Teratogenesis - Teratogenic Agents | Zoology Optional Notes for UPSC PDF Download
Teratogenesis: Teratogenic Agents and Effects on Embryonic Development
Teratogenesis: Teratogenesis, or teratogenicity, refers to the process through which congenital birth defects occur, involving various factors such as biological infections, physical agents, pharmacological drugs, industrial pollutants, maternal health problems, and maternal tipsiness. Teratology is the scientific study that investigates congenital malformations and their causes.
Teratogenic Agents: Agents responsible for causing congenital malformations are termed teratogenic agents. They can be categorized into several groups:
Infectious Agents:
- Examples include viral infections (rubella, herpes simplex, cytomegalovirus), spirochetal infections (syphilis), and protozoal infestations (toxoplasmosis).
- Maternal exposure to influenza during the first trimester is associated with an increased risk of various non-chromosomal congenital anomalies.
Physical Agents:
- Radiation is teratogenic, and its effects are cumulative, with the first trimester being particularly sensitive.
Chemical Agents:
- Medications, such as antiepileptic drugs, can have teratogenic effects, and their use during pregnancy requires careful consideration.
- Retinoic acid (vitamin A metabolite) in excess can result in malformations, and drugs like isotretinoin used for severe acne can cause fetal abnormalities.
- Mefloquine, an antimalarial drug, and miltefosine, used for visceral leishmaniasis, also pose teratogenic risks.
Environmental Pollutants:
- Toluene, an organic solvent, and cadmium, a heavy metal pollutant, can lead to mental health retardation and growth impairment in the fetus.
Tipsiness of Mother:
- Alcohol consumption during pregnancy is teratogenic and can cause fetal alcohol spectrum disorders (FASDs).
- Nicotine consumption is associated with an increased incidence of attention hyperactivity disorder (ADHD), and smoking increases the risk of sudden infant death syndrome (SIDS).
Maternal Health Problems:
- Diabetes mellitus in mothers, both pre-existing and gestational, is associated with an increased risk of congenital anomalies.
- Multiple sclerosis (MS) and rheumatoid arthritis (RA) in pregnant mothers require careful consideration of therapy due to potential teratogenic effects.
Understanding teratogenesis is crucial for identifying and mitigating factors that contribute to congenital malformations during embryonic development. It emphasizes the importance of careful management of maternal health, avoidance of teratogenic agents, and informed decision-making regarding medications during pregnancy to ensure optimal outcomes for both mother and fetus.
Amniocentesis: Prenatal Genetic Testing Procedure
Definition: Amniocentesis, also known as the amniotic fluid test, is a medical procedure used for prenatal genetic testing to assess chromosomal abnormalities, the presence or absence of certain genes, enzymes, fetal infections, and determine the sex of the fetus. It involves the extraction of a sample of amniotic fluid from a pregnant woman.
Why is Amniocentesis Performed?
Amniocentesis is typically offered to women with a significant risk for genetic diseases, including those who:
- Have abnormal ultrasound or lab screens
- Have a family history of certain birth defects
- Previously had a child or pregnancy with a birth defect
- Had an abnormal genetic test result in the current pregnancy
Amniocentesis is not exhaustive in detecting all birth defects, but it can identify conditions such as Down syndrome, sickle cell disease, cystic fibrosis, muscular dystrophy, and Tay-Sachs disease if there is a significant genetic risk.
Procedure:
Preparation: Amniocentesis is performed as an outpatient procedure. Ultrasonography guides the positioning and movements of the fetus, the location of the placenta, and characteristics of amniotic fluid.
Needle Insertion: With ultrasound guidance, a long, sterile needle is inserted through the abdominal wall, muscle, and uterus into the amniotic sac.
Fluid Extraction: Approximately 20ml of amniotic fluid is extracted, with the first 2ml typically discarded due to maternal blood cell contamination.
Fetal Cell Separation: Fetal cells within the amniotic fluid, including multipotent stem cells, are separated and cultured. Chromosomes are examined for abnormalities.
Sealing and Healing: After the procedure, the puncture site seals, and the amniotic sac replenishes the fluid over the next 24-48 hours.
Medical Uses:
Genetic Diagnosis: Amniocentesis aids in the early diagnosis of chromosomal abnormalities, including Down syndrome, Patau syndrome, Edwards' syndrome, sex chromosome aneuploidies, and neural tube defects.
