Breast | Medical Science Optional Notes for UPSC PDF Download
| Table of contents |

|
| Nipple Discharge |

|
| Cystic lesions of breast |

|
| Breast carcinoma-Clinical features |

|
| Algorithm for management of operable breast cancer |

|
| Breast-Repeats |

|
Nipple Discharge

Treatment
- Exclude the possibility of carcinoma and provide reassurance in the majority of cases.
- In cases where the symptoms are intolerable, microdochectomy (removal of the affected duct, typically a single duct) can be considered.
- The Hadfield procedure is employed when the source of the discharge is unknown or when discharge is from multiple ducts. This involves a subareolar resection and cone excision of major ducts.
Cystic lesions of breast
- Arising from the non-integrated involution of stroma and epithelium.
- Typically observed in the last decade of the reproductive phase of life.
- Frequently presents as multiple and bilateral occurrences.
- Onset of breast symptoms can be sudden.
- Differential diagnosis includes fluid-filled structures like simple cysts, complex or complicated cysts, galactocele, hematoma, fat necrosis or oil cyst, breast abscess or mastitis, intracystic papilloma, necrotizing neoplasm, and malignancy (cystadenocarcinoma).
- Diagnosis is established through aspiration and/or ultrasound examination.
Treatment
- Aspiration is an option for a single cyst or a small cluster of cysts. Complete resolution without blood-stained fluid indicates no further intervention is needed.
- However, recurrence, occurring in 30% of cases, may necessitate reaspiration.
- If a residual lump remains or if the aspirated fluid is blood-stained, it is advisable to pursue a core biopsy or local excision for a histological diagnosis. This is especially true if the cyst recurs persistently. Such diagnostic measures help rule out cystadenocarcinoma, a condition more prevalent in elderly women.
Benign Breast Disorder Classification
Congenital Disorders
- Inverted Nipple
- Supernumerary Breasts/Nipples
Injury
- Costochondritis (Pregnancy-Related)
Inflammation/Infection
- Fibroadenoma and Related Disorders
- Duct Ectasia/Periductal Mastitis
- Non-Breast Disorders Including Tietze's Disease
- Galactocele
- Sebaceous Cysts and Other Skin Conditions
- Lactational Abscess
ANDI
Aberrations of Normal Development and Involution (ANDI) - Fundamental Principles:
- Benign disorders and diseases of the breast are intricately linked to the typical processes of reproductive life and the subsequent involution phase.
- A spectrum of breast conditions exists, spanning from normal to disorder to disease.
- The ANDI classification comprehensively covers all aspects of breast conditions, encompassing pathogenesis and the extent of abnormality.
The table's horizontal component delineates ANDI across a continuum, ranging from normal to mild abnormality (disorder) to severe abnormality (disease). Meanwhile, the vertical component signifies the timeframe during which the condition evolves.
Breast Conditions During Early Reproductive Years (15-25 years)
- Lobular Development
- Fibroadenoma
- Giant Fibroadenoma
- Stromal Development
- Adolescent Gigantomastia Hypertrophy
- Nipple Eversion
- Subareolar Abscess
- Nipple Inversion
- Mammary Duct Fistula
Breast Conditions During Later Reproductive Years (25-40 years)
- Cyclical Changes of Menstruation
- Epithelial Hyperplasia of Pregnancy
- Cyclical Mastalgia
- Nodularity
- Bloody Nipple Discharge
- Incapacitating Mastalgia
Breast Conditions During Involution (35-55 years)
- Lobular Involution
