Nutritional Problems in Public Health | Medical Science Optional Notes for UPSC PDF Download
| Table of contents |

|
| Low Birth Weight |

|
| Undernutrition |

|
| Iodine Deficiency Disorders |

|
| NNAPP-National Nutritional Anemia Prophylaxis |

|
Low Birth Weight
- A low birth weight (LBW) infant is defined as one whose birth weight is less than 2.5 kg.
- A very low birth weight (VLBW) infant is characterized by a birth weight less than 1.5 kg, often associated with prematurity (gestational age less than 37 weeks).
- An extremely low birth weight (ELBW) infant is identified by a birth weight below 1 kg.
Low birth weight babies fall into two primary categories:
- Those born prematurely (with a short gestation period).
- Those experiencing fetal growth retardation.
Problem Statement
According to the Rapid Survey on Children 2014, approximately 18.6 percent of infants born in India have a low birth weight.
Contributing factors:
- Maternal malnutrition
- Maternal anemia
- Engaging in strenuous physical labor during pregnancy
- Infections contracted during pregnancy
- Short maternal stature
- Early maternal age
- High parity
- Smoking
- Close birth intervals
Low Birth Weight-Preventive measures
Low birth weight (LBW) stands out as a significant hurdle in maternal and child health, impacting both developed and developing nations. Given the multitude of contributing factors, there is no universally applicable solution to completely eradicate the LBW rate.
Priority should be directed towards comprehensive prenatal care and intervention programs, emphasizing prevention rather than the treatment of LBW infants after birth.
Identify pregnancies at high risk and mitigate the associated risks through appropriate measures. Factors contributing to heightened risk include:
- Maternal malnutrition
- Excessive workload
- Presence of diseases and infections
- Elevated blood pressure
- Experiencing pregnancies at too frequent intervals
Direct interventions include
Specific interventions comprise:
- Employing Mother Health Cards
- Augmenting dietary intake
- Providing supplementary feeding
- Dispensing iron and folic acid tablets
- Fortifying and enriching food items
- Managing infections (e.g., malaria, urinary tract infections, TORCHES)
- Promptly identifying and treating medical disorders (such as hypertension, toxemias, and diabetes)
Indirect interventions include
- Family planning
- Avoidance of smoking
- Improved sanitation measures
- Improve health and nutrition of young girls
- Government support with fully paid maternity leave and child benefits
Undernutrition
Undernutrition is characterized by insufficient intake, inefficient absorption, or excessive loss of nutrients.
Indicators of Undernutiition
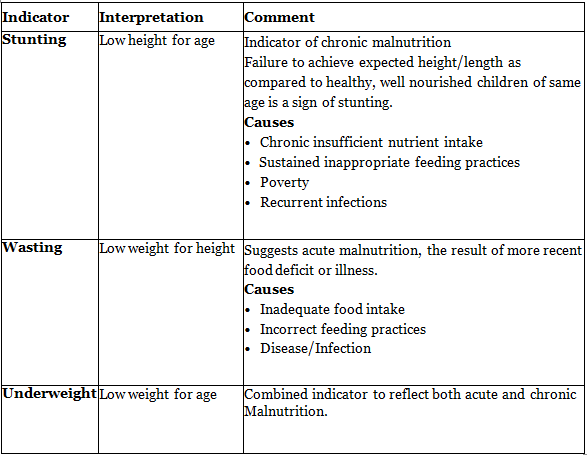
Preventive measures of Undernutrition (8lh FAO/WHO Expert committee on nutrition)
Health promotion:
- Initiatives targeting pregnant and lactating women, such as education and supplement distribution.
- Advocacy for breastfeeding.
- Creation of affordable weaning foods: encouraging frequent and increased food intake for children.
- Strategies to enhance family diets.
- Nutrition education with a focus on promoting proper feeding practices.
