National Health Programmes, Policies and Legislations in India - 1 Chapter Notes | Preventive and Social Medicine (PSM) - NEET PG PDF Download
Revised National TB Control Program
Epidemiology of Tuberculosis in India
- ARI (India): 1-2% (average ARI = 1.7%)
- For every 1% rise in ARI, there are 50 SS +ve cases per lakh population.

Key Notable Points regarding Tuberculosis
- Every TB sputum positive patient can infect up to 10-15individuals in a year.
- Without treatment, 50% of TB patients will die, 25% will remain healthy, and 25% will develop chronic infectious TB.
- TB is the 'Barometer of Social Welfare in India.'
- TB (AFB) Bacillus was discovered by Robert Koch.
- TB Bacilli are alcohol and acid fast.
- Generation time of TB bacilli: 20 hours.
- TB bacteria remain alive: in sputum for 1 day and in droplet nuclei for 10 days.
- Diagnosis in RNTCP. Ziehl Neelsen Staining.
- World TB Day. 24th March.
- TB was declared a global emergency in 1983 by WHO.
- TB is one of the most common opportunistic infections among HIV patients in India.
- Elimination level for Tuberculosis (WHO and STOP TB Strategy): < 1 case per million population (to eliminate TB as a public health issue).
- TB Institutes of importance in India:
- National Tuberculosis Institute: Bangalore
- Tuberculosis Research Centre: Chennai
- LRS Institute of TB and Respiratory Diseases: New Delhi
Annual Risk of Infection (ARI)
- Definition: The proportion of the population that will be primarily infected with tuberculosis in one year.
- Public health importance: Reflects the incidence of TB infection.
- Tuberculin Conversion Index:
- Indicates the incidence of TB infection.
- Best indicator of TB trends unaffected by current control measures.
- Most informative index of the magnitude of the TB problem.
Ziehl Neelsen (ZN) Staining
- Importance: Sputum smear of a suspected TB patient is used for diagnosis.
- Decolourizer: 25% sulphuric acid.
- Acid Fast Bacilli (AFB)of TB: 'Rod shaped' with 'beaded appearance' (Beads: Mycolic Acid).
- Minimum bacillary load for a positive result: >10,000 bacilli per ml sputum.
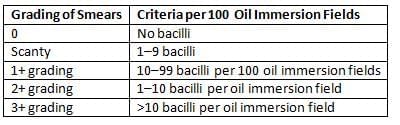
- Results of ZN staining. Minimum 100 fields examined.
Directly Observed Treatment Short Course (DOTS)
- Description: A community-based TB treatment and care strategy that combines supervised treatment with community support.
- Success of Dots depends on five components:
- Political commitment
- Good quality sputum microscopy
- Directly observed treatment
- Uninterrupted supply of good quality drugs
- Accountability
- Ensures high cure rates through three components:
- Appropriate medical treatment
- Supervision and motivation by health/non-health personnel
- Monitoring of disease by health services
- DOTS is administered by peripheral health staff, referred to as 'DOTS Agents'(e.g., MPWs, voluntary workers like teachers, Anganwadi workers, Dais).
- Incentive/honorarium paid: 150/- per patient completing treatment.
- Drugs are supplied in patient-wise boxes containing a full course of treatment:
- Intensive phase: Each blister pack contains one day's medication.
- Continuation phase: Each blister pack contains one week's medication.
- Principles of DOTS administration:
- DOTS is directly observed treatment short course chemotherapy.
- In DOTS, during the intensive phase of treatment, a health worker or trained person observes as the patient swallows the drugs.
- During the continuation phase, the patient receives medicine for one week in a multiblister combipack, with the first dose swallowed in the presence of a health worker.
- In the continuation phase, the patient's medicine consumption is verified by returning the empty multiblister combipack when they come to collect their medication for the next week.
- This program uses alternate day treatment.
- Patient Compliance in Tuberculosis Treatment
- Patient compliance is of utmost importance throughout the prescribed period of treatment. It is the primary consideration, while all other factors are secondary.
- Drugs are administered category-wise, meaning that the same regimen is not given to all patients.
- Streptomycin is only given in Category II.
- In Category I, sputum examinations are conducted for new smear-positive cases at 2, 4, and 6 months.
Revised National Tuberculosis Control Program (RNTCP)
- Differences between National Tuberculosis Program (NTP) and RNTCP:
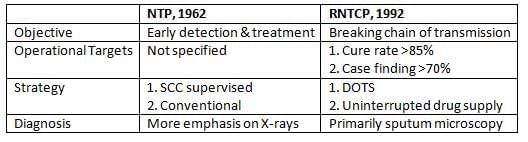
- Objectives of RNTCP:
- To achieve a cure rate of at least 85% through the administration of short course chemotherapy (SCC), and
- To achieve a case detection rate of 70% (only after having achieved the desired cure rate).
- History of RNTCP:
- RNTCP (based on the DOTS strategy) began as a pilot in 1993 and was launched as a national program in 1997.
- Rapid RNTCP expansion began in late 1998.
- By 24th March 2006, the entire country was covered under DOTS, covering approximately 1.14 billion people.
- Infrastructure:
- The RNTCP designated 'Microscopy Centre' is established for approximately 100,000 population (50,000 in hilly and mountainous areas).
- Senior TB Laboratory Supervisor (STLS) is one for every 5 microscopy centres.
- STLS rechecks all positive slides and 10% of all negative slides.
- Diagnosis in RNTCP:
- In RNTCP, the mainstay of diagnosis is sputum microscopy; the sputum smears are stained for acid-fast bacilli (AFB) with 'Ziehl-Neelsen (ZN) stain.'
- Decolorizer: 25% sulphuric acid.
- Counter-stain: 0.1% Loeffler's methylene blue (or 1% picric acid or 0.2% malachite green ).
AFB Sputum Smears (SS) for Diagnosis of a Case of TB [New Guidelines]
- Tuberculosis suspect:. person with a productive cough for more than 2 weeks with or without hemoptysis, fever for more than 2 weeks, chest pain, weight loss, night sweats, and loss of appetite is subjected to 2 SS examinations.
- Number of specimen(s) required for the diagnosis of smear-positive pulmonary
- Tuberculosis: Two.
- ' 2 sputum smears ' over 2 daysperiod:
- Spot Sample (Day 1)
- Morning Sample (Day 2)
- ' 2 sputum smears ' over 2 daysperiod:
- Chances of detecting smear-positive cases:
- With 1 sample: 80%
- With 2 samples: 93%
- Interpretation of Results of 2 Sputum Smear Examinations:
- None sputum positive: Give antibiotics for 10-14 days.
- Cough relieved: Non-tuberculosis person.
- Cough persists: REPEAT two sputum smear examinations.
- (a) None sputum positive: X-ray chest findings suggestive of TB: Sputum negative tuberculosis; Start ATT.
- No findings suggestive of TB: Non-tuberculosis person.
- (b) One sputum positive: Sputum positive pulmonary tuberculosis; Start ATT.
- (c) Two sputum positive: Sputum positive pulmonary tuberculosis; Start ATT.
Categorization and Treatment Regimens in RNTCP [New Guidelines]
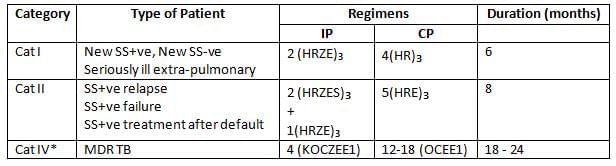
- (*Category IV - DOTS Plus; Category III has been merged into Category I)
- Letters:
- R - Rifampicin
- E - Ethambutol
- H - Isoniazid
- S - Streptomycin
- Z - Pyrazinamide
- K - Kanamycin
- O - Ofloxacin
- Et - Ethionamide
- C - Cycloserine
- Numbers:
- The numbers before letters refer to months of treatment (2 implies two months of treatment).
