Antigen, Antibody, Antigen-Antibody Reaction, Complement Chapter Notes | Microbiology - NEET PG PDF Download
| Table of contents |

|
| Antigen |

|
| Antibody |

|
| Antigen-Antibody Reactions |

|
| Types of Antigen-Antibody Reactions |

|
| Modern Techniques for Detecting Antigen-Antibody Reactions |

|
| What is Complement? |

|
Antigen
Antigens are substances that play a crucial role in triggering immune responses in the body. They possess two specific properties: Immunogenicity and Antigenicity.
- Immunogenicity refers to the ability of an antigen to provoke an immune response, leading to the activation of B-cells and T-cells.
- Antigenicity, on the other hand, is the capacity of an antigen to bind specifically with the products of the immune response, such as antibodies or T-cell receptors.
It is important to note that while all molecules capable of triggering an immune response possess antigenicity, not all antigenic molecules can initiate an immune response.
For instance, haptens are antigenic but lack immunogenicity unless they are attached to a larger protein.
Epitope
- An epitope, also known as an antigenic determinant, is the smallest portion of an antigen that can activate T-cells and B-cells, interacting with specific T-cell receptors or antibodies.
- The part of an antibody that binds to an epitope is called a paratope.
- Epitopes can be categorised into two types:
- Sequential (linear) epitopes are a straight sequence of a few amino acids.
- Conformational (non-sequential) epitopes are found in the flexible parts of complex antigens with a three-dimensional structure.
- Generally, T-cells recognise sequential epitopes, while B-cells bind to conformational ones.
Haptens
- Haptens are small molecules that lack immunogenicity, meaning they cannot trigger an immune response on their own. However, they retain antigenicity, which allows them to bind to specific antibodies or T-cell receptors.
- Haptens can become immunogenic when they combine with a larger protein known as a carrier.
- This hapten-carrier complex can produce antibodies specific to:
- The epitopes of the hapten.
- The unchanged epitopes on the carrier protein.
- New epitopes that arise from the combination of both the hapten and carrier.
- Haptens can be classified into:
- Complex haptens, which have multiple epitopes, can react with specific antibodies, and their hapten-antibody complex can be detected through methods like precipitation reactions.
- Simple haptens, usually having only one epitope (univalent), can bind to antibodies, but their hapten-antibody complex cannot be detected since precipitation requires at least two epitopes.
Factors Affecting Immunogenicity
Various factors can influence how effectively an antigen provokes an immune response:
- Size of the Antigen: Larger antigens, such as hemoglobin, are generally more immunogenic.
- Chemical Nature: Proteins are more potent immunogens compared to carbohydrates, lipids, and nucleic acids.
- Susceptibility to Tissue Enzymes: Antigens that are susceptible to tissue enzymes may have increased immunogenicity by exposing more epitopes.
- Structural Complexity: Antigens with more complex structures tend to have enhanced immunogenicity.
- Foreignness: The greater the foreignness of the antigen to the host, the higher its immunogenicity.
- Genetic Factors: An individual’s genetic makeup can impact the immune response to an antigen.
- Optimal Dose: The right amount of antigen is crucial; too little may not elicit a response, while too much can lead to immune paralysis.
- Route of Administration: The method of delivering the antigen can affect its immunogenicity.
- Repeated Doses: Administering antigens multiple times can influence the immune response.
- Multiple Antigens: The presence of multiple antigens can either reduce or enhance each other’s immunogenicity due to competition or synergistic effects.
- Heterophile Nature: This concept involves antigens that share similar epitopes, allowing cross-reactivity of antibodies.
- Adjuvants: Substances that enhance the immunogenicity of an antigen, often added to vaccines to improve their effectiveness.
Adjuvants
Adjuvants are substances that enhance the immunogenicity of an antigen, making them more effective in provoking an immune response. They are commonly added to vaccines to improve their efficacy.
Examples of adjuvants include:
- Alum: Aluminium hydroxide or phosphate, often used in vaccines to boost the immune response.
- Mineral Oil: Such as liquid paraffin, used in some vaccine formulations.
- Freund’s Incomplete Adjuvant: water-in-oil emulsion containing antigen in the aqueous phase, used to enhance immune responses.
- Freund’s Complete Adjuvant: mix of Freund’s incomplete adjuvant and killed tubercle bacilli in the oil phase, used in research and clinical settings.
- LPS from Bordetella pertussis: Lipopolysaccharides from this bacterium act as excellent adjuvants for diphtheria and tetanus toxoids.