- Implementation of home economics programs.
- Emphasis on family planning and birth spacing.
- Consideration of the family environment.
Specific Protection:
- Ensuring the child's diet includes protein- and energy-rich foods, with an emphasis on items like milk, eggs, and fresh fruits if possible.
- Immunization efforts.
- Food fortification initiatives.
Early Diagnosis and Treatment:
- Regular surveillance.
- Prompt identification of any growth delays.
- Early diagnosis and treatment of infections and diarrhea.
- Implementation of programs for the early rehydration of children with diarrhea.
- Establishment of supplementary feeding programs during epidemics.
- Deworming of heavily infested children.
Rehabilitation:
- Provision of nutritional rehabilitation services.
- Hospital-based treatment.
- Follow-up care.
Low Birth Weight - Repeats
- In reference to pediatric nutrition, define the term "Stunting". What is indicative of? What are its causes? (2019)
- Define "Low Birth Weight" (LBW). Enumerate the public health measures that can help reduce the burden of LBW babies in the community. (2019)
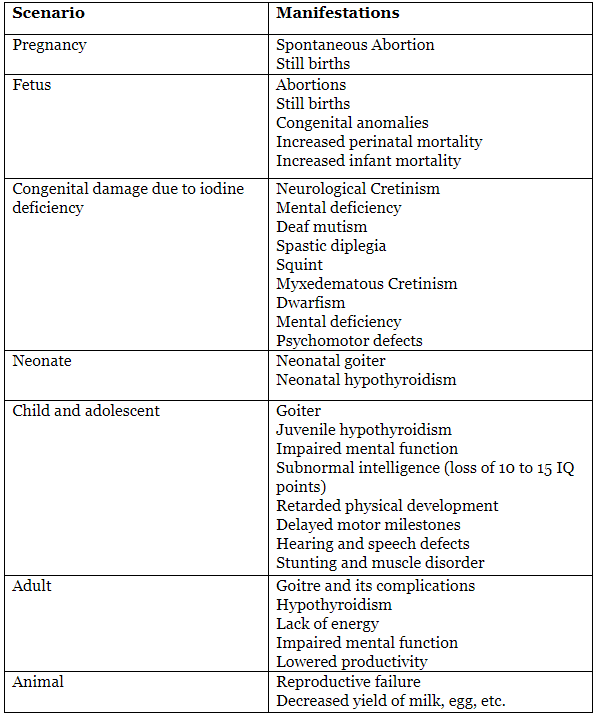
Iodine Deficiency Disorders
Iodine
Iodine plays a crucial role as a component of the thyroxine hormone, facilitating the body's oxidation processes and regulating metabolism. All biological functions of iodide are ascribed to thyroid hormones.
These thyroid hormones, in turn, play a pivotal role in the growth and development of the human brain and central nervous system from the 15th week of gestation to 3 years of age. The iodine content in food is contingent on the iodine levels in the soil where it is cultivated.
In 2001, the World Health Organization, in collaboration with UNICEF, issued dietary intake recommendations for iodine as follows:
- Infants: A recommended iodine intake of 90 µg/day from birth onward.
- For children aged 1 to 10 years, the suggested range is 90 to 120 µg/day.
- Adolescents and adults require approximately 150 µg/day.
Sources of iodine include sea fish, freshwater fish, vegetables, and cereals, among other foods.
Due to insufficient iodine intake from food, leading to low iodine levels in the thyroid gland, the gland responds by enlarging itself to produce adequate amounts of T3 and T4. This enlargement is referred to as a goiter.
Iodine deficiency is recognized as the foremost preventable cause of brain damage and mental retardation worldwide. In India, this deficiency is endemic in the sub-Himalayan regions, spanning approximately 2400 km from Kashmir to NEFA, including the northern districts of Punjab, UP, Bihar, and West Bengal.
Coined by Hetzel in 1983, the term Iodine Deficiency Disorders (IDD) encompasses the collective clinical and subclinical manifestations of iodine deficiency.
Causes of iodine deficiency in India include:
- Limited availability and high cost of seafood.
- Environmental iodine deficiency in the soil.
- Consumption of goitrogenic foods such as rapeseed, mustard, yellow turnip, cabbage, maize, sweet potatoes, and groundnut skin.
National IDD Control Programme
World Iodine Deficiency Disorders Prevention Day is observed on October 21st, underscoring the importance of incorporating iodized salt into daily consumption.

