Allergic dermatitis and Eczema | Medical Science Optional Notes for UPSC PDF Download
| Table of contents |

|
| Eczema |

|
| Atopic dermatitis (AD) |

|
| Contact Dermatitis |

|
| Classification of photosensitivity diseases |

|
| Chronic actinic dermatitis/persistent Light reaction |

|
| Allergic dermatitis/Eczema-Repeats |

|
Eczema
- It is a cutaneous inflammatory response pattern, clinically characterized by itching, redness, and weeping in its acute form, and dryness and lichenification in its chronic form.
- Histologically, it exhibits lymphocyte infiltrate, spongiosis (intercellular edema), and varying degrees of acanthosis (increased thickness of the epidermal layer).
- Eczema serves as the common expression for several disorders, classified as follows:
- Endogenous (Constitutional Type)
- Atopic dermatitis
- Seborrheic dermatitis
- Nummular or discoid dermatitis
- Pompholyx
- Stasis eczema
- Exogenous (Contact)
- Irritant dermatitis
- Allergic dermatitis
- Photodermatitis
- Unclassified
- Lichen simplex
- Neurodermatitis
Atopic dermatitis (AD)
- Atopic Dermatitis (AD) represents the cutaneous manifestation of the atopic state, characterized by a family history of asthma, allergic rhinitis, or eczema.
- The etiology of AD is only partially understood, but there is a clear genetic predisposition.
- An impaired epidermal barrier is a characteristic defect in AD pathophysiology, often associated with a mutation in the filaggrin gene, responsible for encoding a structural protein in the stratum corneum.
- The clinical presentation varies with age:
- In infants, there are weeping inflammatory patches and crusted plaques on the face, neck, and extensor surfaces.
- In children and adolescents, dermatitis typically affects flexural skin, especially in the antecubital and popliteal fossae.
Clinical Features of Atopic Dermatitis
- Pruritus and scratching
- Lesions present in antecubital and popliteal fossae, neck, hands, eyelids.
- Acute lesions exhibit erythema, fine scale, crust, indistinct borders, and excoriations, while chronic lesions show lichenification (increased skin markings) and excoriations.
- Lesions worsened by dry skin
- Personal or family history of atopy (asthma, allergic rhinitis, food allergies, or eczema)
- Clinical course lasting >6 weeks
- Cutaneous stigmata of AD, such as perioral pallor, an extra fold of skin beneath the lower eyelid (Dennie-Morgan folds), increased palmar skin markings, and an increased incidence of cutaneous infections, particularly with Staphylococcus aureus.
Treatment of Atopic Dermatitis (AD)
- Daily Routine:
- Take a daily bath.
- Use mild bath soap.
- Moisturize the entire body with a moisturizer.
- Topical Agents:
- Apply topical anti-inflammatory agents on dermatitis areas.
- Options include low to moderate-potency topical glucocorticoids, non-glucocorticoid anti-inflammatory agents (e.g., tacrolimus ointment, pimecrolimus cream).
- Systemic Antibiotics:
- Use systemic antibiotics effective against Staphylococcus aureus.
- Pruritus Control:
- Manage pruritus with sedative antihistamines.
- Severe Exacerbations:
- Severe exacerbations unresponsive to topical glucocorticoids may require systemic glucocorticoids.
Barrier-Repair Products
- Newer therapies aim to restore the impaired epidermal barrier in AD.
- Filaggrin, a filament-aggregating protein, plays a vital role in epidermal differentiation and barrier function.
- Null mutations in the filaggrin gene are a significant risk factor for AD development.
