Acid peptic disease | Medical Science Optional Notes for UPSC PDF Download
Risk factors Acid peptic disease
- Acid peptic disease or Peptic Ulcer Disease (PUD) encompasses both gastric and duodenal ulcers (DUs).
- Common ulcer locations include the first part of the duodenum and the lesser curve of the stomach. However, ulcers can also occur on the stoma after gastric surgery, the esophagus, and even in a Meckel's diverticulum containing ectopic gastric epithelium.
- The most common risk factors for PUD are H. pylori infection and the use of NSAIDs.
- Additional risk factors comprise:
a. Chronic obstructive lung disease
b. Chronic renal insufficiency
c. Current tobacco use
d. Former tobacco use
e. Older age
f. Three or more doctor visits in a year
g. Coronary heart disease
h. Former alcohol use
i. African-American race
j. Obesity
k. Diabetes
Clinical features-Acid peptic disease
While various textbooks attempt to highlight distinctions in the clinical features of gastric and duodenal ulceration, in-depth analysis has revealed that they cannot be differentiated based on symptoms.
Physical examination is important for discovering evidence of peptic ulcer complications (if any)
Diagnosis-Acid peptic disease
The possible alternative diagnoses include functional dyspepsia, gastrointestinal tumors in the proximal region, gastroesophageal reflux disease, gallbladder-related pain (biliary colic), persistent inflammation of the pancreas (chronic pancreatitis), and Crohn's disease.
For the diagnostic evaluation:
- Gastroduodenoscopy:
- Conduct an endoscopic examination of the stomach and duodenum.
- Obtain multiple biopsy samples for analysis.
- Perform the CLO test to diagnose H. pylori infection.
- Barium studies (double-contrast studies):
- Use radiographic imaging with barium contrast.
- Assist in the diagnosis of H. pylori infection through appropriate diagnostic tests.
- Serum gastrin level assay:
- Measure serum gastrin levels, especially in cases of refractory peptic ulcer disease, to assess for Zollinger-Ellison syndrome.
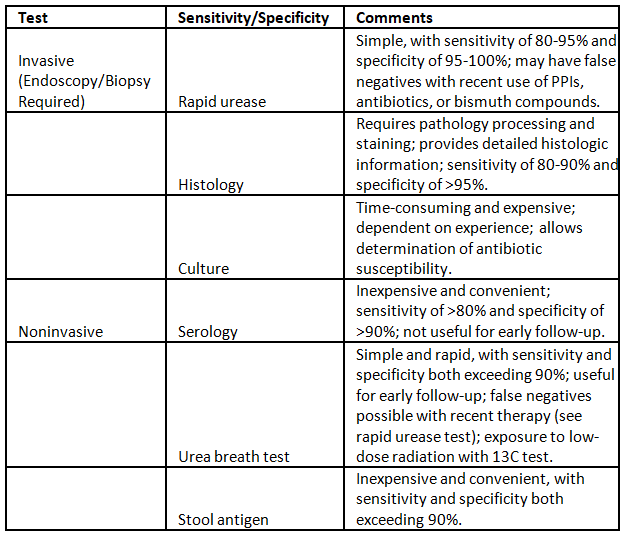
H.Pylori detection
Medical management-Acid peptic disease
 Prolonged acid suppression, particularly with PPIs, is linked to an increased risk of community-acquired pneumonia, as well as both community and hospital-acquired Clostridium difficile-associated disease. Additionally, it is implicated in the onset of deficiencies in iron, vitamin B12, and magnesium.
Prolonged acid suppression, particularly with PPIs, is linked to an increased risk of community-acquired pneumonia, as well as both community and hospital-acquired Clostridium difficile-associated disease. Additionally, it is implicated in the onset of deficiencies in iron, vitamin B12, and magnesium.
H. Pylori eradication therapy
The agents used with the greatest frequency include amoxicillin, metronidazole, tetracycline, clarithromycin, and bismuth compounds.
One FDA approved triple therapy for eradication of H.Pylori is combination of PPI BD+Clarithromycin (500mg BD)+Amoxicillin (1 g BD) or Metronidazole (500 mgTID) for a duration of 14 days
Clarithromycin-based triple therapy should be avoided in settings where H. pylori resistance to this agent exceeds 15%.
Surgical management-Acid peptic disease
- Surgical intervention for peptic ulcer disease (PUD) can be categorized as elective or urgent/emergent, with a significant decline in elective surgeries due to advances in pharmacologic and endoscopic treatments.
- The three main operations for duodenal ulcer management include: a. Vagotomy and drainage: Involves cutting vagal fibers to reduce acid secretion, often combined with pyloroplasty, gastroduodenostomy, or gastrojejunostomy for compensating gastric motility issues. b. Highly selective vagotomy: Targets specific vagal fibers to parietal cells, minimizing gastric dysmotility and eliminating the need for drainage procedures. c. Vagotomy with antrectomy: A procedure with the lowest ulcer recurrence rate (1%) but a higher complication rate, aiming to eliminate gastrin as a stimulant for acid secretion.
- Antrectomy:
- Purpose: Eliminates an additional stimulant of gastric acid secretion, gastrin.
- Two types of reanastomoses after antrectomy:
a. Gastroduodenostomy (Billroth I): Removal of the lower half of the stomach, with the remaining portion anastomosed to the first part of the duodenum.
b. Gastrojejunostomy (Billroth II): Removal of two-thirds of the stomach, closure of the duodenal stump, and anastomosis of the stomach to the jejunum.
- Billroth I vs. Billroth II:
- Billroth I: Involves removing the lower half of the stomach and connecting it to the duodenum.
- Billroth II: Requires removing two-thirds of the stomach, closing the duodenal stump, and anastomosing the stomach to the jejunum.
- The combination of vagotomy (truncal or selective) with antrectomy offers the lowest ulcer recurrence rates (1%) but comes with a higher complication rate.