- The numbers after letters refer to the frequency of administration per week (3 implies thrice per week).
- Seriously Ill Extra-Pulmonary TB:
- Meningitis
- Disseminated TB
- Tuberculous pericarditis
- Peritonitis
- Bilateral or extensive pleurisy
- Spinal disease with neurological complaints
- SS-ve TB with extensive parenchymal involvement
- Intestinal and genitourinary TB.
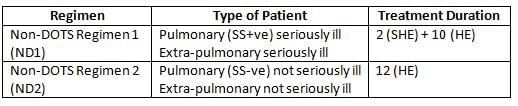
Daily Self-administered Non-DOTS Regimens [New Guidelines]
- Indication: Only if there are adverse reactions to drugs or patient compliance is not possible.
AFB Sputum Smears (SS) for Follow-up of a Case of TB during Treatment [New Guidelines]
- Timing: At the end of 2 months, at the end of 5 months, and at the end of 8 months.
- Interpretation:
- None Positive: Declared Sputum Smear Negative (SS -ve)
- One Positive: Declared Sputum Smear Positive (SS +ve)
- Two Positive: Declared Sputum Smear Positive (SS +ve)
- If Sputum Smear is Positive at the End of the Intensive Phase (IP):
- Category I: Extend the Intensive Phase by 1 month. Conduct a Sputum Smear examination at the end of the extended Intensive Phase. Move the patient to the Continuation Phase (CP), regardless of the Sputum Smear examination results.
- Category II: Extend the Intensive Phase by 1 month. Conduct a Sputum Smear examination at the end of the extended Intensive Phase. Move the patient to the Continuation Phase (CP), regardless of the Sputum Smear examination results.
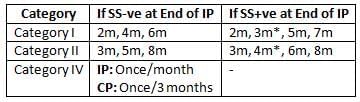
- Note: Patients begin Continuation Phase treatment at 3 months, regardless of Sputum Smear examination results.
Important Definitions in RNTCP
- New Case: Person with tuberculosis (TB) who has either never received treatment or has received treatment for less than 4 weeks.
- Cured: Person who was initially sputum smear positive (SS +ve), completed TB treatment, and had sputum smear negative (SS -ve) results on at least two separate occasions, with one of these occurring at the end of treatment.
- Relapse: Person who was declared cured of TB but returns with a positive sputum smear (SS +ve).
- Failure: Person undergoing TB treatment who remains sputum smear positive (SS +ve) after 5 months of treatment.
- Defaulter: Person who, after being registered for TB treatment, has not taken anti-TB medications for 2 months or more consecutively.
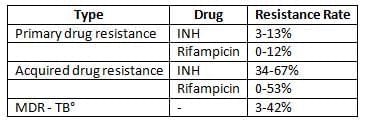
Drug Resistance in Tuberculosis (TB)
- Primary (Initial) Resistance: This type of resistance occurs when a person is infected by someone who has TB bacteria that are resistant to drugs.
- Secondary (Acquired) Resistance: This resistance develops during the course of TB treatment.
- Multidrug Resistant TB (MDR-TB): This condition is characterized by resistance to the drugs Isoniazid and Rifampicin, which may be accompanied by resistance to other drugs as well.
Treatment of Multidrug Resistant TB (MDR-TB):
- DOTS PLUS (Category IV): Treatment under this category must be based on sensitivity testing to ensure the right drugs are used.
- Directly observed therapy is crucial for improving treatment outcomes and is a fundamental aspect of MDR-TB treatment.
- When the sensitivity of the TB strain is known, and it is confirmed resistant to both Isoniazid (INH) and Rifampicin (RMP), the
- Following five drugs should be selected in this order, based on known sensitivities:
- Aminoglycoside (such as amikacin or kanamycin) or polypeptide antibiotic (like capreomycin)
- Pyrazinamide
- Ethambutol
- Fluoroquinolones, with moxifloxacin being the preferred choice
- Rifabutin
- Additional Options: The following drugs can also be considered based on the specific case:
- Cycloserine
- Thioamide (prothionamide or ethionamide)
- Para-aminosalicylic acid (PAS)
- Macrolide (such as clarithromycin)
- Linezolid
- High-dose INH (if there is low-level resistance)
- Interferon-alpha
- Thioridazine
Extensive Drug Resistant TB (XDR-TB):
- XDR-TB is defined by resistance to Rifampicin and Isoniazid, as well as resistance to any drug in the quinolone family and to one injectable second-line drug (such as Kanamycin, Capreomycin, or Amikacin).
- XDR-TB is essentially a form of MDR-TB with additional resistance to 3-6 classes of second-line drugs.
- The treatment principles for MDR-TB and XDR-TB are generally the same.
- XDR-TB is not easily spread in healthy populations but can lead to outbreaks in individuals already compromised by conditions such as HIV.
- Drug Resistance (TB) in India:
Tuberculin Test and Mantoux Test (also known as Pirquet test or PPD Test)
- Dose: Tuberculin Unit (TU) in 0.1 ml.
- The Mantoux test is a tool used for detecting infection by the tuberculosis bacterium, Mycobacterium tuberculosis.
- Positive reaction: Positive reaction indicates either a past or present infection by Mycobacterium tuberculosis.
- WHO recommended preparation: PPD-RT-23 with Tween-80 is the recommended preparation by WHO.
- Reading after 72 hours: The test is read after 72 hours, and the following criteria are used:
- Reactions >10 mm: Positive
- Reactions 6-9 mm: Doubtful
- Reactions <6 mm: Negative
- Tuberculin test conversion: tuberculin test conversion is defined as an increase of more than 10 mm within a 2-year period, regardless of the age of the individual.
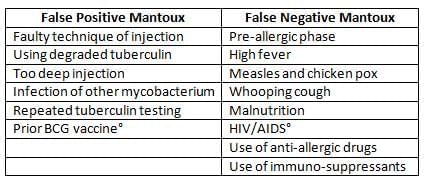
- False Mantoux Reactions:
Antitubercular Drugs
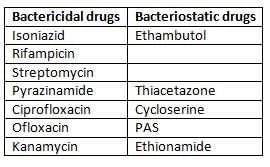
- Isoniazid:
- This was the first effective bactericidal drug used to treat tuberculosis.
- It may also act as a bacteriostatic at lower concentrations and is effective against both extracellular and intracellular organisms causing the disease.
- Rifampicin:
- The only bactericidal drug effective against 'persisters' or dormant bacilli in solid caseous lesions.
- Acts on extracellular as well as intracellular organisms.
- Works best on slowly or intermittently dividing (spurters ).
- Pyrazinamide:
- Targets intracellular bacilli.
- Acts on bacilli at sites of inflammatory response.
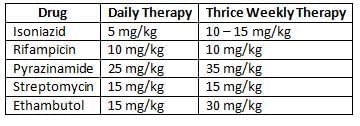
Dosages of Antitubercular Drugs
Important Facts of Antitubercular Drugs
- Rifampicin is the most effective and bactericidal anti-tubercular drug.
- Isoniazid is the most toxic and causes rapid sputum conversion.
- Rifampicin causes orange discoloration of urine and is contraindicated in AIDS patients on Protease Inhibitors.
- Isoniazid is the first drug to develop resistance.