- Other Bacteria or Their Products:
- Mycobacterium bovis
- Toxoids, such as Diphtheria (DT) and Tetanus (TT) toxoids, which act as adjuvants for the Haemophilus influenzae type b vaccine.
- Non-Bacterial Products: Such as silica particles, beryllium sulfate, squalene, and thimerosal, which can also serve as adjuvants.
Heterophile Antigens
Heterophile antigens are characterized by their shared epitopes, meaning that antibodies generated against an antigen from one species can cross-react with similar antigens from another species. This phenomenon is utilized in various diagnostic tests:
- Weil–Felix Reaction: This test is used to diagnose typhus fever by detecting antibodies against rickettsial antigens that cross-react with Proteus antigens.
- Paul-Bunnell Test: Conducted for infectious mononucleosis caused by Epstein-Barr virus (EBV), this test uses sheep red blood cell antigens to identify cross-reacting antibodies in patient sera.
- Cold Agglutination Test and Streptococcus MG Test: These tests are employed for primary atypical pneumonia by detecting antibodies against Mycoplasma pneumoniae using human O blood group red blood cells and Streptococcus MG antigens, respectively.
- Forssman Antigen: This is a universal heterophile antigen found in various organisms, including animals, plants, and bacteria, but it is absent in rabbits.
Biological Classes of Antigens
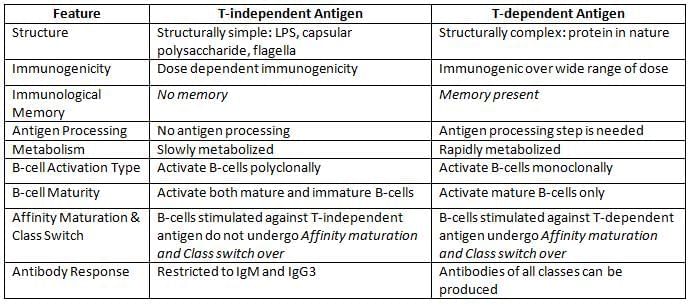
Antigens can be classified into two main categories based on their ability to trigger antibody production: T-cell dependent (TD) and T-cell independent (TI) antigens.
- T-dependent (TD) Antigens: Most common antigens fall under the category of T-cell dependent antigens. These antigens are processed and presented to T-cells by specialized immune cells known as antigen presenting cells (APCs). Once the T-cells are activated, they release signaling molecules called cytokines, which in turn stimulate B-cells to produce antibodies.
- T-Independent (TI) Antigens: There are a few antigens such as bacterial capsule, flagella and LPS that do not need the help of T-cells and APCs. They directly bind to Ig receptors present on B-cells and stimulate B-cells polyclonally leading to hypergammaglobulinemia.
Superantigens
- Superantigens are a special type of antigen that can activate T cells directly, without the need for antigen-presenting cells (APCs).
- They bind to the variable β region of the T-cell receptor (TCR), creating a non-specific connection between the MHC-II of APCs and T cells.
Examples of Superantigens
1. Bacterial Superantigens:
- Staphylococcal Toxins: Including Toxic Shock Syndrome Toxin (TSST), Exfoliative Toxin, and various Enterotoxins.
- Streptococcal Toxins: Such as Streptococcal Pyrogenic Exotoxin (SPE)-A and SPE-C.