Complications-Acid peptic disease

Cirrhosis of Liver-Etiology
Cirrhosis is defined as a diffuse process characterized by fibrosis and the conversion of normal liver architecture into structurally abnormal nodules.
Depending on the size of the nodulesCirrhosis may be:

Cirrhosis of Liver-Pathogenesis


Cirrhosis of Liver-Histopathology

Fibrous septa-delicate bands or broad scars around multiple adjacent lobules.
- Parenchymal nodules, encircled by these fibrous bands.
- Regeneration by preexisting long-lived hepatocytes and newly formed hepatocytes from stem cells (canals of hering)
Cirrhosis of liver-Clinical features
- Jaundice results from decreased liver function and elevated bilirubin levels.
- Bleeding tendencies occur due to impaired synthesis of coagulation factors.
- Elevated urea levels lead to increased ammonia, contributing to hepatic encephalopathy.
- Ascites is associated with decreased albumin production.
- Bile acids impairment hinders intestinal absorption of fat-soluble vitamins.
- Inefficient medication metabolism leads to drug accumulation, raising the risk of toxicity.
- Liver disease-related diabetes is linked to heightened insulin resistance.
- Liver's compromised estrogen and androstenedione metabolism contributes to hyperestrogenism, leading to hypogonadism and gynecomastia.
- Limited activation of vitamin D results in secondary hyperparathyroidism.
- Palmar erythema and spider angiomas reflect local vasodilatation, with each angioma being a pulsating, dilated arteriole from which small vessels radiate.
- Parotid gland enlargement is observed as a manifestation of impaired liver function.

