Upper Limbs | Medical Science Optional Notes for UPSC PDF Download
Brachial Plexus
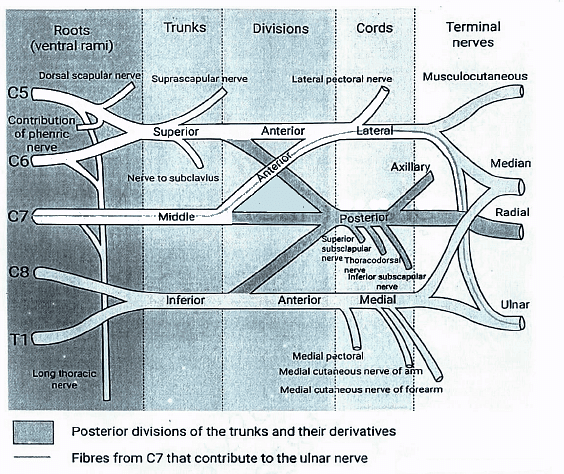
The brachial plexus originates from the merging of the ventral rami of the lower four cervical nerves and the majority of the first thoracic ventral ramus.
The plexus consists of roots, trunks, divisions, cords and branches

Sensory innervation of Hand

Brachial plexus injuries
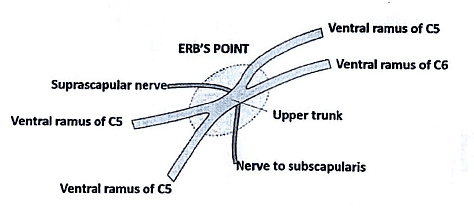
Erb's Paralysis refers to the impairment of the upper trunk region of the brachial plexus, specifically identified at Erb's point where six nerves converge. This condition results from injury to the upper trunk.
Causes:
(a) Commonly occurring due to undue separation of the head from the shoulder, observed in situations such as birth injuries, falls on the shoulder, and incidents during anesthesia.
Nerve roots involved: Mainly C5 and partly C6.
Muscles affected: Mainly biceps, deltoid, brachialis, and brachioradialis, along with partial involvement of supraspinatus, infraspinatus, and supinator.
(b) Clinical presentation:
Arm: Hanging by the side, adducted, and medially rotated.
Forearm: Extended and pronated.
The resulting deformity is commonly referred to as 'policeman's tip hand' or 'porter’s tip hand.'
Brachial Plexus Injuries
Klumpke's Paralysis originates from injury to the lower trunk of the brachial plexus and is typically caused by excessive abduction of the arm, such as when grasping an object after a fall from a height or occasionally during birth.
Key details:
- Site of injury: Lower trunk of the brachial plexus.
- Cause of injury: Excessive arm abduction, seen in situations like holding onto something with the hands after a fall or in certain birth injuries.
- Nerve roots involved: Mainly T1 and partly C8.
- Muscles paralyzed:
- Intrinsic muscles of the hand (T1).
- Ulnar flexors of the wrist and fingers (C8).
Deformity (hand position): The resulting deformity is a claw hand due to the unopposed action of the long flexors and extensors of the fingers. In a claw hand, there is hyperextension at the metacarpophalangeal joints and flexion at the interphalangeal joints.

Ulnar nerve-Gross Anatomy
The ulnar nerve, a continuation of the medial cord of the brachial plexus, does not give rise to branches in the upper arm. Its course begins as it enters the posterior compartment of the upper arm midway down its length, piercing the medial intermuscular septum. It then traverses behind the medial epicondyle of the humerus, enters the forearm, and descends to the wrist deep to the flexor carpi ulnaris.
The ulnar nerve provides innervation to the flexor carpi ulnaris and the ulnar half of the flexor digitorum profundus. Just before reaching the wrist, it emits a dorsal cutaneous branch, supplying the skin over the dorsal aspect of the little finger and the ulnar half of the ring finger. Crossing into Guyon's canal superficially to the flexor retinaculum, it further divides into a motor branch, which serves the hypothenar muscles, intrinsic hand muscles (excluding the radial two lumbricals), and adductor pollicis. Additionally, cutaneous branches supply the skin of the palmar aspect of the little finger and the ulnar half of the ring finger.