- Thiacetazone is contraindicated in HIV due to exfoliative dermatitis.
- Streptomycin is an injectable antitubercular drug but is contraindicated in pregnancy and in children under 6 years of age.
- Ethambutol is contraindicated in children under 6 years of age and can cause optic neuritis (red-green color blindness).
- Streptomycin can cause vestibular damage.
- Rifampicin and Isoniazid are contained in all phases of all categories of DOTS
National Polio Elimination Program (NPEP)
Pulse Polio Immunization (PPI) Program in India
- Launched in India: 1995-96 (1st round on 9th Dec 1995 and 20th Jan 1996).
- First PPI targeted children under 3 years of age.
- Later, WHO recommended age group be 0-5 years (1996-97).
- Meaning of 'Pulse'?: Mass administration of Oral Polio Vaccine (OPV) on a single day to 'all children 0-5 years', regardless of their previous immunisation status.
- PPI aims to replace wild polio virus in the community with vaccine-derived virus.
- PPI is in addition to routine immunisation.
- Intensive Pulse Polio Immunization (IPPI): Added rounds with fixed booths and 'house-to-house search-and-vaccinate' approach.
- Success of PPI (India): 35,000 cases annually in 1995-96 to NIL cases in 2013.
Basic Strategies to Eradicate Poliomyelitis from India:
- Routine immunisation.
- PPI/National Immunisation Day (NID)/Sub-NID (SNID).
- Surveillance of acute flaccid paralysis (AFP).
- Conduct extensive house-to-house immunisation mopping-up campaigns.
Vaccine Vial Monitor (VVM)
- Description: A simple tool (sticker on OPV vial) that indicates whether the vaccine is potent at the time of administration.
- Mandatory since 1998 for quality assurance.
WHO Grading of VVM (OPV):
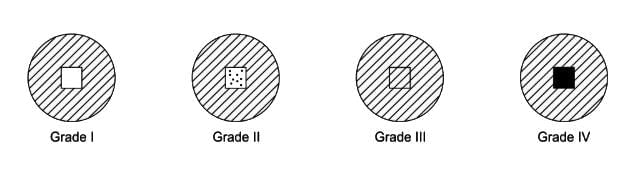 VVM (Vaccine Monitor)
VVM (Vaccine Monitor)
Acute Flaccid Paralysis (AFP) Case Investigation:
- AFP: Acute onset (<4 weeks) in a child under 15 years, or any case of paralytic illness in a person of any age when polio is suspected.
- Acute: Rapid progression from onset to maximum paralysis.
- Flaccid: Loss of muscle tone, 'floppy' instead of spastic or rigid.
- Paralysis: Weakness, loss of voluntary movement.
- Differential diagnosis of AFP:
- Descending asymmetric flaccid lower motor neuron (LMN) paralysis.
- Guillain Barre Syndrome (Cytologico-albuminic dissociation).
- Transverse myelitis (Normal CSF, sensory loss+, bladder dysfunction+).
- Traumatic neuritis (any age, only one leg involved).
- Other non-polio enteric viruses: Coxsackie-B, ECHO, Enterovirus type 70 and 71, Mumps.
- Active case search in the community:
- In the community where an AFP case resides or where an AFP case has visited during the incubation period for polio (4-25 days before paralysis onset), a house-to-house active case search is conducted.
- This activity is carried out immediately along with active case search for any children under 15 years who have had the onset of AFP within the preceding 60 days.
- All cases found are investigated promptly, with the collection of two stool specimens before OPV administration.
- Adequate stool sample collection: From every AFP case, stool samples are collected for diagnosing poliomyelitis.
- Acute Flaccid Paralysis (AFP): Is a condition characterized by the sudden onset of weakness in the muscles, leading to a flaccid (limp) appearance. It is crucial to monitor and investigate cases of AFP, especially in children, as it can be indicative of serious underlying conditions, including viral infections like poliomyelitis.
- This document outlines the standard operating procedures for the collection, transport, and laboratory analysis of stool specimens from AFP cases, as well as the necessary follow-up and surveillance measures to ensure effective monitoring and response to potential outbreaks.
- Objective:
- Samples should be collected 48 hours apart.
- Specimens must be gathered within 14 days of the onset of paralysis (or, at most, within 8 weeks ).
- Each specimen should weigh a minimum of 8 grams (roughly the size of an adult thumb).
- Samples should be collected in a clean, dry, screw-capped container (there's no need for sterility or preservatives).
- Transport samples to the lab using a Reverse cold chain method, maintaining temperatures between +2°C to +8°C.
- A Standard Lab Request Form (LRF) must accompany the specimens.
Outbreak Response Immunization (ORI):
Following the collection of stool specimens and the investigation of Acute Flaccid Paralysis (AFP) cases, Outbreak Response Immunization (ORI) is carried out in the affected community.
- Children aged 0-59 months are administered one dose of Oral Polio Vaccine (OPV), irrespective of their previous immunizations, in the locality where the AFP case was identified.
- The travel history of the AFP child may suggest other locations that require ORI.
- A minimum of 500 children should be vaccinated during the ORI.
60-Day Follow-Up for AFP Cases:
- The District Immunisation Officer (DIO) is required to visit each AFP case 60 days after the onset of paralysis to assess for any residual weakness.
- This follow-up visit should be conducted before the 70th day post-onset.
- Residual weakness can be identified by:
- Measuring mid-arm or mid-thigh circumference to detect any wasting on one side.
- Observing asymmetry in the skin folds on the inner thighs.
WHO Indicators of AFP Surveillance & Laboratory Surveillance
- The two most critical indicators are:
- Non-polio AFP rate in children under 15 years (target: > 1/100,000 ): If this rate is ≤ 1/100,000, the surveillance system may be missing cases of AFP.
- Reported AFP cases with 2 stool specimens collected within 14 days of paralysis onset (target: > 80% ).
- Other important indicators include:
- Timeliness of weekly 'zero reporting' (target: > 80% ).
- Investigation of reported cases within 48 hours of reporting (target: > 80% ).
- Completeness of weekly 'zero reporting' (target: > 90% ).
- Follow-up examinations for reported AFP cases at least 60 days after paralysis onset (target: > 80% ): This includes cases with inadequate or no stool specimens, isolation of vaccine virus, isolation of wild poliovirus, or any case suspected of poliomyelitis on initial examination ('hot case').
- Specimens should arrive at the national lab within 3 days of being sent (target: > 80% ).
- Specimens arriving in 'good condition' (target: > 80%): Conditions include:
- Use of frozen ice packs or ice, or a temperature indicator showing <> .
- Specimen volume must be adequate (> 8 grams ).
- No signs of leakage or drying.
- Proper documentation must be completed (laboratory request/reporting form).
- Specimens should have a 'turn-around time' of <28> (target: > 80% ): This is the time from receipt to reporting of results.
- Stool specimens from which a non-polio enterovirus is isolated (target: > 10% ):
- This indicates the quality of the 'reverse cold chain' (i.e., that specimens were kept at temperatures <>8°C during transport).
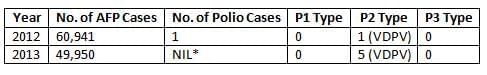
AFP and Poliomyelitis Data - India
RCH Program
The key components of the RCH Program include
- Community Needs Assessment Approach (CNAA): Systematic approach to identify and address the specific health needs of the community.
- Integrated Packages of Services for Mother and Child: Comprehensive healthcare services tailored for mothers and children.
- Medical Termination of Pregnancy (MTP) Services at Primary Health Centers (PHCs): Including safe abortion options to ensure reproductive health.