Cirrhosis of liver-Diagnosis
- CBP-anemia (either from chronic Gl blood loss, nutritional deficiencies, or hypersplenism related to portal hypertension) and thrombocytopenia.
- Serum total bilirubin can be normal or elevated with advanced disease.
- Prothrombin times are often prolonged and usually do not respond to administration of parenteral vitamin K.
- Serum sodium levels are usually normal unless patients have ascites and then can be depressed, largely due to ingestion of excess free water.
- Serum alanine and aspartate aminotransferases (ALT, AST) are typically elevated, particularly in patients who continue to drink, with AST levels being higher than ALT levels, usually by a 2:1 ratio.
- Liver biopsy can be helpful to confirm a diagnosis, but generally when patients present with alcoholic hepatitis and are still drinking, liver biopsy is withheld until abstinence has been maintained for at least 6 months to determine residual, nonreversible disease.
- Fibroscan is a type of USG elastography and helps to assess early changes of cirrhosis. Elastography is particularly advantageous in this case because when fibrosis is diffuse, a biopsy can easily miss sampling the diseased tissue, which results in a false negative misdiagnosis.
Cirrhosis of liver-Treatment
- Abstaining from alcohol consumption is crucial in the management of alcohol-related issues.
- Medications such as Acamprosate can be employed to diminish alcohol cravings.
- Caution is advised against the use of Acetaminophen in this context.
- Emphasizing good nutrition and maintaining long-term medical supervision are essential components of the treatment plan.
- Proper management of associated complications is imperative for comprehensive care.
Role of Glucocorticoids:
- Glucocorticoids may be utilized in severe alcoholic hepatitis cases without infection.
- Treatment eligibility is determined by a discriminant function (DF) value exceeding 32.
- The DF is calculated by adding the serum total bilirubin to four times the difference in prothrombin time compared to control (in seconds).
- Improved 28-day survival is observed in patients with a DF value exceeding 32 when treated with glucocorticoids.
Cirrhosis of liver-Complications
- Spontaneous bacterial peritonitis is a potential complication.
- Portal hypertension is a condition that may arise.
- Hepatic encephalopathy is a manifestation of impaired liver function.
- Hepatorenal syndrome denotes renal dysfunction associated with liver issues.
- Portal vein thrombosis is the formation of clots in the portal vein.
- Pulmonary complications linked to portal hypertension can occur.
- Hepatopulmonary syndrome refers to pulmonary abnormalities associated with liver disease.
- Portopulmonary hypertension is a specific form of pulmonary hypertension related to portal hypertension.
- Tumors, including hepatocellular carcinoma (HCC), can develop as a late complication of liver disease.
Portal Hypertension-Etiology
Portal hypertension is present if the portal venous pressure is > 6 mm Hg (normal value: 1-5 mm Hg). Portal venous pressure > 10 mm Hg is clinically significant and > 12 mm Hg is associated with complications.
Causes of portal hypertension can be classified as follows:
- Pre-hepatic:
- Portal vein thrombosis
- Splenic vein thrombosis
- Hepatosplenic schistosomiasis
- Intrahepatic:
- Cirrhosis, including fibrous proliferation
- Massive hepatic metastases
- Post-hepatic:
- Budd-Chiari syndrome
- Right-sided heart failure
- Constrictive pericarditis
Portal Hypertension-Presentation
- Blood flow through portosystemic anastomoses occurs via paraumbilical veins and epigastric veins, leading to the development of Caput medusae.
- Hemorrhoidal or anorectal varices may form through blood flow in rectal veins.
- Esophageal varices and (epi)gastric varices may develop due to blood flow through veins of the gastric fundus and lower esophagus, posing a risk of life-threatening esophageal variceal bleeding.
- Congestive splenomegaly manifests, followed by signs of hypersplenism.
- Upper gastrointestinal bleeding may occur from portal hypertensive gastropathy, gastrointestinal ulcers, or diffuse lower gastrointestinal bleeding.
- The presence of transudative ascites is observed in this context.

