin Angiotensin Aldosterone System (RAAS).
Q10: Identify the glands that perform the excretory functions in prawns.
Ans: Prawns rely on green glands for their excretory process, which are alternatively known as antennal glands due to their location at the antenna's base. This excretory system consists of coelomic structures, a labyrinth, nephridial duct, bladder, and nephridiopore.
Q11: What is meant by osmoregulation?
Ans: Osmoregulation involves the adjustment of body fluid concentration to match the external environment. The kidneys are responsible for maintaining the internal environment. Nephrons, by regulating urine production from blood, handle both excretion and osmoregulation. Osmoregulation is influenced by two types of nephrons and the length of Henle's loop. Cortical nephrons are active when there is a sufficient to excess water supply, while juxtamedullary nephrons come into play when water supply is limited.
Q12: How have terrestrial organisms adapted themselves for the conservation of water?
Ans: Adaptation to terrestrial environments involves the production of nitrogenous wastes that are less toxic, such as urea and uric acid, in order to conserve water. Ammonia, which is excreted by aquatic animals, requires a significant amount of water for dissolution. However, for terrestrial animals, this large water requirement is unnecessary. They excrete waste products with less water consumption and are classified as either ureotelic or uricotelic.
Q13: Why is a haemodialysis unit called an artificial kidney?
Ans: Haemodialysis is a process that eliminates urea and creatinine from the blood. During haemodialysis, an individual's blood is filtered through a specialized unit where dialysing fluid, with a composition similar to plasma but lacking nitrogenous waste, is used.
Q14: Differentiate Glycosuria from ketonuria.
Ans:
- Glycosuria refers to the detection of glucose in the urine and is observed in individuals with diabetes and Cushing syndrome.
- Ketonuria is the presence of ketone bodies in the urine and is commonly observed in diabetes.
Long Answer Type Questions
Q1: Explain the micturition and disorders of the excretory system.
Ans: During the process of micturition, urine is produced by the nephrons and then stored in the urinary bladder until a signal is sent by the central nervous system (CNS). This signal is initiated when the bladder stretches due to the accumulation of urine, and stretch receptors on the bladder walls send signals to the CNS. To facilitate the smooth contraction of the bladder muscles and simultaneous relaxation of the urethral sphincter, the CNS transmits motor messages. This coordinated action leads to the release of urine, a process known as micturition.
Some disorders related to this process include:
- Kidney malfunction can result in the buildup of urea in the blood, a condition known as uremia, which may eventually lead to kidney failure. To treat this, urea is removed from the blood through procedures like hemodialysis and kidney transplantation.
- Renal calculi, also known as kidney stones, occur when insoluble crystallized salt deposits form within the kidney.
- Inflammation of the kidney's glomeruli is referred to as glomerulonephritis.
Q2: What is the role of tubular secretion in maintaining acid-base and ionic balance in the body fluids?
Ans: Tubular cells are responsible for releasing ammonia, hydrogen ions (H+), and potassium ions (K+) into the filtrate during the process of urine formation. This tubular secretion is essential for regulating the balance of ions and the body's acid-base equilibrium in bodily fluids, playing a crucial role in the formation of urine. The proximal convoluted tubule (PCT) contributes to this process by selectively secreting ammonia, hydrogen ions, and potassium ions into the filtrate. Additionally, the distal convoluted tubule (DCT) also has the capability to selectively secrete potassium ions, hydrogen ions, and ammonia, which helps maintain the proper sodium-potassium balance and pH levels in the blood. Another structure involved in preserving the blood's pH and ionic balance by selectively secreting hydrogen ions (H+) and potassium ions (K+) is the collecting duct.
Q3: Explain the types of nitrogen excretion.
Ans: There are three primary methods of nitrogen excretion in organisms: ammonotelism, ureotelism, and uricotelism.
- Ammonotelism involves the direct excretion of ammonia, which diffuses across the body's surface. Organisms employing this method need access to ample water due to the high toxicity of ammonia. Notably, the kidneys are not involved in this process.
- Ureotelism, on the other hand, involves the conversion of ammonia into urea by the liver. The kidneys then excrete this urea. Urea is less toxic than ammonia and has lower solubility in water. A small amount of urea is retained to help maintain osmotic balance.
- Uricotelism is characterized by the excretion of uric acid in the form of solid pellets. This method results in minimal water loss, as uric acid is insoluble in water and relatively non-toxic.
Q4: Explain why in the loop of Henle, the glomerular filtrate gets concentrated in the descending limbs and diluted in the ascending limbs.
Ans: The thin wall of Henle's loop allows water to pass through but not solutes. As the isotonic tubular fluid moves down the loop, it gradually loses water through osmosis, driven by the higher osmolarity in the medullary interstitium. Consequently, the filtrate becomes more concentrated (hypertonic) compared to the blood plasma.