- Control and Prevention of Reproductive Tract Infections (RTI) and Sexually Transmitted Infections (STI): Essential for safeguarding reproductive health.
- Adolescent Health: Focused on the specific health needs of adolescents.
- Services in Urban Slums: Targeted healthcare services for vulnerable populations in urban slum areas.
- Improving Quality of Services: Ensuring high standards of healthcare delivery.
- Addressing Unmet Needs and Sub-Centre Action Plans: Identifying and fulfilling unmet healthcare needs at the sub-centre level.
- Communication Strategy: Effective communication to raise awareness and promote health services.
- Gender Sensitiveness: Ensuring gender-sensitive approaches in healthcare delivery.
- Greater Involvement of Panchayati Raj Institutions (PRIs), Non-Governmental Organizations (NGOs), and the Community: Fostering collaboration and community participation in healthcare initiatives.
Couple Protection Rate (CPR)
- Definition: The Couple Protection Rate (CPR) measures the percentage of eligible couples protected against childbirth by approved family planning methods such as condoms, oral pills, IUDs, or sterilization.
- Indicator of Contraceptive Prevalence: CPR serves as an indicator of contraceptive prevalence within a community.
- National Reproductive Goal: Demographers believe that a Net Reproduction Rate (NRR) of 1 requires a CPR exceeding 60%. This belief led to the previous National Population Policy aiming for a CPR of 60% by the year 2000
- Effective Couple Protection Rate (ECPR):
- Definition: The Effective Couple Protection Rate (ECPR) represents the percentage of eligible couples effectively protected against childbirth by approved family planning methods.
- Clarification Needed: Further context and explanation are necessary to clarify the significance of ECPR and how it differs from CPR.
IFA Tablets and Iron Deficiency Anemia
- Adult IFA Tablet: Contains 100 mg of elemental iron and 500 mcg of folic acid.
- Pediatric IFA Tablet: Contains 20 mg of elemental iron and 100 mcg of folic acid.
- IFA Tablet for Preterm Infants: Recommended content per tablet is 10–15 mg of elemental iron and 100 mcg of folic acid.
- National Nutritional Anemia Prophylaxis Program: Launched in 1970 to prevent nutritional anemia in mothers and children, now implemented by the Maternal and Child Health Division of the Ministry of Health and Family Welfare as part of the RCH initiative.
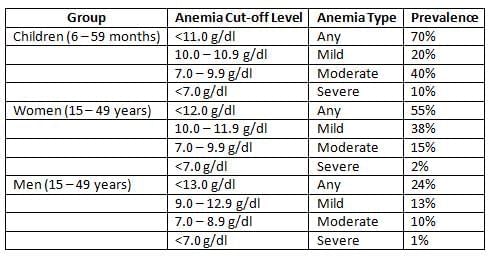
Prevalence of Iron Deficiency Anemia (IDA) in India:
Integrated Management of Neonatal and Childhood Illness (IMNCI)
- IMNCI is a strategy aimed at reducing illness and death associated with major causes of childhood illnesses.
- Curative Component: Includes management of conditions such as
- Diarrhoea
- Pneumonia
- Malaria
- Severe
- Malnutrition
- Nutritional counselling
- Health Promotive and Preventive Component:
- Breastfeeding
- Nutritional counselling
- Vitamin A and Iron supplementation
- Treatment of helminthic infestation.
- Target Group: Children under 5 years, specifically aged 2 months to 5 years.
- Components of IMNCI Strategy:
- Improving case management skills of healthcare staff.
- Enhancing overall health systems.
- Promoting better family and community health practices.
- Case Management Process:
- Assessing the young infant or child
- Classifying the illness
- Identifying the treatment
- Treating the infant or child
- Counselling the mother and Providing follow-up care.
- Indian Adaptation of IMCI: IMNCI includes early neonatal age (0–7 days) in the program and incorporates national guidelines on malaria, anemia, vitamin A supplementation, and immunisation schedule.
- Colour Coding:
- Pink: Pre-referral treatment and urgent referral to hospital.
- Yellow: Specific treatment at PHC.
- Green: Home-based management.
Quality Indicators to Monitor and Evaluate RCH Program
- Number of RTI/STI cases detected, treated, and referred.
- Number of ANC cases registered, both total and those registered before 12 weeks.
- Number of pregnant females with three antenatal checkups.
- Number of high-risk pregnant females referred for additional care.
- Number of pregnant females who received two doses of Tetanus Toxoid (TT) vaccine.
- Number of pregnant females under anemia prophylaxis and treatment.
- Number of ANC cases with complications referred to PHC or FRU.
- Number of deliveries conducted by trained and untrained birth attendants.
- Number of women receiving three post-natal checkups.
- Number of newborns with recorded birth weights.
- Number of children fully immunised as per the schedule.
- Number of adverse effects following immunisation (AEFI) reported.
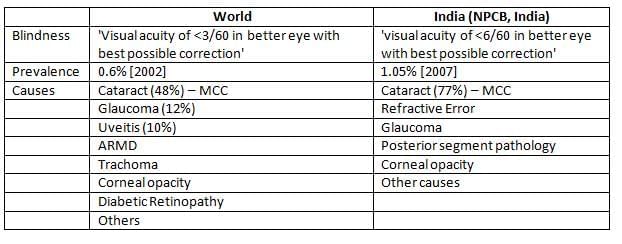
National Program for Control of Blindness (NPCB)
- India has the highest number of blind individuals globally, with an estimated prevalence of 1.05%. The most common cause of blindness is cataract, accounting for 77% of cases.
- The NPCB, launched in 1976, aims to reduce blindness prevalence to 0.5% by 2010.
- Blindness is defined as visual acuity of less than 6/60 in the better eye, with 48% of cases caused by cataracts.
- The NPCB focuses on strengthening eye care services, developing human resources, promoting outreach activities, and enhancing institutional capacity.
Blindness in India
- India is the largest contributor to global blindness, with a current prevalence of 1.05%.
- The state with the highest prevalence of blindness is Jammu & Kashmir, while Meghalaya has the lowest prevalence.
- Blindness prevalence in individuals over 50 years old is 8.5%, and the prevalence of one-eyed blindness is 0.8%, with cataract being the most common cause (73%).
- India is believed to overestimate the number of blind individuals according to WHO definitions. If the WHO cutoff of <3/6 0 in BEBPC) was applied, the estimated prevalence of blindness would be lower.
Blindness in India can be classified into:
- Economic Blindness
- Social Blindness
- Manifest Blindness
- Absolute Blindness
Strategies of National Program for Control of Blindness (NPCB, 1976)
- Strengthening service delivery
- Developing human resources for eye care
- Promoting outreach activities and public awareness
- Developing institutional capacity
- Establishing eye care facilities for every 5 lakh persons
Revised Strategies of NPCB
- Enhance the comprehensiveness of NPCB by addressing:
- Bolstering support for conditions causing blindness, such as corneal blindness and refractive errors among schoolchildren.
- Enhancing follow-up care for individuals who have undergone cataract surgery.
- Managing additional causes of blindness, including glaucoma.
- Strengthen the involvement of voluntary organizations.
- Transition from eye camp methods to a fixed facility surgical approach.
- Improve access to eye care services in tribal and underserved regions.
- Expand World Bank project activities by:
- Building dedicated eye OTs and wards.
- Training eye surgeons.
- Implementing modern cataract surgery techniques.
- Providing ophthalmic equipment.
