Steven Johnson syndrome (SJS) | Medical Science Optional Notes for UPSC PDF Download
| Table of contents |

|
| Introduction |

|
| Steven Johnson syndrome, Toxic epidermal necrosis (SJS)/TEN) |

|
| Prognostic Scoring |

|
| Erythema multiforme |

|
| TEN vs EM |

|
| Steven Johnson syndrome-Repeat |

|
Introduction
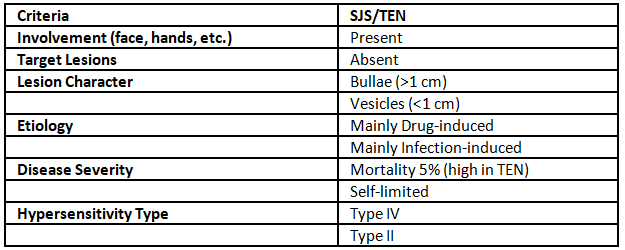
SJS is identified by the presence of blisters and the detachment of mucosal and epidermal layers, which occurs due to complete-depth epidermal necrosis. The classification Stevens-Johnson syndrome/toxic epidermal necrolysis overlap is employed for situations where detachment ranges from 10% to 30%, while TEN is utilized for cases involving more than 30% detachment.
Etiology
The origin of SJS/TEN is believed to stem from an immune system malfunction, with drug exposure or infections serving as potential triggers. SJS is categorized as a type IV hypersensitivity reaction, wherein a drug or its metabolite prompts cytotoxic T cells (specifically CD8+ T cells) and T helper cells (specifically CD4+ T cells) to initiate autoimmune responses targeting the body's own tissues.
Steven Johnson syndrome, Toxic epidermal necrosis (SJS)/TEN)
SJS is frequently triggered by certain drugs, including:
- Sulfonamides
- Nevirapine
- Allopurinol
- Lamotrigine
- Aromatic anticonvulsants (such as phenytoin, barbiturates, carbamazepine)
- NSAIDs (specifically oxicam)
Factors that increase the risk of SJS include:
- HIV/AIDS
- Systemic lupus erythematosus
Presentation
Individuals experiencing SJS, SJS/TEN, or TEN typically exhibit a sudden onset of painful skin lesions, accompanied by a high fever exceeding 39°C (102.2°F), a sore throat, and conjunctivitis arising from mucosal lesions. The mortality rates for those affected by SJS and TEN are approximately 10% and 30%, respectively.
Diagnosis
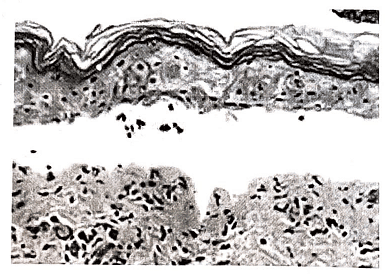
Nikolsky's sign proving positive is valuable in confirming the diagnosis of SJS and TEN. A prompt diagnosis can be facilitated by employing frozen-section skin biopsy. The histopathological features include extensive epidermal necrosis with limited inflammation. The acute nature of the condition is evident in the distinctive basket-weave pattern observed in the stratum corneum.
Treatment
- Considered a dermatological emergency.
- Optimal outcomes are achieved through prompt identification, immediate cessation of any suspected medication, supportive care, and vigilant monitoring of ocular issues and infections.
- Early in the disease's progression, systemic glucocorticoid therapy (1-2 mg/kg of prednisone) may offer some benefit, but prolonged use of systemic glucocorticoids has been linked to increased mortality.
- Cyclosporine could be a potential treatment option for SJS/TEN.
- Further research is required to evaluate the benefits of intravenous immunoglobulin (IVIG) in the management of SJS/TEN.
Prognostic Scoring
The likelihood of death from SJS/TEN can be assessed by employing the SCORTEN scale, which considers various prognostic indicators. It is advisable to calculate the SCORTEN within the initial 3 days of hospitalization.
This scale systematically assigns scores to seven independent risk factors, enabling the determination of the mortality rate for the individual patient.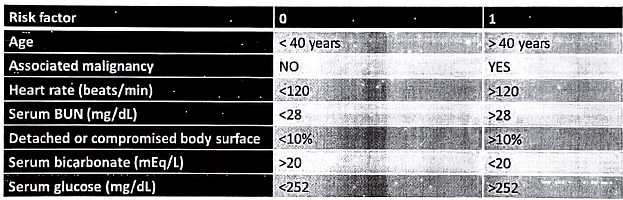
The more risk factors present, the higher the SCORTEN score, and the higher the mortality rate, as shown in the following table.
Erythema multiforme