- Mycoplasma arthritidis Mitogen-I
- Yersinia enterocolitica
- Yersinia pseudotuberculosis
2. Viral Superantigens:
- Epstein-Barr Virus (EBV)
- Cytomegalovirus (CMV)
- Rabies Nucleocapsid
- HIV-encoded Nef (Negative Regulatory Factor)
3. Fungal Superantigen:
- Malassezia furfur
Antibody
Structure of Immunoglobulins
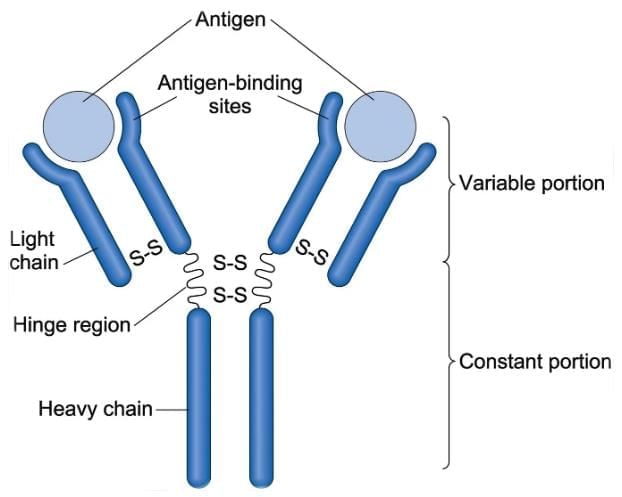
- Antibodies, also known as immunoglobulins, have a Y-shaped structure made up of four polypeptide chains:
- Two light (L) chains
- Two heavy (H) chains
- All four chains are connected through disulfide bonds and other non-covalent interactions, including:
- Salt linkages
- Hydrogen bonds
- Hydrophobic bonds
- Each chain has two ends:
- Amino-terminal end (NH3)
- Carboxyl-terminal end (COOH)
- There are five classes of heavy chains:
- Gamma (γ)
- Alpha (α)
- Mu (μ)
- Delta (δ)
- Epsilon (ε)
- There are two classes of light chains:
- Kappa (κ)
- Lambda (λ)
- Each antibody contains:
- Only one type of light chain
- Only one type of heavy chain
- Based on the constant region of the heavy chains, antibodies are classified into five types:
- IgG
- IgA
- IgM
- IgD
- IgE
- Each heavy and light chain has:
- A variable region
- A constant region
- The variable region contains areas called hypervariable regions or complementarity determining regions that have higher variability:
- There are three hot spots in the light chain
- There are four hot spots in the heavy chain
- The paratope is the specific site on the hypervariable regions that interacts with the epitope of an antigen.
- The hinge region:
- Is the joint between the constant regions of heavy chains in IgG, IgA, and IgD
- Is absent in IgE and IgM
- Contains a lot of proline and cysteine
- This area is flexible, helping the antibody to reach the antigen
- Regarding enzymatic digestion:
- Papain digestion: This enzyme cuts the antibody above the hinge region, resulting in:
- Two Fab fragments (antigen-binding fragments)
- One Fc fragment (crystallizable fragment)
- Pepsin digestion: This enzyme cuts below the hinge region, leading to:
- One F(ab')2 fragment
- Many smaller fragments
- Mercaptoethanol digestion: This method produces four fragments (two heavy and two light chains) by only breaking the disulfide bonds, without affecting the peptide bonds.
- Papain digestion: This enzyme cuts the antibody above the hinge region, resulting in:
- The chains of immunoglobulins are coded by different chromosomes:
- Heavy chains are coded by chromosome 14
- Kappa light chains are coded by chromosome 2
- Lambda light chains are coded by chromosome 22
- After the chains are made, a process called germ line recombination (or rearrangement) occurs.
Functions of Immunoglobulins
- Antigen Binding: The Fab region of immunoglobulins binds to specific antigens.
- Effector Functions:These are carried out by the Fc region of immunoglobulins.
- Fixation of Complement: The antibody-coated target cell binds to complement through its Fc receptor, leading to complement-mediated target cell lysis.
- Binding to Various Cell Types: Phagocytic cells, lymphocytes, platelets, mast cells, NK cells, eosinophils, and basophils have Fc receptors (FcR) that attach to the Fc region of immunoglobulins.
Properties of Various Immunoglobulins
- IgG Antibody:
- IgG is highest for DHS (decreasing order for DHS is—GAMDE i.e. highest is IgG and lowest IgE):
- Daily production,
- Half life (23 days),
- Serum concentration
- Four subtypes: IgG1-4 (Decreasing order for DHS is IgG 1 > IgG 2 > IgG 3 > IgG 4)○ IgG is Responsible for:
- Precipitation,
- Neutralization,
- NK cell binding (to perform ADCC)
- Classical complement binding (IgM > IgG 3 > IgG 1 > IgG 2) (IgG 4 does not fix complement)
- Coagglutination by binding to S.aureus protein A (Except IgG 3)
- Opsonization
- IgG appears late, so indicates past/chronic infection
- IgG avidity increases with time – So, detection of less avidity IgG indicates relatively recent infection
- Secreted in placenta (Maximum placental transfer IgG 1, minimum IgG 2)
- Secreted in breast milk
- Helps in phagocytosis by binding to FcR on phagocytes (Except IgG 2)
- IgE Antibody:
- Characteristics: Only heat-labile antibody, lowest for DHS.
- Functions: Responsible for type I hypersensitivity reactions, homocytotropic (species-specific) antibody, also known as reagin antibody, raised in helminthic infections.