Measures taken by GOI under National IDO program
- Prohibition of the sale of non-iodized salt.
- Iodine concentration in salt during manufacturing not to be less than 30 ppm.
- Iodine concentration in salt at the retail level not to be less than 15 ppm.
- Inclusion of a smiling sun imprint to aid illiterate individuals in recognizing iodized salt.
- The Central Government allocates funds for health education and promotional campaigns to encourage the consumption of iodized salt.
- The Central Government also allocates financial support for the establishment of Iodine Deficiency Disorders (IDD) Control Cells in State Health Directorates.
- A National Reference Laboratory overseeing IDD has been established at the biochemistry division of the National Institute of Communicable Diseases in Delhi. It monitors the iodine levels in salt and urine, with an allocation of Rs 75,000 per district laboratory for this purpose.
National IDD control program-Monitoring:
The International Council for the Control of Iodine Deficiency Disorders (ICCIDD), along with the World Health Organization (WHO) and UNICEF, advocates monitoring the advancement of Iodine Deficiency Disorders (IDD) programs in any country through the use of measurable indicators.
The indicators encompass:
(i) Percentage of households using adequately iodized salt (>90%);
(ii) Urinary iodine excretion: proportion below 100 mcg/lt (<50%) and proportion below 50 mcg/lt (<20%); and
(iii) Thyroid size: percentage of school children aged 6-12 years with enlarged thyroid, assessed through palpation or ultrasound (<5%).
IDD-Repeats
- Discuss briefly iodine deficiency disorders (2009).
NNAPP-National Nutritional Anemia Prophylaxis
Definition
The World Health Organization (WHO) defines nutritional anemia as "a condition in which the hemoglobin content of blood is lower than normal due to a deficiency of one or more essential nutrients, irrespective of the underlying cause of such deficiency."
Problem Statement:Studies on the prevalence of nutritional anemia in India indicate that 65% of infants and toddlers, 60% of children aged 1-6 years, approximately 88% of adolescent girls (with 3.3% experiencing severe anemia, defined as hemoglobin <7 gm/dl), and 85% of pregnant women (with 9.9% having severe anemia) are affected. The prevalence of anemia is slightly higher in lactating women compared to pregnant women, with iron deficiency anemia being the most common.
To address nutritional anemia among mothers and children (1-12 years), the Government of India initiated the National Nutritional Anemia Prophylaxis Programme during the Fourth Five-Year Plan. New recommendations, post the eleventh five-year plan, advocate the inclusion of infants aged 6-12 months and individuals aged 11-18 years in the National Nutritional Anemia Prophylaxis Programme (NNAPP). The program, now part of the Reproductive and Child Health (RCH) initiative, is managed by the Maternal and Child Health (MCH) Division of the Ministry of Health and Family Welfare.