Ulnar nerve-Clinical Anatomy
The ulnar nerve, often referred to as the 'musician's nerve,' plays a crucial role in controlling the fine movements of the fingers due to its extensive motor distribution to the short muscles of the hand.
The ulnar nerve is particularly prone to injury at two primary locations:
(a) Behind the medial epicondyle of the humerus
(b) At the wrist
In both instances, it is relatively superficial and susceptible to damage. An ulnar nerve lesion at the wrist results in a condition known as 'ulnar claw-hand,' primarily affecting the ring and little fingers.
A true claw-hand, involving all the fingers, is brought about by a combined lesion of the ulnar and median nerves.
Ulnar claw-hand exhibits the following characteristics:
(a) Hyperextension at the metacarpophalangeal joints and flexion at the interphalangeal joints, primarily affecting the ring and little fingers more than the index and middle fingers. The little finger is held in abduction by extensor muscles, leading to hollowing of the intermetacarpal spaces due to wasting of the interosseous muscles.
(b) Sensory loss is localized to the medial one-third of the palm and the medial one and a half fingers, including their nail beds.
(c) Vasomotor changes: Skin areas experiencing sensory loss are warmer due to arteriolar dilatation, and dryness is observed due to the absence of sweating resulting from the loss of sympathetic supply.
(d) Trophic changes: Prolonged cases of paralysis result in dry and scaly skin. Nails become prone to cracking, accompanied by atrophy of the pulp of the fingers.
(e) The patient faces difficulty in spreading out the fingers due to the paralysis of the dorsal interossei. Additionally, there is a loss of power in adduction of the thumb and flexion of the ring and little fingers.
It's important to note that, compared to median nerve lesions, ulnar nerve lesions result in a relatively functional hand.
Radial nerve-Gross Anatomy
The radial nerve courses behind the third part of the axillary artery and the upper segment of the brachial artery, positioned anteriorly to the Subscapularis and the tendons of latissimus dorsi and teres major. Alongside the profunda brachii artery, it takes a dorsal inclination, traversing the triangular space below the lower border of teres major, between the long head of the triceps and the humerus.
Within this space, it provides innervation to the long head of the triceps and gives rise to the posterior cutaneous nerve of the arm, which supplies the skin along the posterior surface of the upper arm. Subsequently, the nerve spirals obliquely across the back of the humerus, initially positioned posterior to the uppermost fibers of the medial head of the triceps in the first part of the spiral groove. In this region, it issues a muscular branch to the lateral head of the triceps and another branch that traverses the medial head of the triceps to reach the anconeus.
Upon reaching the lateral side of the humerus, the radial nerve penetrates the lateral intermuscular septum to access the anterior compartment. It then descends deep within a groove between the brachialis and, proximally, the brachioradialis, and more distally, the extensor carpi radialis longus. Anterior to the lateral epicondyle, the nerve bifurcates into superficial and deep terminal rami.

Radial nerve-Clinical Anatomy
- Lesions affecting the radial nerve at its origin from the posterior cord in the axilla can result from extended pressure, such as that caused by a lengthy crutch (referred to as crutch palsy). Additionally, compression against the humerus may transpire when the arm is rested on a sharp edge, such as the back of a chair, a condition colloquially known as 'Saturday night palsy.'
- These injuries manifest with weakened brachioradialis, accompanied by muscle wasting and loss of reflex. The consequence includes both wrist and finger drop, attributed to the diminished strength of wrist and finger extensors, as well as weakness in extensor pollicis longus and abductor pollicis longus. Sensory impairment or paraesthesiae may be present in the superficial radial nerve's distribution. Nevertheless, due to nerve overlap, anesthesia is typically confined to a small area on the dorsum of the hand between the first and second metacarpal bones.
Median nerve-Gross Anatomy
The median nerve is the result of the convergence of the terminal branches of the lateral and medial cords of the brachial plexus. It does not generate branches in the upper arm. Upon entering the forearm between the two heads of pronator teres, it emits the anterior interosseous nerve, which innervates all the flexor muscles of the forearm except for flexor carpi ulnaris and the ulnar half of flexor digitorum profundus.
The median nerve itself passes beneath the flexor retinaculum at the wrist. Upon entering the palm, it issues motor branches to the thenar muscles and the radial two lumbricals, along with cutaneous branches to the palmar aspect of the thumb, index and middle fingers, and the radial half of the ring finger.

Median nerve-Clinical Anatomy
Carpal tunnel syndrome is a condition characterized by the compression of the median nerve at the wrist within the carpal tunnel, leading to symptoms such as paresthesia, pain, and numbness in the distribution of the median nerve.
The carpal tunnel is a narrow passageway located on the anterior aspect of the wrist, serving as the entry point to the palm for various tendons and the median nerve. It is created by two layers: a deep carpal arch and a superficial flexor retinaculum (transverse carpal ligament). The deep carpal arch forms a concave surface, converted into a tunnel by the overlying flexor retinaculum.
Contents
Within the carpal tunnel are a total of 9 tendons, enveloped by synovial sheaths, and the median nerve.
Tendons
- Tendon of flexor pollicis longus
- Four tendons of flexor digitorum profundus
- Four tendons of flexor digitorum superficialis

Causes of Carpal Tunnel Syndrome
- Myxedema
- Edema
- Diabetes Mellitus
- Idiopathic
- Acromegaly
- Neoplasms (Ganglion, Lipoma)
- Trauma
- Rheumatoid Arthritis
- Amyloidosis
- Pregnancy
Mnemonic: MEDIAN nerve TRAPped

Upper limb -Repeats
- Describe course, relations and distribution of ulnar nerve in hand. Add a note on its applied anatomy (2005).
- Describe Carpal tunnel syndrome, its manifestations and the causes. (2011)
- Describe the effects of damage to radial nerve at the level of deltoid tuberosity. (2014)
- Give a brief account of ulnar nerve. (2016)
|
7 videos|219 docs
|
FAQs on Upper Limbs - Medical Science Optional Notes for UPSC
| 1. What is the brachial plexus? |  |
| 2. What is the function of the ulnar nerve? |  |
| 3. What are the gross anatomical features of the ulnar nerve? |  |
| 4. What are some clinical conditions associated with the ulnar nerve? |  |
| 5. How can ulnar nerve injuries be treated? |  |

|
Explore Courses for UPSC exam
|

|
