- IgA Antibody:
- Abundance and Types: Second most abundant antibody (second highest for DHS), with serum IgA predominantly in monomeric form and secretory IgA (SIgA) in dimeric form (valency four) joined by a J chain and secretory component.
- Functions: SIgA responsible for mucosal/local immunity, IgA existing in two subclasses (IgA1 and IgA2) with predominance in serum and secretions.
- IgD Antibody:
- Functions: Surface immunoglobulin on B-cells, highest carbohydrate content.
- IgM Antibody:
- Characteristics: Highest antibody for MIS (molecular weight, intravascular distribution, sedimentation coefficient), pentameric nature with 10 valency, acting as surface immunoglobulin on B-cells, first antibody to appear after infection and in intrauterine life (20 weeks) indicating congenital infection.
- Functions: Agglutination, hemolysis, opsonization (examples include antibodies in typhoid, reagin antibody in syphilis, natural antibodies in ABO and Rh system).
Abnormal Immunoglobulin:
- Bence Jones Proteins: Produced in multiple myeloma (light chain disease) where excess light chains coagulate at 50°C and redissolve at 70°C.
- Waldenström’s Macroglobulinemia: lymphoma affecting B-cells producing excess IgM, with somatic mutations in the MYD88 gene in over 90% of patients.
- Heavy Chain Disease: Characterised by excessive production of short and truncated heavy chains, with four types based on the heavy chain involved: alpha, gamma, mu, and delta chain disease.
- Cryoglobulinemia: condition where blood contains cryoglobulins, a type of Ig that becomes insoluble at low temperatures but redissolves when heated, usually consisting of IgM directed against the Fc region of IgG.
Ig Specificity or Antigenic Determinants of Ig
Isotypes
- The five classes of immunoglobulins are IgG, IgA, IgM, IgD, and IgE.
- These classes are known as isotypes.
- They differ in the amino acid sequences of the constant region of their heavy chains.
- This difference is referred to as isotypic variation.
Idiotypes
- The unique amino acid sequence in the paratope region (in VH and VL regions) of one member acts as an antigenic determinant for others of the same species.
- These antigenic determinants are called idiotopes.
- Immunoglobulins differ in their idiotopes found in the variable region, known as idiotypic variation.
- Idiotypes arise from mutations (somatic hypermutations) in the variable region genes.
- Thus, idiotypes may seem foreign to the host, but they do not trigger an autoimmune response due to their small numbers.
Allotypes
Allotypes refer to the antigenic markers present in the isotype genes of the constant region of heavy (H) and light (L) chains, which are determined by various alleles.
- All members of a species inherit the same set of isotype genes, but some genes have multiple alleles.
- As a result, allotypes can be found in the constant region of immunoglobulin (Ig) molecules of the same class in some members of a species, but not in others.
- Allotypes are classified into specific types, such as kappa light chains and gamma (γ) and alpha (α) heavy chains.
- Anti-allotype antibodies may develop after a blood transfusion or through maternal transfer of IgG to the fetus.
Monoclonal Antibodies
Monoclonal antibodies (mAb) are antibodies produced from a single clone of plasma cells, all recognizing the same antigen—meaning they target a single epitope of an antigen.
The hybridoma technique is used to create mAb (Nobel Prize winners G. Kohler and C. Milstein):
- A mouse B-cell, stimulated against one specific epitope of an antigen, is fused with an immortal cell, such as a myeloma cell, which can replicate indefinitely.
- This fusion creates a hybridoma cell with two main characteristics:
- It produces mAb with the same antigen specificity (thanks to the B-cell).
- It replicates indefinitely, creating clones of identical cells (due to the myeloma cell).
- However, in the reaction chamber, there will also be some unfused mouse B-cells and unfused myeloma cells, which are removed by sub-culturing the fluid in a special medium known as HAT media.
- HAT medium contains hypoxanthine, aminopterin, and thymidine.
Purine synthesis in mammalian cells (like splenic B-cells) can occur through:
- De novo pathways
- Salvage pathways
Definitions:
- Epitope: The specific part of an antigen that an antibody targets.
- Paratope: The specific site on the antibody that binds to the epitope.
- Idiotope: The antigenic determinant of an antibody, found in the variable region of H & L chains.
- Isotype: The classes and subclasses of antibodies that differ in the constant region of heavy chains.
Effects of HAT media on different cell types:
- Unfused splenic B-cells: They can grow but do not last long as they are not immortal.
- Unfused myeloma cells: They cannot grow because they lack the HGPRT enzyme needed for the salvage pathway.