Organizational Structure for NPCB
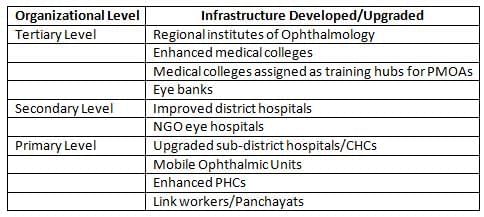
- NPCB was launched in 1976as a '100% Centrally sponsored program'
- India was the first country to launch a national level program for blindness.
- Apex Institute: National Institute of Ophthalmology (Dr. Rajendra Prasad Centre for Ophthalmic Sciences [2007] AIIMS, New Delhi)
- The NPCB defines blindness as a visual acuity of less than 6/60 in the better eye.
- Prevalence of blindness in general population: 1.05% (MCC: Cataract 77%) [2007]
- Cataract surgery rate required to clear the backlog of blindness: 340 operations per lakh population [2007]
- IOL implantations in cataract surgeries: 34% [2007]
- NPCB was launched in 1976as a '100% Centrally sponsored program'
Definition and Causes of Blindness in NPCB
Important Points of Blindness
- Goal for Blindness in National Health Policy (NHP) 2002:
- Reduce the prevalence of blindness to 0.5% by 2010
- About 80% of blindness is avoidable
- Legal Blindness: Visual acuity <6/60 (<20/200) Or Visual field <20° in better Eye with best possible correction.
- Work Vision: <6/60 (Economic)
- Walk Vision: <3/60 (Social Blindness)
School Eye Screening (SES) Program
- Focus on middle school (V -VIII class) covering 10 -14years age
- 150,000 children to be screened per block
- One trained teacher to handle 150 students
- 1 -day training for teacher at nearest PHC
- Teacher Kit: Vision screening cards, referral cards, tape/rope to measure 20 feet
- Visual cut-off for referral to nearest PHC: <6/9 in either eye
- Prerequisites for undertaking SES:
- Availability of Para-medical Ophthalmic Assistant (PMOA)
- Acquisition of relevant ophthalmic equipment
- Engagement of an optician to supply spectacles
Vision 2020- Right to Sight Initiative
- Targets for X Five-Year Plan under Vision 2020:
- Boost cataract surgery rate to 450 operations per one lakh population.
- Enhance visual outcome (>6/18) after cataract surgery in 80% of cases.
- Increase intra-ocular lens (IOL) implantation in over 80% of cataract surgery cases.
- Establish 50 paediatric ophthalmology units in tertiary care hospitals.
- Screen known diabetics for diabetic retinopathy for those over 35 years attending eye clinics.
- Ensure refraction services are available in all districts.
- Set up 4000 vision centers managed by trained optometrists/Refractionists/Ophthalmic Assistants.
- Develop low vision centers at 50 centers of excellence/tertiary centers.
- Replace 25 fully functional, accredited safe eye banks.
- Achieve 75% coverage for regular vitamin A supplementation (till 5 years age)
- International organizations involved in Vision 2020
- WHO
- Orbis
- International Agency for Prevention of Blindness
- International Eye Foundation
- International Federation for Ophthalmological Societies
- International Organization against Trachoma
- Rotary International
- World Blind Union
- National Council of Optometry
- Lions Club International
- Helen Keller International
Cataract Blindness Control Project (CPCB)
- The Government of India secured a soft loan from the World Bank° to address cataract blindness across 7 states from 1994 to 2002.
- Activities undertaken in the project:
- Establishment and operation of District Blindness Control Societies (DBCS).
- Construction of eye theatre/eye wards in district hospitals.
- Provision of ophthalmic equipment.
- Intra-Ocular Lens (IOL) implantation in District Hospitals.
- Training of surgeons in IOL surgery.
- Support to NGOs for establishing eye care facilities.
- Achievements of the project:
- 15.35 million cataract operations performed (Target: 11 million).
- IOL implantation increased from 3% (1998) to 75% (2002).
- 307 dedicated eye units were built and equipped in the Government sector & 30 in the non-government sector.
- 800 eye surgeons trained in IOL surgery.
National AIDS Control Programme (NACP)
3 by 5 Initiative
- People living with HIV/AIDS (PLHA) worldwide: 40 million
- 3 by 5 Target: Introduced by WHO and UNAIDS on December 1, 2003
- Interim target: Aim to provide anti-retroviral treatment (ART) to 3 million PLHA in developing countries by the end of 2005
- Ultimate goal: Achieve universal access to ART for all in need
- Focus areas:(Five pillars)
- Simplified tools for ART delivery
- New services for reliable medicine and diagnostic supply
- Sharing and applying new knowledge and successful strategies
- Urgent support to countries
- Global leadership with strong partnerships
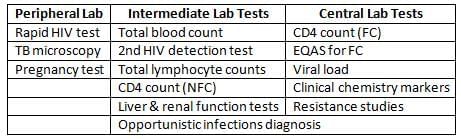
- Role of Laboratories in the 3 by 5 Initiative:
HIV Screening in NACP
- Tests for Screening of HIV: E/R/S Battery
- ELISA (E) Test
- RAPID (R) Test
- SIMPLE (S) Test
- Confirmatory diagnosis of HIV: Western Blot Assay
- Screening strategies of HIV:
- Strategy I: One of the three tests (E/R/S) is used
- Used to screen every blood unit before transfusion
- Not recommended for diagnosing HIV in individuals
- Strategy II: Two of the three tests (E/R/S) are used
- Screening for those with symptoms of AIDS-defining illnesses (NACO guidelines)
- Strategy III: All three tests (E/R/S) are used
- Screening for asymptomatic individuals
- The ELISA Test is the most common first screening test for HIV
- It has high sensitivity.
- Strategy I: One of the three tests (E/R/S) is used
HIV Diagnosis Tests
- Western Blot Assay(Immunoblot):
- Detects specific proteins in tissue samples.
- Used as a confirmatory test for HIV in India.
- Based on detecting:
- Viral core protein (p24)
- Envelope glycoprotein (gp 41)
- Mechanism:
- Gel electrophoresis separates proteins.
- Proteins are transferred to a membrane (nitrocellulose or PVDF).
- Probe detection using specific antibodies.
- Antigen Test: Detects the p24 protein of HIV.
- Nucleic-acid-based tests: Amplify and detect a specific sequence in the HIV gag gene.
- RT-PCR test: Extracts viral RNA, uses reverse transcriptase; PCR is applied for amplification.
- Quantiplex bDNA: Centrifuges plasma, adds oligonucleotides for RNA binding; enzyme reaction allows RNA quantification.
Targeted Interventions in NACP
- Basic purpose: Reduce HIV transmission among vulnerable populations.
- Approach: Comprehensive methods for at-risk groups.
- Main activities:
- Behaviour change
- Treatment of STDs
- Creating an environment that supports behaviour change
- Segments of the population covered:
- Sex workers
- Injecting drug users
- Truck drivers
- Men who have sex with men (MSM)
- Migrant workers
- Street children
Opt-in/Opt-out Testing
- Opt-in testing: Testing is offered, and patients must give permission.
- Opt-out testing: Patients are informed that testing is standard, and they can decline; consent is assumed unless declined.
- WHO and CDC recommend opt-out testing in healthcare settings.
- Opt-out testing has a higher rate (85-98%) than opt-in testing (25-83%).
- It does not remove the need for informed consent.
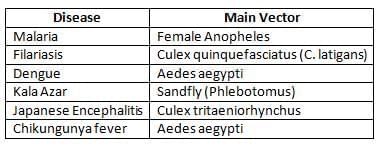
National Vector Borne Disease Control Programme (NVBDCP)
Introduction NNBDCP
- NVBDCP Covers 6 Vector-Borne Diseases° of Public Health Importance in India:
Modified Plan of Operation (MPO)
- The Modified Plan of Operation (MPO) was introduced in 1977 after the malaria eradication attempts were set aside.
