Acute hepatitis-Differential diagnosis | Medical Science Optional Notes for UPSC PDF Download
Viral Diseases
- Infectious mononucleosis
- Cytomegalovirus
- Herpes simplex
- Coxsackieviruses
- Toxoplasmosis
Diagnostic Tests
Differential heterophile and serologic tests for these agents can aid in the differential diagnosis when HBsAg, anti-HBc, IgM anti-HAV, and anti-HCV determinations yield negative results.
Drug-Induced Hepatotoxicity
A comprehensive drug history is crucial because certain drugs and anesthetic agents can mimic symptoms of acute hepatitis or cholestasis.
Specific Drugs Associated with Hepatotoxicity
- Anesthetic: Halothane
- Antibiotics: Isoniazid and rifampicin
- Antiepileptic: Phenytoin and carbamazepine
- Antifungal: Ketoconazole
- Antiviral: Zidovudine
Autoimmune hepatitis (recurrent episodes of acute hepatitis)
Alcoholic hepatitis (Stigmata of alcoholism, mild elevations of aminotransferases)
Rare
Occasionally, genetic or metabolic liver disorders (e.g., Wilson's disease, a l antitrypsin deficiency) and nonalcoholic fatty liver disease are confused with acute viral hepatitis.
Because acute hepatitis may present with right upper quadrant abdominal pain, nausea and vomiting, fever, and icterus, it is often confused with acute cholecystitis, common duct stone, or ascending cholangitis.
Viral hepatitis-Routes of Transmission
- Type A:
- Mainly transmitted through the feco-oral route (major route).
- Minor routes include sexual transmission and bloodborne transmission.
- Type B:
- Primarily transmitted parenterally.
- Other modes of transmission include perinatal (vertical), sexual, and horizontal (skin to skin).
- Sexual and perinatal transmission rates are relatively low.
- Recognized with a low rate of secondary transmission to household contacts.
- Type C:
- Transmission occurs primarily through parenteral routes.
- Sexual and perinatal transmission rates are minimal.
- Secondary transmission to household contacts is recognized at a low rate.
- Type D (Delta hepatitis):
- Always associated with hepatitis B (carrier state).
- Transmission mode is identical to hepatitis B.
- Type E:
- Mainly transmitted through the feco-oral route (major).
- Minor routes include the ingestion of undercooked meat or meat products from infected animals.
- Also transmitted through sexual contact and bloodborne routes.
Horizontal transmission, which refers to the spread of HBV from child to child, is the primary cause of a significant number of HBV infections and carriers in regions outside of Asia. Researchers suggest that transmission occurs through direct physical contact among children, particularly those with skin conditions like impetigo and scabies, or with cuts and grazes. Frequently, transmission takes place during activities such as playing together or sharing a bed.
Viral hepatitis-Overview