- Hybridoma cells: They can grow and survive long-term.
Types of Monoclonal Antibodies
- Mouse mAb: Contains 100% mouse-derived proteins.
- Chimeric mAb: 34% mouse proteins (variable region) and 66% human proteins (constant region).
- Humanised mAb: The antigen-binding site is 10% mouse-derived, with the rest human-derived.
- Human mAb: 100% human-derived amino acids.
Noncovalent Interactions in Antigen-Antibody Reaction
- Hydrogen bonds
- Electrostatic interactions
- Hydrophobic interactions
- Van der Waals forces
Marrack's Lattice Hypothesis
- Zone of equivalence: When antigen and antibody levels are equal.
- Prozone: Excess antibody present.
- Postzone: Excess antigen present.
Role of Aminopterin in HAT Media
- Aminopterin blocks the de novo pathway, forcing the cell to use the salvage pathway to create purines for survival.
- The salvage pathway relies on two essential enzymes:
- HGPRT (hypoxanthine guanine phosphoribosyl transferase)
- Thymidine kinase
- Thus, any cell (e.g., a myeloma cell) lacking HGPRT cannot grow in HAT medium.
Selection of Individual Hybridoma Cells
- Individual hybridoma cells can be selected through techniques such as:
- Radioimmunoassay
- ELISA
- Using specific antigen fragments to identify desired hybridoma cells.
Different Types of Monoclonal Antibodies
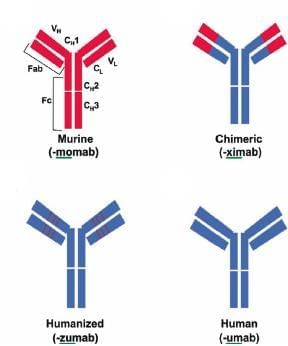
- Mouse mAb: These antibodies are made entirely from mouse-derived proteins. However, because these proteins are foreign to humans, they can trigger an immune response. This response leads to the production of human anti-mouse antibodies (HAMA), which can accelerate the clearance of the monoclonal antibody from the human body.
- Chimeric mAb: Chimeric monoclonal antibodies are created by combining 34% mouse-derived proteins (found in the variable region) with 66% human-derived proteins (located in the constant region). This blend helps reduce the likelihood of an immune response while retaining the antibody's effectiveness.
- Humanized mAb: Humanized monoclonal antibodies consist of approximately 10% mouse-derived proteins, primarily located at the antigen-binding site. The remaining structure is mostly human-derived, but some mouse sequences are retained for functional purposes. This modification aims to enhance compatibility with the human immune system.
- Human mAb: Human monoclonal antibodies are made entirely from human-derived amino acids. Because of their human origin, they are less likely to provoke an immune response and are considered the most effective type of monoclonal antibody.
Antigen-Antibody Reactions
- Antigen (Ag) and Antibody (Ab) reactions have some key features:
- Specificity: This reaction happens when a specific part of an antigen, called an epitope, interacts with the matching part of its antibody, known as the paratope.
- There are non-covalent interactions between the antigen and its antibody, which include:
- Hydrogen bonds
- Electrostatic interactions
- Hydrophobic interactions
- van der Waals forces
- Strength: The strength of the interaction is determined by affinity and avidity.
- Affinity: This refers to the total of all non-covalent interactions that occur between a single epitope of an antigen and its corresponding paratope on the antibody. It can be measured using:
- Equilibrium dialysis
- Surface plasmon resonance method
- Avidity: This term describes the overall strength of all binding sites when a multivalent antibody binds to a complex antigen that has multiple epitopes.
Marrack’s Lattice Hypothesis
When serum containing antibodies is diluted in normal saline, the antibody level decreases gradually. When a fixed amount of antigen is added to these diluted samples:
- The Ag-Ab reaction works best in the middle tubes, where the amounts of antigen and antibody are equal (known as the zone of equivalence).
- In the earlier tubes, antibodies are in excess, so the Ag-Ab reaction does not take place; this is called the prozone phenomenon.
- In the later tubes, antigen is in excess, resulting in the failure of the Ag-Ab reaction; this is known as the postzone phenomenon.
This lattice hypothesis applies to all Ag-Ab reactions.