- Under the MPO, areas were classified based on the Annual Parasitic Incidence (API)
- Areas with API > 2:
- Regular insecticide spray every 6 weeks
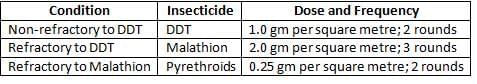
- Conducting entomological studies
- Malaria surveillance
- Treating cases
- Intensifying efforts in rural areas (support under Plasmodium falciparum Containment Programme with SIDA)
- Decentralising lab services to PHC level
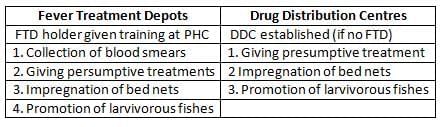
- Establishing Drug Distribution Centers (DDCs) and Fever Treatment Depots (FTDs)
Areas with API < 2:
- Focal spraying with DDT, BHC, or Malathion if a case of Pf occurs in the area
- Active and passive surveillance
- Presumptive treatment for all suspected fever cases
- Ensuring radical treatment for those found positive on blood smear
- Epidemiological investigation of cases to identify causes
Fever Treatment Depots (FTDs) and Drug Distribution Centers (DDCs)
Malaria Diagnosis
- Diagnosis of malaria in NVBDCP (malaria component): Peripheral blood smear
- Two types of smear:
- Thick smear(Sensitivity): Indicates presence of malaria
- Thin smear(Specificity): Used for species identification
- Stain used: JSB (Jaswant Singh Bhattacharaya) Stain
- 1 microscope per 30,000 population in rural areas and 50,000 in urban areas
- Dipstick test in selected areas
- 'Link Worker' per 2000 population in high Pf areas (collects smears, provides presumptive treatment, and sends slides to PHCs)
- Fever Treatment Depot (FTD) in every village.
- Rapid tests for diagnosing Pf:
- Dipstick test (Pf Histidine rich protein II -HRP II)
- Leishman stain
- Field's stain
- Acridine orange
- Dipstick Test is for the rapid diagnosis of Plasmodium falciparum (Pf)
- Optimal Test [Parasite-specific lactic dehydrogenase (LDH dipstick test)]: Positive in P. falciparum and P. vivax parasitaemia; it is simple, rapid, and superior to HRP I.
- 1 microscope per 30,000 population.
Enhanced Malaria Control Project (EMCP)
- World Bank supported project for six crore tribal population in 8 states
- Implemented in 1045 PHCs across 100 districts in 8 states
- Selection criteria for PHCs in EMCP:
- Annual parasitic incidence (API) > 2 in last 3 years
- Pf cases > 30% of all malaria cases
- 25% of the population is tribal
- Area has reported deaths due to malaria (with flexibility to direct resources to areas in need during outbreaks)
- Objectives of EMCP:
- Reduction of malaria morbidity
- Prevention of malaria mortality
- Consolidation of gains achieved so far
- Important strategies of EMCP:
- Early case detection and prompt treatment (EDPT):
- Link worker (1 per 2000 population)
- Microscopy
- Dipstick test
- FTD
- Early case detection and prompt treatment (EDPT):
- Selective vector control:
- Introduction of larvivorous fishes
- Use of biocides - Bacillus thuringiensis H14
- Environmental management
- Residual spray in areas with > 1 case of Pf
- Personal protection:
- Insecticide treated bednets (ITBN).
Insecticide Treated Bed Nets (ITBN)
- ITBN Programme (especially deltamethrin) has led to a significant decline in malaria incidence and API
- Average decline in anopheline mosquito density - 68%
- Average decline in culicine mosquito density - 50%
- Chemicals used in ITBN Programme: Synthetic pyrethroids
- Deltamethrin: 2.5% at a dosage of 25 mg/m²
- Cyfluthrin: 5% at a dosage of 50 mg/m²
- Other Insecticides Used:
- Permethrin
- Lambdacyhalothrin
- Etofenprox
- Cypermethrin
- Effectiveness of Pyrethroids:
- Lasts for 6 - 12 months (Retreatment every 6 months )
- Long-lasting Insecticidal Mosquito Nets (LLINs)
- Use pyrethroid insecticides and a chemical binder.
- Can be washed over 20 times, allowing use for over 3 years.
- Household Bed Nets Used for Mosquito Control:
- The number of holes per square inch should exceed 150.
- Diameter of each hole <>0.0475.
- Common Insect Repellents:
- DEET (N, N-diethyl-m-toluamide)
- Allethrin
- Essential oil of lemon eucalyptus (p-menthane-3, 8-diol (PMD) )
- Icaridin (picaridin)
- Nepetalactone (catnip oil)
- Citronella oil
- Soybean oil
- Neem oil
Types of Drug Resistance in Malaria
- R1 resistance: Infection reappears between 7-28 days after treatment ends, following initial symptom relief and parasite clearance.
- R2 resistance: Patients see a significant drop in parasite count (over 75%. at 48 hours, but parasites remain by day 7.
- R3 resistance: Parasite count does not drop by more than 75% within 48 hours or may even increase by day 7.
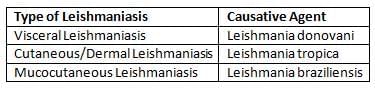
NVBDCP: Leishmaniasis
Introduction to Leishmaniasis
- Leishmaniasis (Kala azar) is a group of diseases caused by Leishmania:
- Kala Azar Transmission:
- Transmitted by female Phlebotomus argentipes (sandfly).
- Sandflies mainly hop instead of flying.
- They rest in cracks and crevices of walls.
- Insecticide of Choice:
- Historically, DDT was used; it is now banned in many countries due to environmental issues.
- Recommended spray height is up to 6 feet on walls.
- If resistant to DDT, use BHC.
Sandfly
- Kala Azar is also known as 'Black Sickness'.
- It is transmitted by female Phlebotomus argentipes (sandfly).
- Sandflies are vectors for:
- Visceral Leishmaniasis (Kala Azar)
- Cutaneous Leishmaniasis (Oriental Sore)
- Sandfly Fever
- Oroya Fever
- Sandflies inject the infective stage, metacyclic promastigotes, during blood meals.
DDT
- DDT stands for Dichloro-Diphenyl-Trichloroethane.
- Synthesised by Othmar Zeidler in 1874.
- Insecticidal properties discovered by Swiss scientist Paul H. Muller in 1939 (awarded the 1948 Nobel Prize in Physiology and Medicine).
- Positive associations have been found with liver, biliary tract, and breast cancers
Tests for Leishmaniasis
- Parasitological diagnosis: LD bodies in aspirates from spleen, liver, bone marrow, lymph nodes, or skin.
- Hematological diagnosis: Progressive leucopenia, anemia, altered albumin:globulin ratio (raised IgG).
- Aldehyde Test of Napier: Previously used for diagnosis; better for surveillance.
- Non-specific test requiring venous blood.
- Detects raised globulins.
- False positives can occur in chronic conditions with reversed albumin: globulin ratio
- Serological Tests:
- rK-39 Dipstick test: For Visceral Leishmaniasis (Kala Azar).
- IFAT
- Direct Agglutination Test
- Leishmanin (Montenegro) Test:Tests immunity status.
- 1 ml (intradermal) washed promastigotes on the forearm.
- Read after 48-72 hours.
- Induration > 5 mm is positive.