- Macrocytosis
- Sclerosing Lesions
- Dilatation Duct Ectasia
- Periductal Mastitis
- Sclerosis
- Nipple Retraction
- Epithelial Turnover
- Epithelial Hyperplasia
Fibroadenoma of Breast
Age Group 15-25 Years:
- Hyperplasia of a single lobule enclosed by a distinct capsule.
- Generally stable in nature.
- Small fibroadenomas (<1 cm) are considered normal, while larger ones (1-3 cm) are categorized as a disorder. Giant fibroadenomas (>3 cm) or the presence of multiple small fibroadenomas (more than 5 in one breast) suggest a diseased state.
- Biopsy is recommended if the individual is aged over 25 and exhibits atypical features on ultrasound.
- Treatment involves enucleation through a cosmetically appropriate incision, especially in cases with suspicious cytology, very large fibroadenomas, or patient preference.
- Alternatives include cryoablation, echotherapy (heating with high-frequency ultrasound), or removal using a large core vacuum biopsy system.
Cyclical mastalgia with nodularity
- Old Nomenclature: Previously known as Fibroadenosis.
- Nodularity or Lumpy Breasts:
- Bilateral condition, often observed in the upper outer quadrant.
- Cyclical nature, with lumpiness and tenderness increasing before menstruation.
- Treatment involves reassurance, and reexamination after six weeks, preferably at a different point in the menstrual cycle.
- Cyclical Mastalgia:
- Important to differentiate from non-cyclical mastalgia (associated with periductal mastitis) and referred pain (from chest wall, back, or neck).
- Treatment involves:
- Exclude malignancy.
- Determine whether it is cyclical or non-cyclical.
- For non-cyclical mastalgia, use NSAIDs or inject local anesthetic on a trigger spot.
- For cyclical mastalgia, reassure the patient and recommend adequate firm bra support during the day, a softer bra at night, exclude caffeine, and consider evening primrose oil over three months (effective in >50% of cases).
- In cases of intractable symptoms, consider Danazol 100mg TID or Tamoxifen.
Duct ectasia/periductal mastitis
- Dilatation of Breast Ducts (Duct Ectasia):
- Associated with periductal inflammation.
- Common occurrence in smokers.
- Manifests with brown or green discharge from the nipple.
- The accumulated discharge in the dilated ducts triggers an irritant reaction in surrounding tissue, leading to periductal mastitis, abscess, and possibly fistula formation.
- Chronic Cases:
- Fibrosis can develop, resulting in slit-like nipple retraction.
- Treatment:
- Antibiotic therapy, specifically Co-amoxiclav plus metronidazole, where anaerobic infection is a potential etiological factor.
- Malignancy should be ruled out through mammogram, FNAC (Fine Needle Aspiration Cytology), or biopsy.
- Surgical intervention, such as Haldfield's operation involving the excision of all major ducts, can be pursued for a cure.
- Smoking cessation increases the likelihood of long-term cure.
Retraction of Nipple
- Nipple Retraction:
- Occurs during puberty, presenting as a momentary retraction or inversion of the nipple.
- Slit-like retraction may be associated with duct ectasia and chronic periductal mastitis.
- Circumferential retraction, with or without an underlying lump, could suggest an underlying carcinoma.
- Potential issues with breastfeeding may arise, and infection can occur due to the retention of secretions, particularly during lactation.
- Treatment:
- Spontaneous resolution is common.
- If not, options include:
- Simple cosmetic surgery (with a risk of damaging underlying ducts).
- Mechanical suction.