Types of Antigen-Antibody Reactions
Conventional Techniques include:
- Precipitation
- Agglutination reaction
- Complement fixation test
- Neutralisation test
Newer Techniques include:
- ELISA (Enzyme-Linked Immunosorbent Assay)
- IFA (Immunofluorescence Assay)
- RIA (Radioimmunoassay)
- CLIA (Chemiluminescent Immunoassay)
- Immunohistochemistry
- Rapid tests (Lateral flow assay or ICT and Flow through assay)
- Western blot
- Immunoassays using electron microscope
Precipitation Reaction
When a soluble antigen interacts with its antibody under the right conditions of temperature, pH, and electrolytes (like NaCl), it results in the creation of a complex made of the antigen and antibody.
- This complex can appear in two forms:
- An insoluble precipitate band when using a gel as the medium.
- Insoluble floccules when using a liquid medium.
1. Precipitation in Liquid Medium
- Ring test: Used for streptococcal grouping by the Lancefield technique and Ascoli’s thermoprecipitation test for anthrax.
- Slide flocculation test: VDRL and RPR serological tests for diagnosing syphilis.
- Tube flocculation test: Kahn test, previously used for syphilis.
2. Precipitation in Gel (Immunodiffusion)
It has many advantages over liquid medium:
(i) Clear visible bands are formed, which can be preserved for longer time,
(ii) Individual antigens from a mixture can be differentiated, e.g.
- Single diffusion in one dimension (Oudin procedure)
- Double diffusion in one dimension (Oakley–Fulthorpe procedure)
- Single diffusion in two dimensions (Radial immunodiffusion)
- Double diffusion in two dimensions (Ouchterlony procedure)
3. Precipitation in Gel in Presence of Electric Current
The movement of Ag and Ab can be made faster if immunodiffusion in gel is carried out in presence of electric current.
Examples include:
- Electroimmunodiffusion (EID)
- CIEP (Countercurrent immunoelectrophoresis)
- Rocket electrophoresis.
Agglutination Reaction
- It involves the clumping of particles when a solid or insoluble antigen is mixed with its antibody under suitable conditions of electrolytes, temperature, and pH.
- This reaction is more sensitive than the precipitation test, making it easier to observe and interpret the clumps.
Diagnostic Applications of Agglutination Tests
- Slide Agglutination: Used for confirming the identification and serotyping of bacterial colonies from culture.
- Tube Agglutination: Commonly used for various diagnostic purposes, including:
- Typhoid Fever (Widal Test): Detects antibodies against H (flagellar) and O (somatic) antigens.
- Acute Brucellosis: Standard agglutination test for diagnosis.
- Blood Grouping: Determining ABO and Rh blood groups.
- Coombs Test (Antiglobulin Test): Detects incomplete Rh antibodies:
- Direct Coombs Test: Identifies bound Rh antibodies in the serum of the fetus or baby.
- Indirect Coombs Test: Detects free Rh antibodies in maternal serum that may affect the fetus.
- Heterophile agglutination tests:
- Typhus fever (Weil–Felix reaction).
- Infectious mononucleosis (Paul Bunnell test).
- Mycoplasma pneumonia (Cold agglutination test).
- Microscopic agglutination test (MAT) for leptospirosis.
- Indirect or passive agglutination test: Antigen coated on carriers like latex or RBCs to find antibodies (Ab) in serum. Examples:
- Indirect hemagglutination test (IHA).
- Latex agglutination test (LAT) for antibody detection, e.g., ASO.
- Reverse passive agglutination test: Antibody (Ab) coated on carriers to detect antigen (Ag) in serum. Examples:
- RPHA (Reverse passive hemagglutination assay), e.g., HBsAg detection.
- Latex agglutination test for antigen detection, e.g., CRP, RA factor, capsular antigen in CSF, and streptococcal grouping.
- Coagglutination test (using S. aureus protein A as a carrier).
Complement Fixation Test
- CFT detects complement-fixing antibodies in patients’ serum. It is now rarely used:
- Wasserman test was widely used for diagnosing syphilis.
- CFT was also used to detect antibodies in Rickettsia, Chlamydia, Brucella, Mycoplasma infections, and some viral infections like arboviruses and rabies.
- Indirect complement fixation test: Identifies certain bird (e.g., duck, parrot) and mammal (e.g., horse, cat) serum antibodies that cannot fix guinea pig complement.
- Conglutination test: Conducts CFT using non-hemolytic complements, e.g., horse complements.
Complements are also used for various serological tests, other than CFT, such as:
- Treponema pallidum immobilization test (to detect antibodies to T. pallidum).
- Sabin-Feldman dye test for detecting Toxoplasma antibodies.
- Vibriocidal antibody test for V. cholerae.