Portal Hypertension-Diagnosis
- Diagnosis of portal hypertension in a patient with a known risk factor (e.g., cirrhosis) can be established based on clinical manifestations such as ascites.
- Duplex ultrasonography may reveal specific findings like the visualization of cavernous transformation, indicating chronic portal vein thrombosis.
- An unspecific finding on ultrasound is the dilation of the portal vein beyond 13 mm.
- Indirect indications of portal hypertension include the visualization of blood flow through portosystemic anastomoses, splenomegaly, and the presence of ascites using duplex ultrasonography.
- Abdominal CT scans can visually confirm portal vein thrombosis.
- Esophagogastroduodenoscopy (EGD) is employed for the assessment and, if necessary, treatment of esophageal varices.
Portal Hypertension-Management
The three primary complications of portal hypertension are gastroesophageal varices with hemorrhage, ascites, and hypersplenism
- Diagnosis of portal hypertension in a patient with a known risk factor (e.g., cirrhosis) can be established based on clinical manifestations such as ascites.
- Duplex ultrasonography may reveal specific findings like the visualization of cavernous transformation, indicating chronic portal vein thrombosis.
- An unspecific finding on ultrasound is the dilation of the portal vein beyond 13 mm.
- Indirect indications of portal hypertension include the visualization of blood flow through portosystemic anastomoses, splenomegaly, and the presence of ascites using duplex ultrasonography.
- Abdominal CT scans can visually confirm portal vein thrombosis.
- Esophagogastroduodenoscopy (EGD) is employed for the assessment and, if necessary, treatment of esophageal varices.
If more than two organisms are identified, secondary bacterial peritonitis due to a perforated viscus should be considered.
Spontaneous bacterial peritonitis
- Definition: Bacterial infection of ascitic fluid without other intraabdominal causes leading to secondary bacterial peritonitis.
- Etiology and Risk Factors: Commonly observed in individuals with advanced liver cirrhosis or those undergoing peritoneal dialysis.
- Bacterial Species: Escherichia coli is the most frequent in ascites. Nosocomial cases of spontaneous bacterial peritonitis (SBP) often involve Klebsiella spp. and streptococci.
- Pathophysiology: Bacteria migrate through the intestinal wall, colonizing mesenteric lymph nodes through a process known as bacterial translocation.
- Clinical Features:
- Often asymptomatic
- Possible symptoms include abdominal pain, a tense abdominal wall, and fever.
- Diagnosis:
- Gold standard: Diagnostic paracentesis performed before antibiotic administration.
- SBP is defined as ascitic fluid with more than 250 polymorphonuclear leukocytes per microliter.
- Determining specific pathogens is seldom successful.
- Treatment:
- First-line therapy involves intravenous administration of a third-generation cephalosporin as broad-spectrum therapy.
- Follow-up after 48 hours via repeated paracentesis.
- If granulocyte count decreases to less than 250 per microliter, treatment can be terminated after an additional five days.
- If granulocytes do not decrease by more than 25%, modify treatment based on the resistogram.
- Prognosis: SBP carries a high recurrence and mortality rate.
Hepatic encephalopathy
- Definition: Hepatic encephalopathy (HE) refers to variations in mental status and cognitive function occurring in the context of severe liver disease. Insufficient elimination of metabolic byproducts due to hepatic dysfunction leads to the accumulation of neurotoxic metabolites, notably ammonia.
- Triggers:
- Deterioration of liver function
- Infections, such as spontaneous bacterial peritonitis
- Gastrointestinal bleeding
- Constipation
- Portal vein thrombosis
- Hypovolemia/exsiccosis and electrolyte disturbances (hypokalemia, hyponatremia)
- Renal failure
- Excessive protein consumption
Hepatic encephalopathy-Grading

Hepatic encephalopathy-Neurological effects
- Asterixis
- Fatigue, lethargy, apathy
- Memory loss
- Impaired sleeping patterns
- Irritability
- Disoriented, socially aberrant behavior (e.g., defecating/urinating in public, shouting at strangers, etc.)
- Slurred speech
- Muscle rigidity
- Constructional apraxia: Refers to the inability of patients to accurately copy drawings or three-dimensional constructions, typically resulting from damage to the parietal lobe.

- Earliest sign is altered handwriting .This can be assesed by trail making test.
- Trail maiking test - Join 1 to 25 numbered circles.
- Normally joined in 15-30 seconds .
- If >30 seconds its is impaired.
Hepatic encephalopathy-Diagnosis

Elevated blood ammonia levels
Assessment of mental status
- Number connection test: completed slower than the age-normalized standard or cannot complete
- Psychometry-based diagnostic method (e.g., Mini-Mental State Examination, MMSE) Triphasic Wave in electroencephalogram(EEG) is characteristic of hepatic encephalopathy.
Hepatic encephalopathy-Management

General measures
- Avoidance of trigger substances (e.g., hepatotoxic medication, alcohol)
- Treatment of further complications which might aggravate HE (see "Triggers" above)
Lactulose: synthetic disaccharide laxative
- First-line treatment for HE
Acid peptic disease-Repeats
Q1: Discuss the etiology, clinical features, investigations and drug treatment of Duodenal Ulcer (1996).
Q2: Enumerate the various complications of peptic ulcer (1996).
Q3: Management of perforated duodenal ulcer in a 45 year old man (2000)
Q4: What are the common causes of hematemesis? Discuss the treatment of duodenal ulcer. (2010)
|
7 videos|219 docs
|
FAQs on Acid peptic disease - Medical Science Optional Notes for UPSC
| 1. What are the risk factors for developing acid peptic disease? |  |
| 2. What are the clinical features of acid peptic disease? |  |
| 3. How is H. pylori detected in acid peptic disease? |  |
| 4. What are the surgical management options for acid peptic disease? |  |
| 5. What are the complications of acid peptic disease? |  |

|
Explore Courses for UPSC exam
|

|