In contrast, the thick ascending limb of the loop of Henle is permeable to ions like K+, Na+, Cl-, partially permeable to urea, but impermeable to water. In this section, substances like calcium (Ca), magnesium (Mg), chloride (Cl), potassium (K), and sodium (Na) are reabsorbed from the filtrate, causing it to become less concentrated (hypotonic) compared to the blood plasma.
Q5: What is the role played by Renin-Angiotensin in the regulation of kidney function?
Ans: The renin-angiotensin system serves several crucial roles:
- Juxtaglomerular cells in the walls of the afferent arteriole release renin when blood pressure is low.
- Renin, an enzyme, converts angiotensinogen (a plasma protein produced by the liver) into Angiotensin-I and subsequently Angiotensin-II.
- Angiotensin-II is a potent vasoconstrictor, which means it narrows blood vessels, leading to an increase in blood pressure.
- Angiotensin-II also boosts the Glomerular Filtration Rate (GFR), enhancing the filtration of blood in the kidneys.
- This system triggers the adrenal cortex to release aldosterone.
- Aldosterone, in turn, promotes the reabsorption of sodium and water in the distal parts of the tubule, further elevating blood pressure and GFR.
- Overall, this process represents autoregulation of the Glomerular Filtration Rate to help maintain blood pressure and filtration efficiency in the kidneys.
Q6: Define the following term with examples?
(i) Ammonotelic organisms.
(ii) Uricotelic organisms.
(iii) Ureotelic organisms.
Ans:
(i) Ammonotelic organisms: These are living beings that eliminate nitrogenous waste in the ammonia form. Examples of ammonotelic organisms encompass bony fishes, sepia, and octopus.
(ii) Uricotelic organisms: These are creatures that excrete nitrogenous waste in the uric acid form. Uricotelic organisms encompass birds, as well as other species such as lizards and insects.
(iii) Ureotelic organisms: These are organisms that expel nitrogenous waste in the urea form. Ureotelic organisms include cartilaginous fish, certain bony fishes, adult amphibians, and mammals, including humans.
Q7: Describe the role of lungs, liver and skin in excretion.
Ans: Respiration produces waste products in the form of water and carbon dioxide, which are expelled from the body through the lungs. Human lungs discharge approximately 18 liters of carbon dioxide per hour and around 400 milliliters of water daily.
In the liver, decomposed hemoglobin is transformed into bile pigments, specifically bilirubin and biliverdin, which are excreted through bile. Bilirubin undergoes further breakdown into stercobilin and urobilin. Bilirubin is a harmful substance, and its buildup can lead to jaundice. These pigments are excreted in feces. Additionally, the liver plays a role in eliminating cholesterol, steroid hormones, vitamins, and certain drugs through bile. Unwanted amino acids in the liver produce ammonia, which combines with carbon dioxide to form urea, a process known as the urea cycle or Ornithine cycle. The kidneys are responsible for excreting this urea.
The skin features sweat and sebaceous glands, with sweat glands releasing sweat and sebaceous glands producing sebum.
Q8: Give a brief account of the countercurrent mechanism.
Ans: The countercurrent mechanism is a specialized process that enhances water absorption from the glomerular filtrate, aiding in water conservation and resulting in more concentrated urine.
This mechanism involves several key components:
- The countercurrent mechanism operates in both Henle's loop and the vasa recta, where filtrate flows in opposite directions along the limbs of the Loop of Henle and in the vasa recta.
- The renal medulla's interstitium has a hypertonic osmolarity gradient, increasing from the renal cortex to the tip of the medullary papillae.
- The high osmolarity is maintained through active transport of sodium, potassium, and chloride ions from the thick ascending limb of Henle into the interstitium.
- The hyperosmolarity at the papillary tip can reach levels of 1200-1450 mOsmol/L, indicating the accumulation of solutes in water-rich surroundings.
- This gradient is upheld by the countercurrent mechanism and the close proximity between Henle's loop and the vasa recta, ensuring a balanced inflow and outflow of solutes and water.
- The movement of sodium chloride (NaCl) and urea plays a pivotal role in maintaining this gradient, facilitated by Henle's loop and the vasa recta. The vasa recta, a capillary network encircling the Loop of Henle, acts as a countercurrent exchanger.
- The ascending limb of Henle's loop is impermeable to water, while the descending limb is highly permeable, creating a gradient.
- The countercurrent mechanism consists of two aspects: countercurrent multiplication by Henle's Loop and countercurrent exchange by the vasa recta.
- Countercurrent multiplication involves the repeated reabsorption of sodium from the thick ascending limb of Henle's loop and a continuous inflow of new sodium chloride from the proximal convoluted tubule (PCT). NaCl is transported through the ascending limb and enters the descending limb of the vasa recta. NaCl returns to the medullary interstitium via the ascending part of the vasa recta, while water diffuses into the blood of the ascending vasa recta, eventually entering the general circulation.
