Trigeminal Nerve: Neuroanatomy | Medical Science Optional Notes for UPSC PDF Download
Trigeminal Nerve

The trigeminal nerve originates from two roots emerging from the pons at its junction with the middle cerebellar peduncle. These two roots are:
(a) A large lateral sensory root
(b) A small medial motor root
Both roots extend forward and laterally over the apex of the petrous temporal bone to enter the middle cranial fossa. In this location, the sensory root displays an enlargement known as the trigeminal ganglion. This ganglion further divides into branches, namely the ophthalmic, maxillary, and mandibular branches.
The ophthalmic nerve progresses forward in the lateral wall of the cavernous sinus and then splits into three branches—lacrimal, frontal, and nasocilliary—before entering the orbit through the superior orbital fissure. Through these branches, the ophthalmic nerve provides innervation to the eyeball, conjunctiva, upper part of the nasal cavity, lacrimal gland, skin of the forehead, external nose, and eyelids.

The maxillary nerve exits the skull through the foramen rotundum, enters the pterygopalatine fossa, proceeds into the orbit through the inferior orbital fissure, and is then named the infraorbital nerve. Exiting the orbit through the infraorbital foramen, the infraorbital nerve becomes apparent on the face.
In summary, the maxillary nerve spans four regions: the middle cranial fossa, pterygopalatine fossa, orbit, and face. The branches of the maxillary nerve include:
- Meningeal branch in the middle cranial fossa
- Ganglion branches to the pterygopalatine ganglion
- Zygomatic nerve
- Posterior superior alveolar nerve in the pterygopalatine fossa
- Middle superior alveolar nerves in the orbit
- Palpebral, lateral nasal, and labial branches in the face.
Through these branches, it provides innervation to the nasal cavity, palate, upper teeth and gums, and the skin of the middle third of the face. The maxillary nerve also offers sensory supply to the mucous membrane of the nasopharynx and the maxillary sinus, while conveying secretomotor fibers to the lacrimal gland.
The mandibular nerve exits the skull via the foramen ovale, entering the infratemporal fossa. Just below the basal skull, it merges with the motor root of the trigeminal nerve. The motor root, accompanying the sensory root, passes deeply alongside the trigeminal ganglion, leaving the skull through the mandibular foramen to join the mandibular division of the trigeminal nerve, forming the trunk of the mandibular nerve.
This trunk of the mandibular nerve further divides into two large branches—anterior and posterior. The following branches arise from the mandibular nerve:
- Meningeal branch (nervus spinosus).
- Nerve to medial pterygoid from the undivided trunk.
- Masseteric nerve.
- Deep temporal nerves (2 in number).
- Lateral pterygoid nerve.
- Buccal nerve from the anterior division.
- Auriculotemporal nerve.
- Lingual nerve.
- Inferior alveolar nerve from the posterior division.

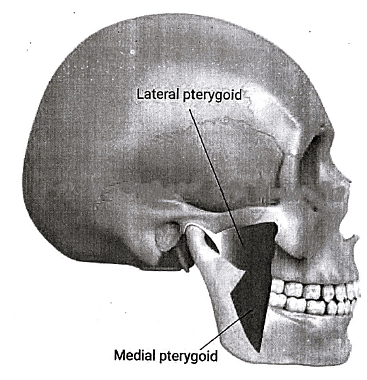
Through these branches, the mandibular nerve provides innervation to the muscles involved in mastication, including the temporalis, masseter, medial and lateral pterygoids. Additionally, it supplies the mylohyoid, anterior belly of the digastric, tensor veli palatine, and tensor tympani muscles.
The sensory fibers of the mandibular nerve offer sensory supply to the auricle, temporal region, and the skin of the lower one-third of the face, excluding the area over the angle of the mandible.
Trigeminal Nerve-Clinical anatom
1. Trigeminal nerve lesions manifest with the following clinical features:
- Diminished general sensation in the face and mucous membrane of the oral and nasal cavities.
- Absence of the corneal reflex.
- Flaccid paralysis of the muscles of mastication, leading to jaw deviation to the side of the lesion due to the unopposed action of the lateral pterygoid muscle.
- Hypoacusis, characterized by partial deafness to low-pitched sounds resulting from paralysis of the tensor tympani muscle.
2. Trigeminal neuralgia is characterized by paroxysmal, intense pain of sudden onset and brief duration within the cutaneous distribution area of one or more divisions of the trigeminal nerve, typically affecting the 2nd and 3rd divisions.
Each episode lasts from a few seconds to several minutes or hours, and these attacks can recur for hours with very short intervals between them.
|
7 videos|219 docs
|
FAQs on Trigeminal Nerve: Neuroanatomy - Medical Science Optional Notes for UPSC
| 1. What is the function of the trigeminal nerve? |  |
| 2. What are the three main branches of the trigeminal nerve? |  |
| 3. What are the common causes of trigeminal nerve disorders? |  |
| 4. What are the symptoms of trigeminal neuralgia? |  |
| 5. How is trigeminal neuralgia treated? |  |

|
Explore Courses for UPSC exam
|

|
