Erythema multiforme is an immune system overreaction commonly triggered by infections, particularly the herpes simplex virus (HSV). It manifests as a skin eruption characterized by distinctive target lesions. This form of erythema is believed to involve immune complex deposition, predominantly IgM-bound complexes, in the surface microvasculature of the skin and oral mucous membrane. Typically, it follows an infection or exposure to certain drugs.
There are two forms of Erythema Multiforme:
- Mild to moderate, known as erythema multiforme minor, often associated with HSV.
- Severe, referred to as erythema multiforme major, which can be triggered by HSV, mycoplasma, or certain medications. This severe form involves mucous membrane participation and systemic symptoms.
Causes
Infections:
- Bacterial infections such as Bacillus Calmette-Guerin (BCG) vaccination, hemolytic Streptococci, legionellosis, leprosy, Neisseria meningitidis, Mycobacterium, Pneumococcus, Salmonella species, Staphylococcus species, and Mycoplasma pneumoniae, as well as Chlamydial infections.
- Fungal infection caused by Coccidioides immitis.
- Parasitic infections from Trichomonas species and Toxoplasma gondii.
- Viral infections, especially Herpes simplex.
"Erythema multiforme typically resolves on its own and generally does not necessitate treatment."
Drug reactions:
- Antibiotics, including sulphonamides and penicillin.
- Anticonvulsants such as phenytoin and barbiturates.
- Aspirin.
- Antituberculoid medications.
- Allopurinol.
Clinical Features
- The severity of erythema multiforme can range from a mild, self-limiting rash to a more severe and life-threatening form known as erythema multiforme major, which also affects mucous membranes.
- Erythema multiforme minor is characterized by typical target lesions or raised, edematous papules that are distributed acrally (on the extremities).
- Erythema multiforme major exhibits typical target lesions or raised, edematous papules distributed acrally, along with the involvement of one or more mucous membranes.
- The characteristic target lesion, also referred to as an iris lesion, in erythema multiforme has distinct features: a well-defined margin, a regular round shape, and three concentric color zones. The center is dusky or dark red with a blister or crust, the next ring is a paler pink and raised due to edema (fluid swelling), and the outermost ring is bright red.
TEN vs EM
Steven Johnson syndrome-Repeat
Q1: Describe Etiology, Clinical features and Prognostic scoring points of mortality of Stevens- Johnson syndrome. (2009)
Q2: What are points of difference between Erythematic Multiforme and toxic Epidermal Necrolysis (TEN)? (2009)
Q3: How will you manage a case of Stevens-Johnson syndrome in an adult? (2011)
Q4: What is Stevens - Johnson syndrome (SJS)? Enumerate the common etiological factors and pathological events leading to its clinical manifestations. (2014)
|
7 videos|219 docs
|
FAQs on Steven Johnson syndrome (SJS) - Medical Science Optional Notes for UPSC
| 1. What is Steven Johnson syndrome (SJS) and Toxic epidermal necrosis (TEN)? |  |
| 2. What is the prognostic scoring system used for Steven Johnson syndrome (SJS) and Toxic epidermal necrosis (TEN)? |  |
| 3. What is the difference between Erythema multiforme (EM) and Steven Johnson syndrome (SJS)? |  |
| 4. How can one differentiate between Toxic epidermal necrosis (TEN) and Erythema multiforme (EM)? |  |
| 5. Can Steven Johnson syndrome (SJS) recur? |  |

|
Explore Courses for UPSC exam
|

|

















