Prolapse of uterus | Medical Science Optional Notes for UPSC PDF Download
| Table of contents |

|
| Uterine prolapse |

|
| Clinical presentation |

|
| Vault Prolapse |

|
| Prolapse of Uterus-Repeats |

|
DeLancey's levels of support of the genital organs


Etiology of Prolapse
Confirmed risk factors
- Older age
- Race
- Family history Increased body mass index
- Higher parity
- Vaginal delivery
- Constipation
Possible risk factors
- Intrapartum variables (macrosomia, long second stage of labour, episiotomy, epidural analgesia)
- Increased abdominal pressure
- Menopause
Degrees of Prolapse

- First degree-Descent of cervix into vagina
- Second degree-Descent of cervix to the introitus
- Third degree-Descent of cervix out side the introitus
- Procidentia-All of the uterus outside introitus
Uterine prolapse
Pelvic Organ Prolapse Quantification (POP-Q) system for staging pelvic organ prolapse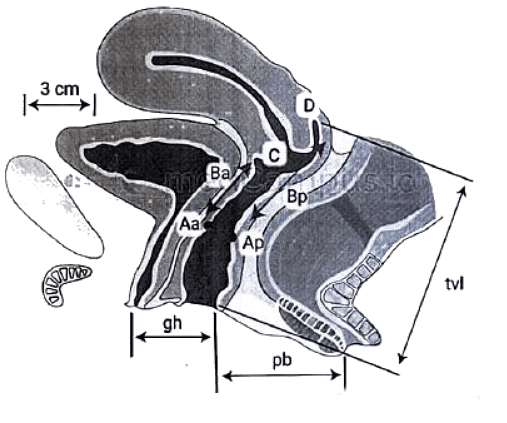
- Aa: Point A anterior
- Ap: Point A posterior
- Ba: Point B anterior
- Bp: Point B posterior
- C:, Cervix or vaginal cuff
- D: Posterior fornix (if cervix is present)
- gh: Genital hiatus
- pb: Perineal body
- tvl: Total vaginal length.
Quantification of prolapse is lately described by the International Continence Society, and is objective and site-specific. The hymen is taken as a fixed point (0). Six reference points are measured, using scaled spatula, and tabulated in a grid The points above the hymen are described as minus and points below as plus.
Staging of POP
- Stage 0-No demonstrable prolapse
- Stage 1-All points, -1
- Stage 2-Lowest point within 1 cm of hymen (between -1 and +1)
- Stage 3-Lowest point >1 cm below hymen but not complete prolapse
- Stage 4-Complete prolapse with lowest point equal to TVL-2
Clinical presentation
Vaginal symptoms
- Sensation of a bulge or protrusion
- Seeing or feeling a bulge
- Pressure
- Heaviness
Urinary symptoms
- Incontinence, frequency, or urgency
- Weak or prolonged urinary stream
- Feeling of incomplete emptying
- Manual reduction of prolapse needed to start or complete voiding ("digitation")
- Change of position needed to start or complete voiding
Bowel symptoms
- Incontinence of flatus, or liquid or solid stool
- Feeling of incomplete emptying
- Straining during defecation
- Digital evacuation needed to complete defecation
- Splinting (pushing on or around the vagina or perineum) needed to start or complete defecation ("digitation")
Sexual symptoms
- Dyspareunia (painful or difficult intercourse)
- Lack of sensation
Signs/Physical examination
- Patient is made to cough and strain, and the nature and degree of prolapse noted. Make a note of stress incontinence if any
- Vulva is examined for perineal lacerations
- Perineal body and levator muscles are palpated to determine the muscle tone.
- Speculum examination is done
- Cervical cytology is obtained
- Evaluate general condition of the patient to decide on her fitness for surgery
Differential diagnosis
- Vulval cyst
- Cyst of anterior vaginal wall
- Urethral diverticula
- Congenital elongation of cervix
- Cervical fibroid polyps
- Chronic inverison of uterus
- Rectal prolapse
Investigations
- Haemoglobin
- Urine examination
- Blood urea,
- Blood sugar,
- X-ray chest
- ECG
- Urine culture
- High vaginal swab in cases of vaginitis
- IVP will reveal ureteric obstruction in major prolapse.
- Ultrasound and MRI localize the defects in the supporting structures and help in surgery
- Transperineal and vaginal ultrasound reveal defect in the levator ani muscles and lateral supports, whereas transrectal ultrasound is useful to confirm enterocele.
Management
- Vaginal hysterectomy with pelvic floor repair- is suitable for women over the age of 40 years, those who have completed their families, and are no longer keen on retaining their childbearing and menstrual functions. The age limit may be relaxed to 35 years for women who have additional menstrual problems, or the uterus is a seat of fibroids, adenomyosis.
- Le Fort's repair is reserved for the very elderly menopausal patient with an advanced prolapse, or for those women who are poor medical risks and are considered unfit for any major surgical procedure.
- Abdominal sling operations have been designed for young women suffering from second or third degree uterine prolapse, and who are desirous of retaining their childbearing and menstrual functions
- Fothergills repair/Manchester operation-lt is suitable for women under 40 years who are desirous of retaining their menstrual and reproductive functions.

Prophylaxis of Prolapse
Discuss the prophylaxis of genital prolapse?
Careful attention during childbirth can do much to prevent prolapse.

Vault Prolapse
A 60-year-old woman presents with something coming out per vagina following abdominal hysterectomy 2 years ago. How will you manage the case?
Diagnosis-Vault prolapse
Risk factors
- Post abdominal and vaginal hysterectomy
- Failure to identify and repair an enterocoele during hysterectomy
- Technical error in previous surgery
- Age
- Menopause (Estrogen deficiency)
- Multiparity
- Obesity
- Chronic cough
Presentation
- Coital difficulty
- Difficulty in walking
- Backache
- Urinary and rectal symptoms
Degrees of Vault Prolapse
- First degree—The vaginal apex is visible at the introitus.
- Second degree—The vault protrudes through the introitus.
- Third degree—The entire vagina is outside the introitus.
Treatment-Surgical procedures (Vaginal/Abdominal Sling surgery)
Sacrocolpopexy is considered the gold standard surgical procedure for vault prolapse Note-Vaeinal route is safer for elderly women. Abdominal surgery in young women avoids dvspareunia.
Other surgical procedures and their indications
Prolapse of Uterus-Repeats
Q1: Write down etiology of uterine prolapse. Briefly describe the supports of the uterus. What are symptoms, signs and management of 3rd degree uterine prolapse in a woman of 42-years age, who has completed her family? (2011)
Q2: Define prolapse of uterus. Enumerate different degrees of prolapse of uterus. Enumerate the factors leading to prolapse of uterus. How would you manage the case of 3rd degree uterovaginal prolapse in a 38-year-old woman who has completed her family? (2017)
|
7 videos|219 docs
|
FAQs on Prolapse of uterus - Medical Science Optional Notes for UPSC
| 1. What is uterine prolapse? |  |
| 2. What are the common symptoms of uterine prolapse? |  |
| 3. How is uterine prolapse diagnosed? |  |
| 4. What are the treatment options for uterine prolapse? |  |
| 5. Can uterine prolapse be prevented? |  |

|
Explore Courses for UPSC exam
|

|

