Mastitis/Breast abscess
- Causation of Lactational Mastitis:
- Newborns act as intermediaries, with 50% harboring staphylococci in the nasopharynx.
- Predominantly caused by S. aureus.
- Higher incidence in women with retracted nipples.
- Treatment:
- Breast support, local heat, and analgesia are recommended.
- Feeding from the affected side can continue if the patient can manage.
- In the cellulitis stage, appropriate antibiotics such as Co-amoxiclav are used. For hospital-acquired staphylococci (often methicillin-resistant), Vancomycin or Clindamycin may be prescribed.
- In the abscess stage, antibiotic usage before drainage is avoided. Ultrasound localization facilitates repeated aspirations under antibiotic cover. Indications for ultrasound-guided aspirations include non-resolving infection within 48 hours, visible induration, and evidence of an underlying abscess. This approach avoids the need for an Incision and Drainage (I&D) procedure, allowing the patient to continue breastfeeding.
- Pus collected during aspiration should be sent for culture.
- In cases requiring I&D, indications include failed resolution with repeated aspirations and marked skin thinning indicating an organizing abscess. This procedure is performed under local anesthesia (EMLA cream applied 30 minutes before surgery). A circumareolar incision is preferred over a radial incision for better cosmetic results. After entering loculi with artery forceps, remaining septa are disrupted, and a drain is inserted for dependent drainage.
Breast carcinoma-Etiology
- Geographical Factors: Predominant in the Western world, with breast cancer being the most common cause of death in middle-aged women.
- Age: Rare occurrence before the age of 20, with an increased risk thereafter.
- Gender: More prevalent in females (F > M), although it accounts for 0.5% of cases in males.
- Genetic Factors: BRCA1 and BRCA2 mutations contribute to the genetic predisposition for breast cancer.
- Diet: Western diets, low intake of phytoestrogens, and alcohol consumption are associated with increased risk.
- Endocrine Factors: Risk factors include nulliparity, late menarche, early menopause, use of oral contraceptive pills, and hormone replacement therapy (HRT). Protective factors include breastfeeding and having the first child at an early age.
- Previous Radiation: A history of previous radiation exposure is also considered a risk factor.
Breast carcinoma-Clinical features
- Localization: Breast cancer is most commonly found in the upper outer quadrant of the breast.
- Clinical Presentation:
- Hard Lump:
- Most breast cancers manifest as a palpable, hard lump.
- Indrawing of the nipple or overlying skin may be associated with the lump.
- Peau d'Orange:
- With local disease progression, there may be skin involvement characterized by peau d'orange (orange peel appearance).
- Advanced cases may exhibit frank ulceration and fixation to the chest wall.
- The term "cancer en cuirasse" is used when the disease progresses around the chest wall.
- Hard Lump:

Investigations for Breast Cancer
- Clinical Examination: Initial assessment involves a thorough clinical examination.
- Imaging:
- Chest Radiograph: A chest X-ray is performed to assess for any lung involvement.
- Computed Tomography (CT) of the Chest and Abdomen: CT scans of the chest and abdomen are conducted to evaluate the extent of disease spread.
- Bone Scan: A bone scan is employed to identify any metastasis to the bones.
- MRI (Magnetic Resonance Imaging): MRI is used to provide detailed images of breast tissue and adjacent structures.
- Whole-Body PET CT (Positron Emission Tomography-Computed Tomography): PET CT scans offer comprehensive information about the metabolic activity and spread of cancer throughout the body.
Breast carcinoma-Treatment
The fundamental objectives of treating breast cancer are to minimize the likelihood of local recurrence and mitigate the risk of metastatic dissemination.
In cases of early breast cancer, where the tumor is confined to the breast and has not spread to the lymph nodes, the primary treatment typically involves surgical intervention, possibly combined with radiotherapy.
Additional systemic therapies, such as chemotherapy or hormone therapy, may be introduced when there are unfavorable prognostic indicators, such as lymph node involvement, indicating a heightened probability of metastatic recurrence.
Conversely, for locally advanced or metastatic disease, the primary approach involves systemic therapy to alleviate symptoms, with surgery assuming a less prominent role in the treatment plan.
Algorithm for management of operable breast cancer
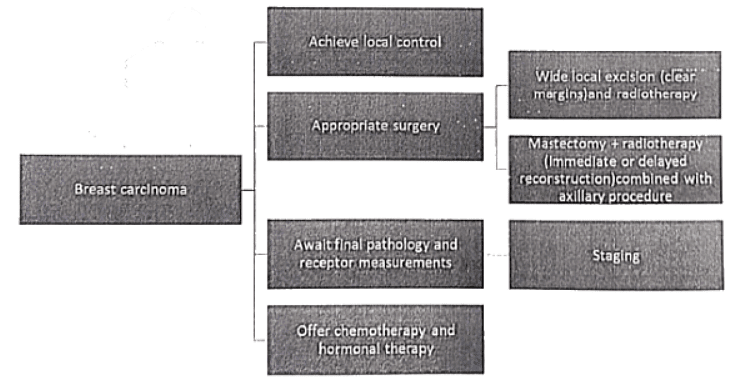
Breast carcinoma-Treatment
Mastectomy:
- Indications:
- Large tumors relative to breast size
- Central tumors beneath or involving the nipple
- Multifocal disease
- Local recurrence
- Patient preference
- Types of Mastectomy:
- Simple Mastectomy: Removal of the breast and axillary tail.
- Patey Mastectomy: Removal of the breast, axillary tail, and axillary lymph nodes (preferred).
- Halsted Radical Mastectomy: Removal of the breast, axillary tail, axillary lymph nodes, Pectoralis major, and minor (no longer indicated).
- Breast and Nipple Reconstruction:
- Immediate or delayed reconstruction options.
- Silicone gel implant under the pectoralis major muscle with acellular dermal matrix (ADM) for superior cosmetic results.
- In case of deficient skin, LD flap or TRAM/DIEP flap can be used.
- Conservative Breast Cancer Surgery:
- Options:
- Wide local excision (tumor + margin of normal breast tissue).
- Lumpectomy (excision of benign tumor + minimal breast tissue loss).
- Quadrantectomy (removal of the entire tumor segment).
- Axillary Staging:
- Presence of metastatic disease in axillary lymph nodes is a key prognostic marker.
- All patients require axillary staging.
- Sentinel node biopsy for clinically node-negative disease; further axillary dissection can be avoided if sentinel nodes are clear.
- Radiotherapy:
- Indications:
- Large tumors.
- Large numbers of positive nodes.
- Extensive lymphovascular invasion.
- Axillary surgery should not be combined with radiotherapy due to excess morbidity.
- Removal of internal mammary lymph nodes is unnecessary.
- Local excision without radiotherapy has a high local recurrence rate; involved margins require further excision or mastectomy before radiotherapy.
- Indications:
Adjuvant systemic therapy
Expected to delay relapse and prolong survival
Treatment of advanced breast carcinoma
Breast-Repeats
Q1: Discuss the pathogenesis and treatment of Breast Abscess. (1999)
Q2: Breast Conservation Therapy. (2007)
Q3: Enumerate the cystic lesions of the breast. How would you manage an 18 yrs. old girl presenting with 8x8 cm, tabulated, soft to firm lump in right breast without any lymphadenopathy? (2009)
Q4: How would you manage a 35-year-old lady with 2 x 2 cm carcinoma breast? (2010)
Q5: What are the possible contributing factors in pathogenesis of carcinoma breast? Describe briefly histopathology of different types of breast carcinoma. (2013)
Q6: What are various types and causes of nipple discharge in a female? How would you examine, investigate and treat a patient with large 6 cm breast tumor with mobile axillary lymph nodes in the axilla? (2013)
Q7: Discuss the causes of Benign Breast Disease, its investigation and management of bilateral fibroadenosis with mastalgia. (2017)
Q8: A 40-year-old lady presents in the OPD with complaint of right breast lump for the last one year which is slowly progressive. How will you evaluate this patient? Briefly outline the treatment of "early breast cancer." (2018)
|
7 videos|219 docs
|
FAQs on Breast - Medical Science Optional Notes for UPSC
| 1. What are the common causes of nipple discharge? |  |
| 2. What are cystic lesions of the breast? |  |
| 3. What are the clinical features of breast carcinoma? |  |
| 4. Can you provide an algorithm for the management of operable breast cancer? |  |
| 5. Is breast cancer recurrence common? |  |

|
Explore Courses for UPSC exam
|

|
