Acute viral hepatitis-Clinical Features
- Prodromal Phase:
- Before the onset of jaundice by 1-2 weeks, patients may experience constitutional symptoms such as anorexia, nausea, vomiting, fatigue, malaise, arthralgias, myalgias, headache, photophobia, pharyngitis, cough, and coryza.
- Dark urine and clay-colored stools may be noticed by the patient 1-5 days before clinical jaundice sets in.
- Fever is more common in hepatitis A or E compared to hepatitis B or C.
- Icteric Phase:
- During this phase, the liver enlarges and becomes tender, often accompanied by right upper quadrant pain and discomfort.
- Recovery Phase/Post-Icteric Phase:
- Constitutional symptoms subside, but some liver enlargement and abnormalities in liver biochemical tests may persist.
- The post-icteric phase duration varies (2 to 12 weeks), with acute hepatitis B and C typically having a more prolonged recovery.
Note: Infection with HDV can occur concurrently with acute or chronic HBV infection, and the duration of HBV infection influences the duration of HDV infection.
Acute viral hepatitis-Diagnosis
Simplified Diagnostic Approach in Patients Presenting with Acute Hepatitis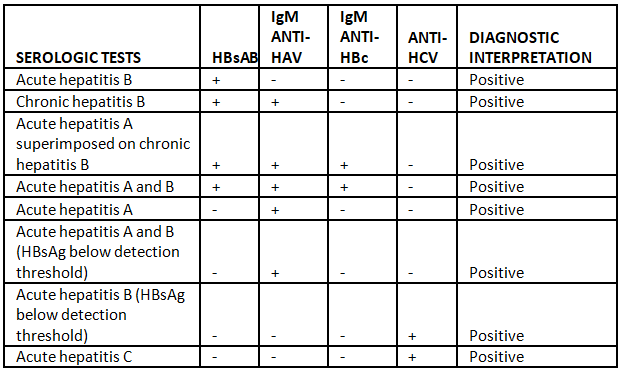
Hepatitis B-Serology
Commonly Encountered Serologic Patterns of Hepatitis B Infection
Chronic Hepatitis B presentation
Jaundice may persist or occur intermittently.
Complications of Cirrhosis in End-Stage Chronic Hepatitis:
- Ascites
- Edema
- Gastroesophageal varices leading to bleeding
- Hepatic encephalopathy
- Coagulopathy
- Hypersplenism
Extrahepatic Complications Associated with Chronic Hepatitis B:
- Tissue deposition of circulating hepatitis B antigen-antibody immune complexes leads to extrahepatic complications.
- These complications include:
- Arthralgias and arthritis
- Purpuric cutaneous lesions (leukocytoclastic vasculitis)
- Immune-complex glomerulonephritis
- Generalized vasculitis (polyarteritis nodosa)
Chronic Hepatitis B Natural History

Chronic Hepatitis C presentation
The clinical features are similar to those observed in chronic hepatitis B.
Note: Immune Complex-Mediated Extrahepatic Complications:
- Immune complex-mediated extrahepatic complications are less common in chronic hepatitis C compared to chronic hepatitis B.
- An exception is essential mixed cryoglobulinemia.
Extrahepatic Complications Unrelated to Immune-Complex Injury in Chronic Hepatitis C:
- Chronic hepatitis C is associated with extrahepatic complications that are not related to immune-complex injury.
- These complications include:
- Sjogren's syndrome
- Lichen planus
- Porphyria cutanea tarda
- Type 2 diabetes mellitus
- Metabolic syndrome
Chronic Hepatitis C Natural History

Chronic Hepatitis
Clinical and Laboratory Features of Chronic Hepatitis
Chronic Hepatitis B Management
Approved Drugs for Chronic Hepatitis B Treatment:
- Injectable interferon (IFN)
- Pegylated interferon (PEG IFN)
- Lamivudine
- Adefovir dipivoxil
- Entecavir
- Telbivudine
- Tenofovir disoproxil fumarate (TDF)
Complications of IFN Therapy:
- Systemic "flu-like" symptoms
- Marrow suppression
- Emotional lability (irritability, depression, anxiety)
- Autoimmune reactions (especially autoimmune thyroiditis)
Miscellaneous side effects, including:
- Alopecia
- Rashes
- Diarrhea
- Numbness and tingling of the extremities
Note:
- With the possible exception of autoimmune thyroiditis, all these side effects are reversible upon dose lowering or cessation of therapy.
- PEG INF-ln these formulations, Polyethylene Glycol (PEG) is added to make interferon last longer in the body. Once-a-week PEG IFN is more effective than the more frequently administered standard IFN.