The program focuses on daily supplementation with iron and folic acid tablets to prevent mild and moderate cases of anemia. The targeted beneficiaries are individuals in "at-risk" groups, including pregnant women, lactating mothers, and those in the age group of 6 months to 18 years.
Eligibility Criteria:
The eligibility for participation is determined based on the patients' hemoglobin levels. If the hemoglobin falls between 10 and 12, a daily supplement of iron and folic acid tablets is recommended. If it is below 10 g, the patient is directed to the nearest primary health center.
Dosage:
The dosage recommendations stem from an extensive process that began with consultations on anemia in adolescent girls, leading to the National Consultation on Micronutrients in late 2003 with ICMR/MHFW. Subsequent collaboration with the committee chaired by DG ICMR, engagement with NRHM, and work with various groups on the 11th five-year plan have contributed to the formulation. Key points include:
For Mothers:
- The current program advises continuing recommendations for pregnant and lactating women.
- A daily administration of one tablet containing 60 mg of elemental iron (equivalent to 180 mg of ferrous sulfate) and 0.5 mg of folic acid is recommended.
- Administration should continue until 2 to 3 months after the normalization of hemoglobin levels to replenish iron stores.
- Regular hemoglobin estimation is essential at 3-4 month intervals.
- The duration of supplementation depends on the progress of the beneficiary.
For Children:
- In case of suspected anemia, screening tests may be conducted on infants at 6 months, 1 year, and 2 years.
- Children aged 6 months to 60 months should be given a daily supplement of 20 mg elemental iron and 100 mcg folic acid, considering this regimen as both safe and effective. Ferrous sulfate and folic acid should be provided in a liquid formulation containing 20 mg elemental iron and 100 mcg folic acid per ml, dispensed in bottles for safety reasons.
- Children aged 6-10 years will receive 30 mg elemental iron and 250 mcg folic acid per day for 100 days in a year.
- Adolescents aged 11-18 years will be supplemented at the same doses and duration as adults, with priority given to adolescent girls.
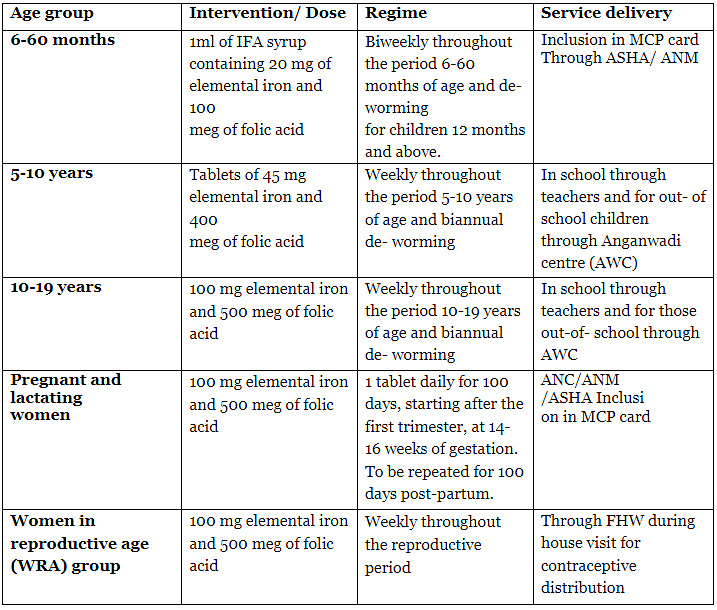
NIPI-National Iron Plus Initiative
In 2013, the Ministry of Health and Family Welfare initiated the "National Iron Plus Initiative" as a comprehensive strategy to address the public health challenge of Iron Deficiency Anemia prevalent throughout the life cycle. The initiative includes age-specific interventions involving Iron and Folic Acid Supplementation and Deworming to enhance hemoglobin levels and diminish the prevalence of anemia across various age groups, namely children aged 6-59 months, 5-10 years, adolescent girls and boys (11-19 years), pregnant and lactating women, and women in the reproductive age group (20-49 years).
Within the framework of the National Iron Plus Initiative, the following age groups are included for lifelong iron supplementation starting from the age of 6 months:
WIFS Programme
Adolescent Weekly Iron and Folic Acid Supplementation (WIFS) Program:
- Also recognized as the WIFS-Blue campaign.
- Oversight by the Ministry of Health and Family Welfare (H&FW).