Neutralization Test
- Neutralization tests are less commonly used nowadays. Examples include:
- Viral neutralization test: Identifies viral neutralising antibodies.
- Plaque inhibition test: Conducted for bacteriophages.
- Schick test for Corynebacterium diphtheriae.
- Nagler’s reaction: Due to α-toxin of Clostridium perfringens.
- ASLO detection in the past (now done by latex agglutination).
- Hemagglutination inhibition (HAI) test.
Modern Techniques for Detecting Antigen-Antibody Reactions
Modern methods for detecting antigen-antibody reactions involve using a detector molecule to label either the antibody or the antigen. This labeling helps identify the corresponding antibody or antigen in a sample by creating a visible effect. While these techniques operate on similar principles, they differ in the type of labeled molecule used and the visible effect produced.
Key Aspects of Modern Techniques
- Immunoassay Method: Refers to the specific method used for the immunoassay.
- Molecules Used for Labeling: Indicates the type of molecule used for labeling in the assay.
- Type of Visible Effect: Describes the visible effect produced as a result of the labeling.
1. Enzyme Linked Immunosorbent Assay (ELISA)
- Principle: In ELISA, an enzyme-linked antibody or antigen is used to capture and detect the target antigen or antibody.
- Detection Method: colour change is detected by a spectrophotometer, indicating the presence of the target molecule.
2. Immunofluorescence Assay
- Principle: This assay uses a fluorescent dye to label the antibody or antigen.
- Detection Method: The fluorescent dye emits light when excited, and this emitted light is detected by a fluorescence microscope, indicating the presence of the target molecule.
3. Radioimmunoassay
- Principle: In this technique, a radioactive isotope is used to label the antibody or antigen.
- Detection Method: The radioactive isotope emits β and γ radiations, which are detected by β and γ counters, indicating the presence of the target molecule.
4. Chemiluminescence-linked Immunoassay
- Principle: Chemiluminescent compounds are used to label the antibody or antigen in this assay.
- Detection Method: These compounds emit light when triggered, and the emitted light is detected by a luminometer, indicating the presence of the target molecule.
5. Immunohistochemistry (IHC)
- Principle: In IHC, an enzyme or fluorescent dye is used to label the antibody or antigen in tissue samples.
- Detection Method: colour change visible to the naked eye or fluorescence microscopy indicates the presence of the target molecule in tissue samples.
6. Western Blot (WB)
- Principle: WB detects specific proteins (antibodies) in a sample containing a mix of antibodies targeting different antigens of the same microbe.
- Detection Method: colour band visible to the naked eye indicates the presence of the target protein in the sample.
7. Immunochromatographic Test
- Principle: Colloidal gold or silver is used to label the antibody or antigen in this test.
- Detection Method: colour band visible to the naked eye indicates the presence of the target molecule in the sample.
8. Protein A Conjugate
- Principle: Immunoferritin is used in electron microscopy to detect specific antibodies in tissue samples.
- Detection Method: Electron-dense molecules like ferritin appear as black dots under an electron microscope, indicating the presence of the target antibody in the sample.
Components of Western Blot
- Western blot is a method used to find specific proteins (antibodies) in a sample that has a mix of antibodies, each aimed at different parts of the same microbe.
- The name "Western blot" comes from its resemblance to the Southern blot, which is used to find DNA fragments, and the Northern blot, which detects mRNAs.
- The Eastern blot is the newest technique in this series; it modifies the Western blot to identify carbohydrate epitopes found on proteins or lipids.
- The Western blot process has three main steps:
- Separation of a complex mixture of protein antigens into smaller pieces using SDS PAGE (sodium dodecyl sulfate-polyacrylamide gel electrophoresis).
- NCM blotting: The protein fragments from the gel are moved (or blotted) onto a Nitrocellulose membrane (NCM).
- Enzyme immunoassay: This step detects specific antibodies in a patient's serum, which contains a mix of antibodies.
Introduction of Rapid Tests
Rapid tests are a game changer for identifying infectious diseases.
- They are very easy to use because they only need one step to get results.
- Results are available quickly, typically in 10 to 20 minutes.
- These tests require very little training to perform.
- No complex equipment is necessary to carry out these tests.
- Often referred to as Point of Care (POC) tests, they can be done without laboratory tools.
- Unlike ELISA and other immunoassays, POC tests provide immediate results.
Two principles of rapid tests:
- Lateral Flow Assay (Immunochromatographic Test - ICT):
- In this method, colloidal gold or silver is used for labeling the sample.