- The thin ascending limb of Henle's loop and the collecting duct in the deeper regions have permeability to urea. Urea, after diffusing out of the collecting ducts, enters the thin ascending limb and is recycled and trapped in the medullary interstitium by the collecting tubule.
- Through this intricate mechanism, a concentration gradient is maintained in the medullary interstitium, resulting in urine that is approximately four times more concentrated than the initial filtrate.
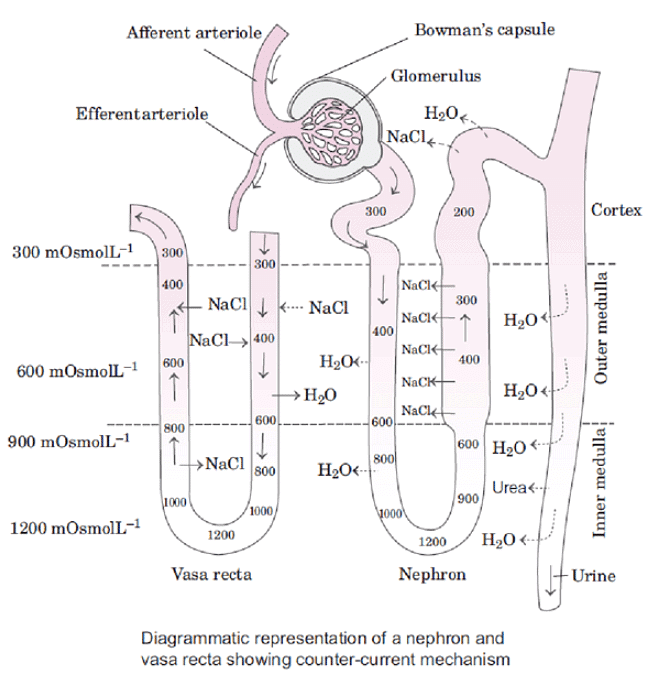
In summary, the countercurrent mechanism is a vital process that enables the kidneys to conserve water and produce concentrated urine through the interaction of Henle's loop, vasa recta, and the selective transport of solutes like NaCl and urea.
Q9: What are the main processes of urine formation?
Ans: The process by which urine is formed is known as uropoiesis, which consists of three main steps:
- Glomerular filtration: This initial step involves the filtration of blood by the glomerulus. It is referred to as "glomerular filtration" because the blood flows into the glomerular capillaries under high pressure, and substances are filtered across the thin capillary walls. The resulting glomerular filtrate is essentially plasma minus proteins and contains various components such as glucose, amino acids, water, urea, uric acid, hippuric acid, salts, vitamins, creatinine, bicarbonates, and phosphates.
- Selective reabsorption: During this phase, the filtrate is further processed to form urine. This process is known as "reabsorption." The proximal convoluted tubule (PCT) plays a significant role in reabsorption, where the majority of substances from the glomerular filtrate are reabsorbed. Glucose and amino acids are completely absorbed through active transport, not normally appearing in urine. Active transport involves energy in the form of ATP and occurs against concentration gradients. Urea and uric acid are not fully reabsorbed and are typically present in urine under normal conditions. Creatinine and sulfates, however, are not reabsorbed at all. Chloride absorption is passive. The counter-current mechanism in Henle's Loop concentrates the fluid further. Sodium is absorbed in the ascending limb only. Water absorption in the distal convoluted tubule (DCT), collecting tubule, and collecting duct is dependent on antidiuretic hormone (ADH).
- Approximately 60-70% of water is reabsorbed in the PCT.
- About 15% of water is reabsorbed in Henle's loop.
- Roughly 4-5% of water is reabsorbed in the DCT. - Tubular secretion: This final step is crucial for urine formation. It involves the removal of certain substances from the blood that were not initially filtered by the glomerular capillaries. Tubular secretion helps maintain ionic and acid-base balance by eliminating ions and other potentially harmful molecules that could accumulate at high levels. The proximal convoluted tubule (PCT) and distal convoluted tubule (DCT) contribute significantly to tubular secretion. This process includes the addition of creatinine, ammonia, hydrogen ions, potassium ions, and uric acid into the glomerular filtrate.
FAQs on Short & Long Question Answers with Solution: Excretory Products and their Elimination - NEET
| 1. What are the main excretory products in humans? |  |
| 2. How does the human excretory system function? |  |
| 3. What role do kidneys play in the elimination of excretory products? |  |
| 4. What are the common disorders related to the excretory system? |  |
| 5. How does the process of osmoregulation relate to excretion? |  |



