Target Beneficiaries:
- Adolescent girls/boys attending school, from 6th to 12th grade (Ministry of Education).
- Adolescent girls not attending schools (Ministry of Social Welfare).
Provided Services:
- Distribution of Iron and Folic Acid (IFA) tablets to the target population every week on a designated day (Monday) throughout 52 weeks.
- Biannual deworming sessions scheduled for February and August.
MCP card (Mother and child protection card)
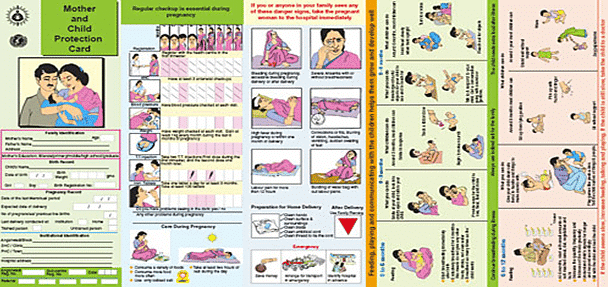
The Mother and Child Protection Card (MCP Card) is the result of collaborative efforts between the Ministry of Women and Child Development and the Ministry of Health & Family Welfare, Government of India. This card serves as an educational tool, guiding mothers and families on various aspects of maternal and child care. It seamlessly integrates maternal and child health into a continuous care approach, aligning with the Integrated Child Development Services (ICDS) scheme of the Ministry of Women and Child Development and the National Rural Health Mission (NRHM) of the Ministry of Health & Family Welfare (MoHFW).
The MCP card not only informs and educates but also documents key services provided during Antenatal, Intranatal, and Postnatal care to ensure the delivery of the minimum package of services to the beneficiaries. It plays a crucial role in the timely identification, referral, and management of complications during pregnancy, childbirth, and the postnatal period. Additionally, the card facilitates the complete immunization of infants and children, encourages early and exclusive breastfeeding, promotes complementary feeding, and monitors their growth.
Key points about the Mother and Child Protection Card:
- Developed as a tool for families to learn, comprehend, and adopt positive practices for the overall health of pregnant women, young mothers, and children.
- Informs families about the various types of services necessary for the health and well-being of women and children.
- Empowers families to make decisions for the continuous improvement of health, nutritional status, and the development of young children.
Specific Target Groups for the MCP Card:
- Pregnant women
- Families with children under 3 years of age
Card Custodians:
- Pregnant women
- Mothers of children under 3 years of age
The Auxiliary Nurse Midwife (ANM) / Anganwadi Worker (AWW) is responsible for recording the relevant information in the designated spaces on the card.
The Anemia Mukt Bharat- intensified Iron-plus Initiative (POSHAN ABHIYAN)
The Anemia Mukt Bharat - Intensified Iron-plus Initiative seeks to enhance existing mechanisms and introduce new strategies to address anemia. It specifically targets six beneficiary groups, employs six interventions, and utilizes six institutional mechanisms to meet the objectives outlined in the POSHAN Abhiyan.
Reducing anemia is a key goal of the POSHAN Abhiyaan, initiated in March 2018. In alignment with the targets of the POSHAN Abhiyaan and the National Nutrition Strategy outlined by NITI Aayog, the Anemia Mukt Bharat strategy is designed to annually decrease the prevalence of anemia by 3 percentage points among children, adolescents, and women in the reproductive age group (15-49 years) from 2018 to 2022.
 Six Interventions
Six Interventions
The Anemia Mukt Bharat strategy is a comprehensive approach that targets various interventions, including:
Prophylactic Iron and Folic Acid supplementation: Administered to children, adolescents, women of reproductive age, and pregnant women.
Deworming: Utilizing Albendazole 400 mg.
An intensified year-round Behaviour Change Communication Campaign (Solid Body, Smart Mind): Focused on promoting four key behaviors, namely improving compliance with Iron Folic Acid supplementation and deworming, adopting appropriate infant and young child feeding practices, increasing intake of iron-rich foods through diet diversity, quantity, frequency, and/or fortified foods, with an emphasis on utilizing locally available resources.
Ensuring delayed cord clamping after delivery (by 3 minutes) in health facilities.
Testing and treatment of anemia: Employing digital methods and point-of-care treatment, with a special focus on pregnant women and school-going adolescents.
Mandatory provision of Iron and Folic Acid fortified foods in government-funded public health programs.
Intensifying awareness, screening, and treatment of non-nutritional causes of anemia in endemic areas, with a particular focus on malaria and hemoglobinopathies.
Nutritional Anemia-Repeats
- Describe the problem of nutritional anemia in India. Describe the National Nutritional Anemia Prophylaxis Programme. (2010)
- As per the National Family Health Survey-4, how grave is the situation in India with regard to Nutritional Anemia. Give statistics substantiating your statement. Under the "National lron+ Initiative", which are the specific groups being specially targeted? What specific interventions are being employed for different target groups under the National lron+ Initiative? What are the mechanisms of service delivery being employed implement the National lron+ Initiative? (2018)
|
7 videos|219 docs
|
FAQs on Nutritional Problems in Public Health - Medical Science Optional Notes for UPSC
| 1. What is low birth weight? |  |
| 2. What are the consequences of low birth weight? |  |
| 3. What is undernutrition? |  |
| 4. What are Iodine Deficiency Disorders (IDD)? |  |
| 5. What is NNAPP (National Nutritional Anemia Prophylaxis)? |  |

|
Explore Courses for UPSC exam
|

|

