- Atopic skin lacks filaggrin degradation products or ceramides.
- Advances in understanding AD pathophysiology involve barrier therapy and the development of moisturizers and topical products targeting reduced ceramides and natural moisturizing factors.
Moisturization
- Emollients, including creams and ointments, enhance the stratum corneum's barrier function by supplying water and lipids.
Contact Dermatitis
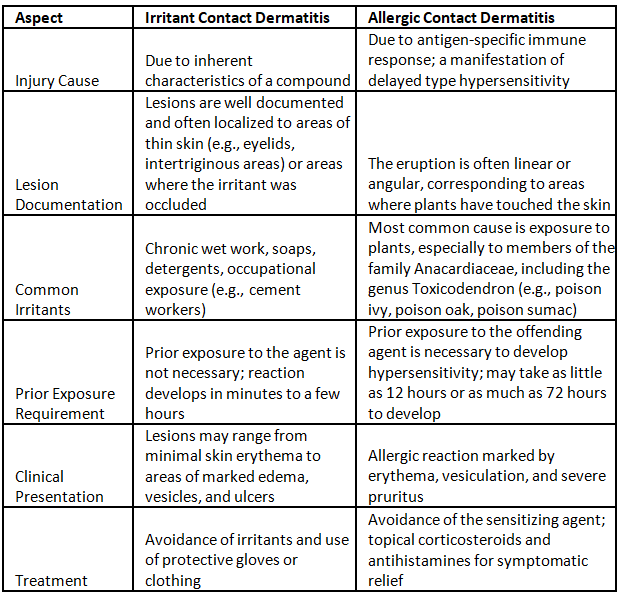
Treatment
- Remove offending agent
- High potency topical glucocorticoids (Topical or systemic)
- Identification of contact allergen a) Question about occupational exposures, topical medications b) Patch testing
Classification of photosensitivity diseases
Photosensitivity is heightened skin sensitivity or an unusual reaction when your skin is exposed to UV radiation from sunlight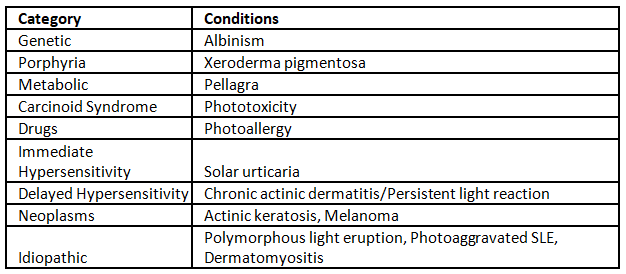
Photoallergens
- Photosensitivity induced by drugs includes reactions triggered by medications like Diclofenac, chlorpromazine, Fluoroquinolones (FQs), Sulfonamides, sulfonylureas, thiazides, among others.
- Photocontact dermatitis involves exposure to phototoxic chemicals found in plants, vegetables, and fruits containing psoralens. Additionally, fragrances in cosmetics, certain sunscreen chemicals, dyes, and disinfectants can also cause photocontact dermatitis.
Chronic actinic dermatitis/persistent Light reaction
- Chronic actinic dermatitis is an uncommon form of persistent photosensitivity, primarily affecting elderly men who have a prolonged history of preexisting allergic contact dermatitis or photosensitivity.
- Individuals with chronic actinic dermatitis exhibit heightened sensitivity to UV-B, UV-A, and visible wavelengths of light.
- The rash associated with this condition may develop on sun-exposed areas, typically affecting the face, neck, and upper chest in a V-shaped distribution, with the backs of hands being commonly affected.
- Lesions are characterized by redness, inflammation, scaling, and lichenification (thickened and hardened patches of skin).
- Itchiness is a common symptom associated with the rash.
Diagnosis is by
Diagnosis of photosensitivity reactions involves specific procedures.
- Phototest procedure: In suspected cases of phototoxicity, determining the minimal erythemal dose (MED) is crucial. This involves exposing the patient to a suspected agent, determining the MED, and then repeating the MED after discontinuation of the agent to identify the causative drug or chemical.
- Photopatch testing: This diagnostic method is employed to confirm the diagnosis of photoallergy. It involves applying a series of known photoallergens to the skin in duplicate. One set is then irradiated with a suberythemal dose of UV-A. The development of eczematous changes at sites exposed to the sensitizer and light is considered a positive result.
Management
- Patients diagnosed with chronic actinic dermatitis typically exhibit heightened sensitivity to a broad spectrum of UV radiation. Managing this condition involves rigorous photoprotection measures, including sun avoidance, the use of high-SPF (>30) sunscreens, and, in severe cases, systemic immunosuppression like azathioprine.
- The primary approach to managing drug photosensitivity is eliminating exposure to the chemical agents causing the reaction and minimizing sun exposure.
- For alleviating acute symptoms of phototoxicity, strategies include cool moist compresses, topical glucocorticoids, and NSAIDs administered systemically. In severe cases, a tapered course of systemic glucocorticoids may be beneficial, and judicious use of analgesics may be necessary.