Treatment of Kala Azar
- 1st Line: Sodium stibogluconate (i/v or i/m) 20 mg/kg for 20 days (antimonial compounds).
- 2nd Line: Pentamidine (i/v) 3 mg/kg for 10 days.
- 3rd Line: Amphotericin-B (i/v) 1 mg/kg for 20 days (now the preferred treatment in many countries).
- Other drugs:
- Ketoconazole
- Allopurinol
- Paramomycin
- Mepacrine (for dermal leishmaniasis)
- New Wonder Drug: Miltefosine (oral) 2.5 mg OD for 4 weeks (now second line treatment).
National Rural Health Mission (NRHM)
Core Strategies of NRHM
- Enhance the skills of Panchayati Raj Institutions (PRIs) through training.
- Improve household-level healthcare access by recruiting and training ASHAs (Accredited Social Health Activists).
- Develop a health plan for each village with the Village Health Committee.
- Strengthen sub-centres with untied funds.
- Support existing Primary Health Centres (PHCs) and Community Health Centres (CHCs), ensuring 30-50 bedded CHCs per lakh population, as per Indian Public Health Standards (IPHS).
- Implement an intersectoral District Health Mission.
- Improve data collection and assessment capabilities for effective planning and monitoring.
- Formulate clear policies for developing human resources in healthcare.
- Enhance preventive healthcare skills at all levels.
- Promote safe motherhood through the Janani Suraksha Yojana (JSY) by encouraging institutional deliveries among poor pregnant women.
- Encourage the non-profit sector, especially in underserved areas.
Key Strategies of NRHM
- The NRHM (2005-12) aims to provide every village with a trained female community health activist, known as ASHA (Accredited Social Health Activist).
- Develop a "Village Health Plan (VHP)" for each village through the Village Health Samiti (Panchayat Health Sub-Center).
- ASHA will collaborate with ANM (Auxiliary Nurse Midwife), Anganwadi Workers, and community workers to create the VHP under the guidance of the Panchayat Health Sub-Center.
- Prepare an "Intersectoral District Health Plan (DHP)" addressing drinking water, sanitation, hygiene, and nutrition, developed by the District Health Mission (DHM).
- DHP will integrate local responses from VHPs with state and national health priorities.
- Health plans will be the core unit for proposed actions, with implementing departments integrated into DHM for effective monitoring.
- Planning, budgeting, and implementation will be centralized at the District level.
Accredited Social Health Activist (ASHA)
- Proposed population norm: ASHA worker per 1000 individuals.
- ASHA serves as:
- The link between the community and the healthcare system.
- A bridge between ANM and the village.
- Accountable to the Panchayat.
- Selection criteria for ASHA:
- A woman resident of the local community.
- Aged preferably between 25-45 years.
- Literate with formal education up to VIII class.
- Responsibilities of ASHA:
- Raise awareness about health and its social factors, mobilising the community for local health planning and using existing health services.
- Promote good health practices and provide basic care as needed, making timely referrals.
- Share information about health determinants, existing services, and the importance of timely access.
- Counsel women on reproductive and child health matters.
- Help the community access government health services.
- Store essential items like ORS, IFA tablets, and delivery kits.
- Provide primary medical care and act as a DOTS provider.
- Assist in developing a comprehensive village health plan.
- Accompany pregnant women and children needing treatment to health facilities.
- Participate in JSY (Janani Suraksha Yojana) to help reduce maternal mortality rate (MMR).
- Training resource person for ASHA: ANM and Anganwadi worker.
- Other roles of Anganwadi worker integrated with ASHA:
- Organise Health-Day.
- Conduct IEC activities.
- Store and issue supplies to ASHA.
- Update the list of eligible couples and children.
- Mobilise for food supplementation.
- Other roles of ANM worker integrated with ASHA:
- Organise meetings with ASHA.
- Guide and participate in organising Health-Day.
- Update the eligible couple register.
- Encourage pregnant women to seek antenatal care.
- Educate ASHA on warning signs during pregnancy.
- Orient ASHA on oral contraceptive pills (OCPs).
Indicators for Monitoring and Evaluation of ASHA's Work
- Process indicators:
- Number of ASHAs selected.
- Number of ASHAs trained.
- % of ASHAs attending review meetings after 1 year.
- Outcome indicators:
- % of newborns weighed and families counselled.
- % of deliveries with skilled assistance.
- % of institutional deliveries.
- JSY Claims Made to ASHA
- Completed Immunization for Ages 12-23 Months
- Unmet Need Percentage in Below Poverty Line (BPL) Households
- Percentage of Fever Cases Treated with Chloroquine Within One Week in Endemic Areas
- Impact Indicators:
- Infant Mortality Rate (IM )
- Child Malnutrition Rates
- Number of Tuberculosis (TB) and Leprosy Cases Detected Compared to the Previous Year
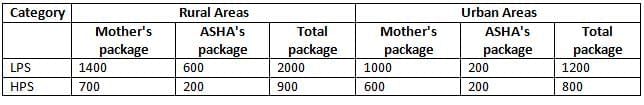
Janani Suraksha Yojana (JSY)
- Launched: 12th April 2005
- The Janani Suraksha Yojana (JSY) is an improved version of the National Maternity Benefit Scheme.
- Objectives of JSY:
- To lower maternal and infant death rates by promoting hospital deliveries and care, focusing on poor women.
- Key Features of JSY:
- Fully funded by the central government.
- Offers cash support along with institutional care.
- Eligibility for Cash Assistance:
- In Low Performing States (LPS): All women having institutional deliveries.
- In High Performing States (HPS): Women below the poverty line (BPL) aged 19 and above, and Scheduled Caste (SC) or Scheduled Tribe (ST) pregnant women.
- Limitations on Cash Assistance
- In Low Performing States (LPS): Cash assistance is available for all births in institutions.
- In High Performing States (HPS): Cash assistance is limited to up to 2 live births.
- JSY Package: New Guidelines
New Initiatives
- Home Delivery of Contraceptives by ASHA
- District Level Household Survey (DLHS-4) in 26 States/UTs
- Promotion of Menstrual Hygiene in 152 Districts
- Differential Financial Approach for Targeted Assistance
- ASHA Involvement in Home-Based Newborn Care (HBNC)
- Performance-Based Fund Allocation to States
- Village Health, Sanitation, and Nutrition Committee (VHSNC)
- Mainstreaming of AYUSH (Ayurveda, Yoga, Unani, Siddha, and Homeopathy)
Janani-Shishu Suraksha Karyakram (JSSK)
- Pregnant Women:
- Free Deliveries, Including Caesarean Sections, in Public Health Institutions
- Free Drugs and Consumables
- Free Diet for 3 Days After Normal Delivery and 7 Days After Caesarean Section
- Free Diagnostics
- Free Blood Transfusions When Necessary
- Free Transport from Home to Institution
Child Health:
- Nutritional Rehabilitation Centers (NRCs) for Severely Malnourished Children and Maternal Counselling
- Integrated Management of Neonatal and Childhood Illnesses (IMNCI) for Common Childhood Illnesses
- Pre-Service IMNCI Training Included in Medical Curriculum
- Facility-Based IMNCI (F-IMNCI) for Major Causes of Neonatal and Childhood Mortality
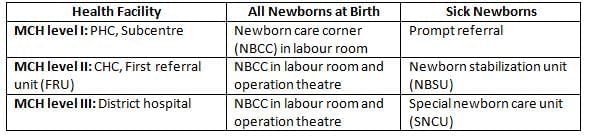
- Newborn care corner (NBCC): A designated space within the delivery room in all health facilities for immediate care of newborns.