Chronic Hepatitis B Management
Recommendations for Treatment of Chronic Hepatitis B
American Association for the Study of Liver Diseases (AASLD)
European Association for the Study of the Liver (EASL) guidelines slightly differ
HBeAg Status and Clinical Recommendations for HBV Infection:
- HBeAg-Reactive Disease:
- Clinical Status: Mild disease
- HBV DNA (IU/mL): >2 x 10^1
- ALT: <2 x ULN
- Recommendation: No treatment; monitor. For patients >40, with a family history of non-hepatocellular carcinoma, and/or persistently elevated ALT at the high end of the twofold range, liver biopsy may aid in the decision to treat.
- HBeAg-Reactive Disease:
- Clinical Status: Mild to moderate
- HBV DNA (IU/mL): >2 x 10^3
- ALT: >2 x ULN
- Recommendation: Treat with oral agents (Entecavir or Tenofovir) or PEG IFN as first-line therapy. The oral agents are administered daily for at least a year.
- HBeAg-Reactive Disease:
- Clinical Status: Chronic hepatitis
- HBV DNA (IU/mL): >2 x 10^3 or >ULN
- ALT: Treat with oral agents (Entecavir or Tenofovir) not PEG IFN. Consider treatment until at least 6 months after liver transplantation or indefinitely.
- HBeAg-Reactive Cirrhosis:
- Clinical Status: Decompensated or compensated
- HBV DNA (IU/mL): Undetectable or >ULN
- ALT: Treat with oral agents (Entecavir or Tenofovir) not PEG IFN; refer for continued liver transplantation or observe.
In cases of cirrhosis (decompensated)
Because the emergence of resistance can lead to loss of antiviral benefit and further deterioration in cirrhosis, a low-resistance regimen is recommended—entecavir or tenofovir monotherapy or combination therapy with the more resistance-prone lamivudine (or telbivudine) plus adefovir. Therapy should be instituted urgently.