- Similar management strategies apply to photoallergic reactions. Additionally, individuals with persistent light reactions and chronic actinic dermatitis must receive meticulous protection against light exposure.
- In cases where chronic systemic high-dose glucocorticoids pose unacceptable risks, immunosuppressive drugs like azathioprine, cyclophosphamide, cyclosporine, or mycophenolate mofetil may be considered for selected patients.
Seborrheic dermatitis
- Manifests on the scalp and is identified as severe dandruff.
- Other affected areas include the face (eyebrows, eyelids, glabella, and nasolabial folds), central chest, axilla, groin, submammary folds, and gluteal clefts.
- Evident by greasy scales covering erythematous patches or plaques.
- Termed "cradle cap" when occurring within the first few weeks of life, typically on the scalp.
- Associated disorders may include HIV, Parkinson’s disease, or recent cerebrovascular accident (CVA).
- Treatment involves the use of topical glucocorticoids, antifungal agents (such as ciclopirox cream), and antidandruff shampoos for the scalp and beard.
Allergic dermatitis/Eczema-Repeats
Q1: Enumerate differences between Allergic and Irritant contact dermatitis (2009).
Q2: Mention common incriminating allergens. Discuss the management of allergic dermatitis. (2010)
Q3: Classify eczema. What is the diagnostic test for allergic contact dermatitis? Discuss in brief the management of atopic dermatitis. (2012)
Q4: How will you differentiate between irritant and allergic contact dermatitis? Write the salient differentiating points of both. (2013)
Q5: A housewife develops itching and irritation in the webs of the hands, following peeling/cutting of vegetables such as jackfruit and lady's finger. It is relieved slightly on washing with cold water. (2016)
(i) What is the likely diagnosis?
(ii) Discuss the etiopathogenesis, management and prevention of this condition.
Q6: A mason working at a building site has developed itchy, oozing lesions of hands and feet. What is the likely diagnosis? How will you identify the causative agent in him and manage the case? (2014)
Q7: A 45-year-old gentleman, agriculturist by occupation, presents with recurrent itchy scaly lesions over face and limbs of one year duration. Examination revealed hyper pigmented scaly lesions over face, neck and upper and lower limbs. There were involvement of skin creases, eyelids, retro auricular areas and nasolabial folds. He gave history of photosensitivity. (2017)
(i) What is your likely diagnosis?
(ii) What tests will you perform to establish the cause of his condition? Describe in brief.
(iii) How will you treat this gentleman?
Q8: A 45-year-old lady develops itchy, hyper pigmented, scaly lesions on face. These lesions become worse after the use of hair dye which she started using five months earlier. (2015)
(i) What is the most likely diagnosis?
(ii) How can this diagnosis be confirmed?
(iii) What medical advice can be given to this lady?
|
7 videos|236 docs
|
FAQs on Allergic dermatitis and Eczema - Medical Science Optional Notes for UPSC
| 1. What is eczema and what are its common symptoms? |  |
| 2. What is the difference between atopic dermatitis and contact dermatitis? |  |
| 3. How are photosensitivity diseases classified? |  |
| 4. What is chronic actinic dermatitis and what are its symptoms? |  |
| 5. Can eczema be cured completely? |  |