- Newborn stabilization unit (NBSU): Facilities within or near maternity wards where sick and low birth weight newborns can be cared for over short periods.
- Location: CHCs, FRUs.
- Space required: 4 bedded unit and 2 beds for post-natal ward for rooming-in.
- Special newborn care unit (SNCU): Neonatal unit near labour room to provide specialized care for sick newborns (EXCEPT assisted ventilation, major surgery).
- Location: District hospitals, Sub-district hospitals with >2000 deliveries per year.
- Space required: 12 bedded unit and 4 additional beds for adult step-down care.
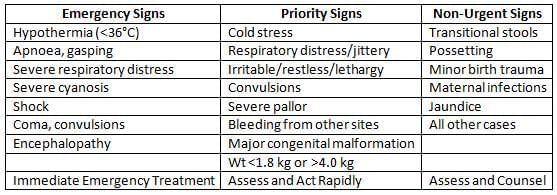
- Triage of Sick Newborns:
- Home-Based Newborn Care (HBNC):
- Main Person Involved: ASHA (Accredited Social Health Activist)
- Other Health Personnel: ANM (Auxiliary Nurse Midwife), Anganwadi Worker, Medical Officer
- ASHA Visits in Institutional Deliveries: Day 3, 7, 14, 21, 28, 42
- ASHA Visits in Home-Based Deliveries: Day 1, 3, 7, 14, 21, 28, 42
- Other Functions of ASHA (Paid ₹ 250/-)
- Record birth weight
- Administer BCG, OPV, and DPT vaccines to newborns
- Register births
- Ensure safety for mothers and newborns until 42 days
- Navjat-Shishu Suraksha Karyakram (NSSK)
National Leprosy Elimination Programme (NLEP)
Multidrug Therapy (MDT)
- Drugs Used in Leprosy Treatment:
- Rifampicin: Kills 99.9% of leprosy bacteria (600 mg dose).
- Clofazimine: Best used daily; inhibits bacterial growth.
- Dapsone: Safe in doses up to 100 mg.
- Other Effective Drugs:
- Thioamides: Ethionamide & Prothionamide
- Fluoroquinolones
- Minocycline
- Macrolides
Treatment of Single Skin Lesion (SSL) of Leprosy:
- Previously: Rom therapy
- Rifampicin 600 mg
- Ofloxacin 400 mg
- Minocycline 100 mg
- Currently: 6-month treatment like for Paucibacillary (PBL) Leprosy (Rifampicin and Dapsone for 6 months).
Lepra Reactions
- Lepra Reactions: Inflammation affecting skin patches, nerves, eyes, and sometimes internal organs.
- They can occur at any time in a leprosy patient:
- Before diagnosis
- At the time of diagnosis
- During treatment
- After treatment has finished
Types of Lepra Reactions:
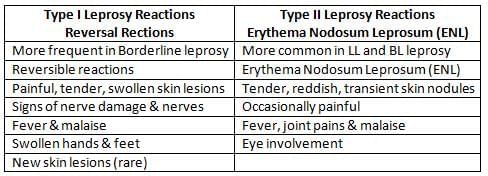
Treatment of Lepra Reactions:
- Type I (Reversal) Reactions: Prednisolone (steroid)
- Type II (ENL) Reactions:
- Mild cases: Analgesics or antipyretics like aspirin
- Severe cases: Prednisolone (steroid)
- During steroid withdrawal: Clofazimine
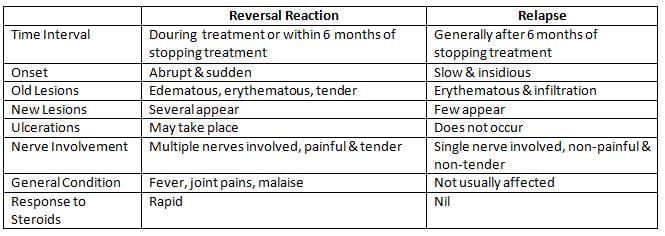
- Reversal Reaction Versus Relapse
Infrastructure Norms under NLEP
- SET Centre: One per 20,000 - 25,000 population
- Urban Leprosy Centre (ULC): One per 50,000 population
- Leprosy Control Unit (LCU): One per 4.5 lakh population
Survey Education and Treatment (SET) Centre
- A SET Centre is attached to: PHC in rural areas
- Administrative control: Medical Officer (PHC)
- Population catered: 20,000 - 25,000
- Staff: One paramedical worker
- Functions:
- Early detection of cases through house-to-house surveys
- Health education about leprosy
- Free treatment for all cases and follow-up
- Contact tracing and chemoprophylaxis with Dapsone
Simplified Information System (SIS)
- Description: Management and Information System for monitoring and evaluating NLEP; initiated in 2002.
Indicators of SIS under NLEP:
- Prevalence rate of leprosy
- New case detection rate
- Child proportion among new cases
- Visible deformed case proportion among new cases
- Multibacillary Leprosy (MBL) proportion among new cases
- Female proportion among new cases
- New case detection rate in Scheduled Castes
- New case detection rate in Scheduled Tribes
- Patient month blister calendar packs stock
- Proportion of health subcenters providing MDT (Multidrug Therapy)
- Absolute number of patients made RFT (Released from treatment)
Newer Initiatives Under NLEP
- Focussed Leprosy Elimination Plan (FLEP) 2005:
- Priority areas: Prevalence > 3 per 10,000
- Increased efforts on IEC, training, and integrated service delivery
- Week-long 'Block Leprosy Awareness Campaign'
- SAPEL and LEC:
- Special Action Projects for Elimination of Leprosy (SAPEL) in rural areas
- Leprosy Elimination Campaigns (LEC) for urban areas:
- To cover populations in difficult/inaccessible areas not generally reached by regular programme activities.
Objective:
The programme aims to support patients who need to temporarily halt their treatment for preventable reasons.
It is particularly advantageous for patients with inconsistent attendance.
- Upon diagnosis, patients can receive the complete MDT course after appropriate counselling.
New Indicators for Leprosy Control
- Operational Indicators:
- Monitor the effectiveness of control activities.
- Include metrics such as:
- Number of new cases detected.
- New cases with grade 2 disability per 100,000 population.
- Treatment completion and cure rate.
- Case Detection Indicators:
- Percentage of children (0-14 years) among new detected cases: A high rate indicates active transmission.
- Percentage of females among new detected cases.
- Percentage of Multi-bacillary cases on regular treatment.
- Percentage of new cases with grade 2 disability.
- Quality of Service Indicators:
- New cases percentage correctly diagnosed.
- Number of relapses.
- Percentage of treatment defaulters.
- Percentage of patients developing new disability during MDT.
- Epidemiological Indicators:
- Assess programme effectiveness.
- Include metrics for measuring transmission and case load.
- Useful for planning treatment services.
|
40 docs|6 tests
|
FAQs on National Health Programmes, Policies and Legislations in India - 1 Chapter Notes - Preventive and Social Medicine (PSM) - NEET PG
| 1. What is the primary objective of the National Program for Control of Blindness (NPCB)? |  |
| 2. How does the National HIV/AIDS Control Programme (NACP) aim to address the HIV/AIDS epidemic in India? |  |
| 3. What are the key components of the National Vector Borne Diseases Control Programme (NVBDCP)? |  |
| 4. What initiatives are taken under the National Leprosy Elimination Programme (NLEP)? |  |
| 5. How does the National Iodine Deficiency Disorders Control Program (NIDDCP) contribute to public health? |  |