- The sample flows laterally through the nitrocellulose membrane (NCM).
- An example of this technique is the detection of antigens in malaria cases.
- Flow Through Assay:
- Instead of gold conjugate, Protein A is used for labeling in this method.
- The sample flows vertically through the nitrocellulose membrane, which distinguishes it from the lateral flow used in ICT.
- A common application of this method is the HIV tridot test.
What is Complement?
Complement refers to a group of proteins present in the serum, which are usually inactive. However, upon activation, these proteins play a crucial role in enhancing the immune response.
- Complement proteins make up about 5% of normal serum proteins.
- They are nonspecific to antigens, meaning their levels do not increase after infection or vaccination.
- Complement proteins are also nonspecific to species, as they are found in different species.
- These proteins are heat labile, which means they can be inactivated at 56°C for 30 minutes.
- Complement proteins bind to the Fc region of antibodies, with IgM binding strongly, followed by IgG3, IgG1, and IgG2.
- Most complement proteins are synthesized by the liver, but they can also be produced by the gastrointestinal tract, macrophages, and spleen.
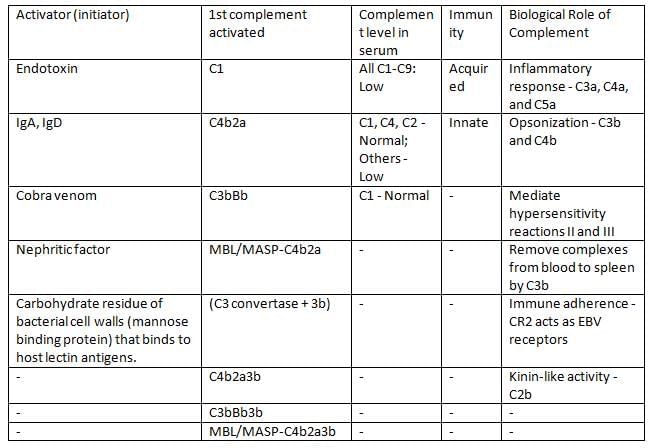
Complement Pathways
There are three pathways for activating the complement system:
- Classical pathway: This pathway is triggered by the antigen-antibody complex and is dependent on antibodies.
- Alternative pathway: This pathway is triggered directly by the antigen and does not require antibodies.
- Lectin pathway: This pathway is similar to the classical pathway but is also independent of antibodies.
Stages of Complement Activation
- The activation of any complement pathway involves four main stages:
- Initiation of the pathway.
- Formation of C3 convertase.
- Formation of C5 convertase.
- Formation of the membrane attack complex (MAC).
- All pathways converge at the formation of C3 convertase, and the remaining stages are the same across all pathways.
Biological Role of Complement
- Target cell lysis: The MAC creates pores in the target cell membrane, leading to cell lysis.
- Inflammatory response: By-products such as C3a, C4a, and C5a act as anaphylatoxins and chemotactic factors, promoting inflammation.
- Opsonization: C3b and C4b are key opsonins that enhance phagocytosis.
- Complement proteins mediate hypersensitivity reactions II and III.
- Complement proteins help remove immune complexes from the blood to the spleen via C3b.
- Immune adherence: CR2 acts as a receptor for Epstein-Barr virus (EBV).
- Kinin-like activity: C2b increases vascular permeability.
Differences between the three complement pathways
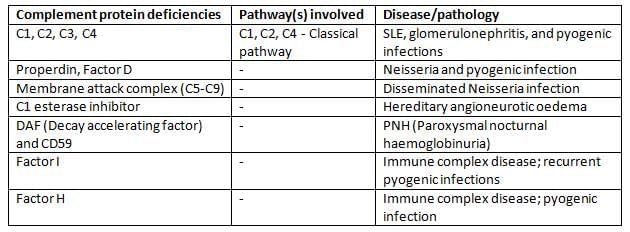
Complement deficiency diseases
|
75 docs|5 tests
|
FAQs on Antigen, Antibody, Antigen-Antibody Reaction, Complement Chapter Notes - Microbiology - NEET PG
| 1. What are antigens and how do they function in the immune response? |  |
| 2. What are antibodies, and what is their role in antigen-antibody reactions? |  |
| 3. What are the different types of antigen-antibody reactions? |  |
| 4. What are some newer techniques used to study antigen-antibody reactions? |  |
| 5. How does the complement system interact with antigen-antibody reactions? |  |