Infection Detection: It can detect infections by assessing glucose levels, Gram stain for bacteria, or abnormal WBC differential count.
Lung Maturity Prediction: Amniocentesis predicts fetal lung maturity, crucial for assessing the risk of infant respiratory distress syndrome.
Decompression of Polyhydramnios: The procedure can relieve polyhydramnios (accumulation of excess amniotic fluid) and diagnose its potential causes.
Rh Incompatibility: Amniocentesis helps diagnose Rh incompatibility, allowing early intervention to prevent complications.
Risks:
- Complications include preterm labor, respiratory distress, chorioamnionitis, fetal trauma, and amniotic fluid embolism.
- Amniotic fluid leakage and bleeding pose risks of spontaneous abortion.
- The procedure is typically performed between the 15th and 20th week of pregnancy to avoid fetal injury.
- "Early amniocentesis" (weeks 11-13) may be considered in certain cases.
- Risks emphasize the importance of careful consideration and informed decision-making.
Additional Note:
- The first amniotic stem cells bank in the US is active in Boston, Massachusetts.
Amniocentesis is a valuable tool in prenatal care, providing crucial information about the fetus's health and aiding in informed decision-making for expectant parents.
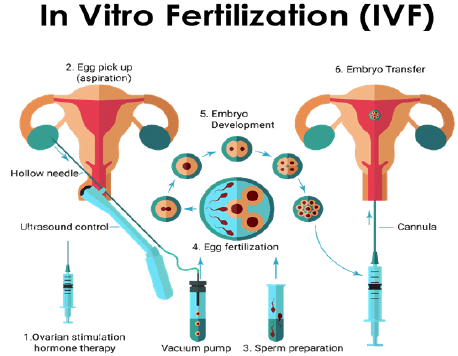
In Vitro Fertilization (IVF): A Comprehensive Overview
Definition: In vitro fertilization (IVF) is a fertility treatment that involves combining an egg with sperm outside the body, in vitro ("in glass"). The process includes monitoring and stimulating a woman's ovulatory process, retrieving eggs, fertilizing them with sperm in a laboratory setting, and then implanting the resulting embryo in the uterus.
Purposes of IVF:
IVF is employed as a treatment for infertility or genetic problems. It is considered for the following conditions:
- Fallopian Tube Damage or Blockage: Difficulty in fertilization due to impaired egg travel or embryo transport.
- Ovulation Disorders: Infrequent or absent ovulation leading to reduced egg availability for fertilization.
- Endometriosis: Abnormal growth of uterine tissue outside the uterus, affecting reproductive organs' functionality.
- Uterine Fibroids: Non-cancerous tumors in the uterus wall that may hinder embryo implantation.
- Previous Tubal Sterilization or Removal: As an alternative to tubal ligation reversal for women seeking conception.
- Impaired Sperm Production or Function: Conditions such as weak sperm movement or abnormal sperm morphology.
- Genetic Disorders: For couples at risk of passing on genetic disorders, with pre-implantation genetic testing conducted during IVF.
- Fertility Preservation: Preserving fertility before cancer treatments that may harm reproductive capabilities.
- Women without a Functional Uterus: Using a gestational carrier for women unable to carry a pregnancy due to health reasons.
Steps Involved in IVF:
Ovulation Induction:
- Medications: Stimulation with hormones (FSH, LH) to produce multiple eggs.
- Monitoring: Vaginal ultrasound and blood tests to track follicle development.
- HCG Administration: To mature eggs before retrieval.
- Uterine Lining Preparation: Progesterone supplements for a receptive uterine lining.
Egg Retrieval:
- Procedure: Done 34-36 hours post-HCG injection.
- Sedation: Patient sedated for comfort.
- Technique: Trans-vaginal ultrasound aspiration to retrieve eggs.
- Processing: Extracted eggs placed in a culture medium for incubation.
Sperm Retrieval:
- Sample Collection: Partner provides a semen sample.
- Processing: Sperms separated from semen fluid in the lab.
- Alternatives: Testicular aspiration or donor sperm may be used.
Fertilization:
- Methods: Conventional insemination or Intracytoplasmic Sperm Injection (ICSI).