Treatment considerations: Because HBeAg seroconversion is not an option, the goal of therapy is to suppress HBV DNA and maintain a normal ALT. PEG IFN is administered by subcutaneous injection weekly for a year. Oral agents, entecavir or tenofovir, are administered daily, usually indefinitely.
Chronic Hepatitis C Management
Historical evolution of antiviral therapy for hepatitis C
Since late 2013, the number of new antiviral agents for hepatitis C has expanded substantially, and, currently, PEG IFN-based treatments have been supplanted by six therapeutic regimens: all oral, IFN-free, highly efficacious (>95% SVR), well tolerated, with high barriers to resistance, simple dosing and low pill burdens, treatment durations as brief as 8 to 12 weeks, and, in many cases, pangenotypic efficacy.
Treatment-Naive or Relapsed After Prior PEG IFN/Ribavirin Therapy:
Genotype 1a:
- Ledipasvir + sofosbuvir for 12 weeks (consider 8 weeks for noncirrhotic patients with HCV RNA <6 x 10^6 IU/mL).
- Paritaprevir/ritonavir + ombitasvir + dasabuvir + RBV for 12 weeks (no cirrhosis) or 24 weeks (cirrhosis).
- Sofosbuvir + simeprevir for 12 weeks (no cirrhosis) or ± RBV for 24 weeks (cirrhosis).
- Daclatasvir + sofosbuvir for 12 weeks (no cirrhosis) or ± RBV for 24 weeks (cirrhosis).
- Grazoprevir + elbasvir for 12 weeks (no cirrhosis or cirrhosis sans ELB NS5A RASs) or + RBV for x 16 weeks (ELB NS5A RASs).
- Sofosbuvir + velpatasvir for 12 weeks.
Genotype 1b:
- Ledipasvir + sofosbuvir for 12 weeks (consider 8 weeks for noncirrhotic patients with HCV RNA <6 x 10^6 IU/mL).
- Paritaprevir/ritonavir + ombitasvir + dasabuvir for 12 weeks.
- Sofosbuvir + simeprevir for 12 weeks (no cirrhosis) or ± RBV for 24 weeks (cirrhosis).
- Daclatasvir + sofosbuvir for 12 weeks (no cirrhosis) or ± RBV for 24 weeks (cirrhosis).
- Grazoprevir + elbasvir for 12 weeks.
- Sofosbuvir + velpatasvir for 12 weeks.
Genotype 2:
- Sofosbuvir + velpatasvir for 12 weeks.
- Daclatasvir + sofosbuvir (no cirrhosis) for 12 weeks or 16-24 weeks (cirrhosis).
Genotype 3:
- Sofosbuvir + velpatasvir for 12 weeks.
- Daclatasvir + sofosbuvir for 12 weeks (no cirrhosis) or ± RBV for 24 weeks (cirrhosis).
Genotype 4:
- Sofosbuvir + velpatasvir for 12 weeks.
- Ledipasvir + sofosbuvir for 12 weeks.
- Paritaprevir/r + ombitasvir + RBV for 12 weeks (no dasabuvir).
- Grazoprevir + elbasvir for 12 weeks.
Genotypes 5, 6:
- Sofosbuvir + velpatasvir for 12 weeks.
- Ledipasvir + sofosbuvir for 12 weeks.
Management Specific to Genotype:
- Treatment is genotypic-specific, and the choice depends on the presence or absence of cirrhosis.
HCV Genotypes:
- HCV has six genotypes (1 through 6) with labeled subtypes (e.g., genotypes 1a and 1b).
- Most individuals are infected with a single, dominant genotype, although mixed infections with more than one genotype are possible.
- HCV 1 is difficult to treat
- Genotype lb-high chance of cirrhosis
- Genotype lb and 3-increase risk of cirrhosis
All patients with chronic HCV infection (detectable HCV RNA, with or without elevated ALT) except for those with short life expectancies owing to comorbid conditions. Anti HCV treatment is contraindicated during pregnancy.
Perinatal hepatitis B
Maternal screening for HBsAg should be performed on all women at the first prenatal visit. The risk of perinatal transmission is high with Hepatitis B, especially if the maternal viral load is increased. Perinatal transmission occurs primarily in infants born to mothers with chronic hepatitis B or (rarely) mothers with acute hepatitis B during the third trimester of pregnancy or during the early postpartum period.
- Mode of delivery: Spontaneous vaginal delivery is an option.
- Newborn immunization: Administration of the first dose of the hepatitis B vaccine series along with one dose of HBIG (hepatitis B immune globulin) should occur within 12 hours of birth.
- Breastfeeding: Permitted, provided that passive-active post-exposure prophylaxis has been administered.
- Infected newborns: Typically asymptomatic, with up to a 90% likelihood of developing chronic infection. If left untreated, there is a significant risk of cirrhosis and progression to hepatocellular carcinoma.
Emergent management of hematemesis
- Assessment of Blood Loss:
- Check for signs of shock, including cold and clammy extremities.
- Observe for a feeble or thready pulse, tachycardia, and peripheral cyanosis (in severe cases).
- Note anxiety and restlessness in the patient.
- Monitor for a systolic blood pressure (SBP) below 90 mmHg.
- Keep track of urine output, aiming for at least 20 ml/hr.
- Diagnostic Procedures:
- Pass a Ryles tube and aspirate to detect concealed hemorrhage and dislodge clots on ulcers, aiding active vasoconstriction.
- Conduct investigations:
- Serial measurements of hemoglobin (Hb) and packed cell volume (PCV) every 12 hours.
- Blood grouping and typing, liver function tests (LFT), renal function tests (RFT), and coagulation profile.
- Emergency upper endoscopy.
- Treatment Measures:
- Establish intravenous (IV) access with 2 large-bore needles for fluid replacement and blood transfusions.
- Administer oxygen supplementation.
- Initiate nil by mouth or Ryles tube feeding to reduce the risk of aspiration.
- Consider antacids administration.
- Perform intravenous proton pump inhibitor (IVPPI).
- Reducing Portal Pressure:
- Administer injection octreotide, starting with a single dose of 100 micrograms IV, followed by a maintenance dose of 50-100 micrograms per hour infusion for 3-5 days.
- Consider other drugs like somatostatin, vasopressin, or terlipressin to reduce portal pressure.
- Sengstaken Blakemore Tube:
- Infuse 75 ml of air into the esophageal balloon to exert pressure on bleeding vessels.
- After 12 hours, recheck for bleeding, and the tube should be decompressed every 12 hours to prevent necrosis.

|
7 videos|219 docs
|
FAQs on Acute hepatitis-Differential diagnosis - Medical Science Optional Notes for UPSC
| 1. What are the routes of transmission for viral hepatitis? |  |
| 2. What is the overview of viral hepatitis? |  |
| 3. What are the clinical features of acute viral hepatitis? |  |
| 4. How is hepatitis B diagnosed? |  |
| 5. What are the symptoms of chronic hepatitis C? |  |

|
Explore Courses for UPSC exam
|

|
