- Conventional: Healthy sperm and mature eggs incubated together.
- ICSI: Single healthy sperm injected directly into each mature egg.
Embryo Transfer:
- Timing: Usually 2-5 days post-egg retrieval.
- Procedure: Embryos transferred into the uterus through a catheter.
- Sedation: Mild sedative for the patient.
- Outcome: Successful implantation may lead to pregnancy.
Result and Follow-up:
- Pregnancy Test: Blood test after 12 days to detect pregnancy.
- Pregnancy Outcome: If successful, referral for prenatal care; if not, potential adjustments for subsequent IVF cycles.
Risks Associated with IVF:
- Multiple Births: Increased risk if multiple embryos are transferred.
- Premature Delivery and Low Birth Weight: Slight elevation in the risk.
- Ovarian Hyperstimulation Syndrome (OHSS): Swelling and pain in ovaries due to fertility drugs.
- Miscarriage: Comparable rates to natural conception, increasing with maternal age.
- Egg-Retrieval Complications: Bleeding, infection, or organ damage.
- Ectopic Pregnancy: Fertilized egg implants outside the uterus, typically in the fallopian tube.
- Birth Defects: Association with maternal age and certain imprinting disorders.
- Spread of Infectious Diseases: Potential transmission through donor sperm.
- Anaesthesia Risks: Associated with sedation during the procedure.
IVF is a comprehensive fertility treatment offering hope to individuals facing various reproductive challenges, with careful consideration of associated risks and potential outcomes.
Stem Cells: A Comprehensive Overview
Definition: Stem cells are undifferentiated cells present in the human body, capable of generating specialized cells through division. Under specific conditions, they can produce either identical stem cells (self-renewal) or differentiate into functional cells such as blood cells or brain cells.
Sources of Stem Cells:Embryonic Stem Cells (ESCs):
- Derived from 3 to 5-day-old embryos.
- Highly versatile, used for regenerative and cell replacement therapies.
Adult Stem Cells:
- Found in small numbers in various adult tissues (e.g., bone marrow, fat).
- Limited ability compared to embryonic stem cells.
Adult Cells Altered to Resemble ESCs:
- Genetic reprogramming transforms regular adult cells into stem cells.
- Altered cells exhibit properties similar to embryonic stem cells.
Perinatal Stem Cells:
- Discovered in amniotic fluid and umbilical cord blood.
- Exhibit the ability to differentiate into specialized cells.
Embryonic Stem Cells (ESCs):
- Isolation: Derived from the inner cell mass of a blastocyst, a pre-implantation embryo.
- Stage: Blastocyst stage is reached 4-5 days post-fertilization.
- Ethical Considerations: Isolating the inner cell mass involves destroying the blastocyst, raising ethical concerns about pre-implantation embryo moral considerations.
Pluripotent:
- ESCs can differentiate into any embryonic cell type.
- Differentiation potential includes ectoderm, endoderm, and mesoderm, giving rise to over 220 cell types in the human body.
Self-Renewal and Structure Repair:
- ESCs can self-renew indefinitely under defined conditions.
- Conditions supporting self-renewal prevent clumping and maintain an unspecialized state.
Regenerative Medicine:
- ESC therapies proposed for tissue replacement and regenerative medicine.
- Potential treatments for spinal cord injuries, macular degeneration, diabetes, neurodegenerative disorders, and more.
Cell Replacement Therapies (CRTs):
- ESCs can differentiate into various cell types.
- Current research includes cardiomyocytes, neurons, hepatocytes, bone marrow cells, islet cells, and endothelial cells.
Clinical Potential:
- Differentiation into natural killer cells and bone tissue.
- Exploration for Parkinson's disease treatment through dopamine-producing cells.
- Research on ESCs for diabetes treatment, generating insulin-producing cells.
Drug Discovery:
- ESCs contribute to drug discovery, acting as an alternative to organ transplants.
- Used in toxicology and as cellular screens for developing small molecule drugs.
Stem cells, particularly embryonic stem cells, hold significant promise for medical advancements, from regenerative therapies to drug development. However, ethical considerations and ongoing research challenges need to be addressed for their responsible and effective utilization.
|
181 videos|351 docs
|















