NEET PG Exam > NEET PG Notes > Preventive and Social Medicine (PSM) > Chapter Notes: Preventive Obstetrics, Paediatrics and Geriatrics
Preventive Obstetrics, Paediatrics and Geriatrics Chapter Notes | Preventive and Social Medicine (PSM) - NEET PG PDF Download
| Table of contents |

|
| MCH |

|
| MCH Indicators |

|
| Breast Feeding |

|
| Growth and Development |

|
| School Health |

|
| ICDS, IMNCI, BFHI |

|
| Neonatal Screening |

|
| Geriatrics |

|
| Miscellaneous |

|
MCH
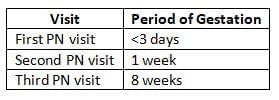
Ante-natal and Post-natal Visits (RCH Program)
- Ideal recommended antenatal visits: 13 - 14
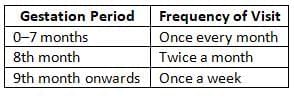
- Minimum recommended antenatal visits: 3
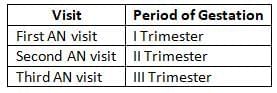
- Minimum recommended antenatal visits (If one visit per trimester is not possible): 3

- Minimum recommended postnatal visits: 3
At Risk Approach
- The at-risk approach aims to identify high-risk antenatal mothers and infants early on while ensuring appropriate care for all.
- At-risk infants are those who may face perinatal, neonatal, and infant mortality and require special intensive care.
- The basic criteria for identifying at-risk infants include:
- Birth weight: Less than 2.5 kg (low birth weight)
- Multiple births: Twins or higher-order multiples
- Birth order: Greater than 5
- Feeding method: Artificial feeding
- Weight: Less than 70% of expected weight
- Failure to thrive: Not gaining weight for three consecutive months
- Medical conditions: Protein-energy malnutrition (PEM) or diarrhea
- Family circumstances: Working mother or single parent
- At-risk mothers are identified based on the following criteria:
- Age: Elderly primipara (over 30 years)
- Height: Short-statured primipara (under 140 cm)
- Fetal position: Malpresentations such as breech or transverse lie
- Energy requirements: Increased energy needs during pregnancy and lactation
- Medical issues: Antepartum hemorrhage, threatened abortion, preeclampsia, eclampsia, anemia, diabetes, tuberculosis, and other general diseases
- Previous complications: History of stillbirth, intrauterine death (IUD), manual removal of placenta, or previous cesarean section or instrumental delivery
- Parity: Elderly grandmultipara (over 5 previous births)
- Prolonged pregnancy: More than 14 days past the estimated due date (EDD)
- Multiple pregnancies: Twins or hydramnios
- Danger signals during labor are used to identify mothers who need to be transferred to the nearest primary health centre (PHC).
- These signals include:
- Labor progress: Sluggish or absent contractions after rupture of membranes, or no progress after rupture of membranes
- Fetal distress: Prolapse of hand or cord, meconium-stained amniotic fluid, or abnormal fetal heart sounds
- Maternal complications: Excessive vaginal bleeding, collapse during labor, or elevated temperature (above 38°C)
- Postpartum complications: Incomplete separation of the placenta within half an hour after delivery, postpartum hemorrhage (PPH), or collapse
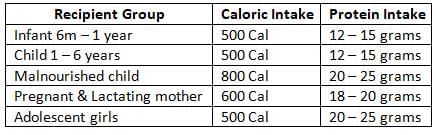
Nutritional Requirements
- Recommended daily energy intake: [New Guideline 2011]
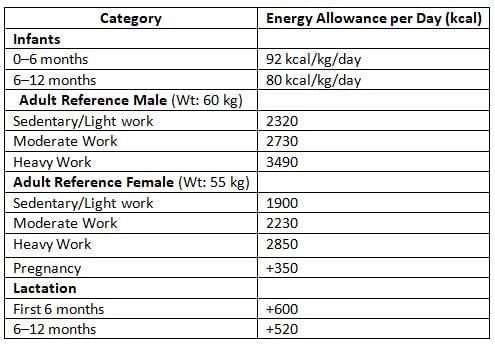
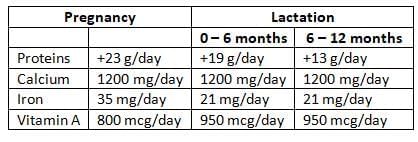
- Requirements in Pregnancy and Lactation:
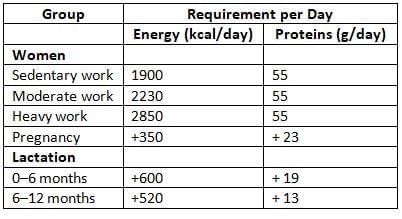
- Other requirements in pregnancy and lactation:
Cleans of Safe Delivery
- The 'Five cleans' practices under strategies for eliminating neonatal tetanus include:
- Clean delivery surface
- Clean hands (of birth attendants)
- Clean cord cut (blade or instrument)
- Clean cord tie
- Clean cord stump
- Procedures undertaken to ensure 5 cleans:
- Clean delivery surface: A clean plastic sheet
- Clean hands: Soap and clean water
- Clean cord cut: A new razor blade
- Clean cord tie: A clean piece of thread
- Clean cord stump: Nothing to be applied to cord
- Sometimes these practices are called '3 cleans':
- Clean cord care (cut, tie and stump)
- Suggested 'Seven Cleans'(Including Five Cleans)
- Sterilized delivery area Washed hands (of delivery assistants)
- Sanitized umbilical severance (knife or tool)
- Sterile umbilical binding
- Disinfected umbilical remnant (no ointment)
- Pure water
- Fresh cloth
- For hand cleansing
Iron and Folic Acid (IFA) Tablets
- Adult Tablet:
- 100 mg of elemental Iron
- 500 mcg of Folic acid (to be taken for at least 100 days during pregnancy)
- Schedule: 1 Tablet per day for 4-5-6 months of pregnancy (Total 100 tablets)
- Pediatric Tablet:
- 20 mg of elemental Iron
- 100 mcg of Folic acid (to be given for at least 100 days every year until the child is 5 years old)
Birth Weight and Its Importance
The birth weight of an infant is the most crucial factor determining its chances of survival, healthy growth, and development.
- Single best measure to assess physical growth: Weight
- Measurement Timing: Birth weight should preferably be measured within the first hour of life.
- Average Birth Weight in India: 2.8 kg (range: 2.7 - 2.9 kg)
- Low Birth Weight (LBW) Causes: Most cases of LBW in India are due to maternal malnutrition linked to fetal growth issues.
- Maternal Nutrition Impact: There is a linear relationship between maternal nutrition and birth weight.
- Smoking Effect: Smoking during pregnancy reduces birth weight by an average of 170 grams.
- Vaccination Guidelines: LBW is not a barrier for vaccinations, except for the Hepatitis B vaccine, which is not recommended for preterm infants with a birth weight below 2.0 kg.
- Growth Chart: Weight and Age
- Plotting: Growth chart is plotted between Weight and Age
- Milestones: Birth weight doubles at 5 months, triples at 1 year, and quadruples at 2 years.
Field Instrument for Measuring Birth Weight:

Low Birth Weight (LBW)
- Definition: Low Birth Weight (LBW) is defined as a birth weight of less than 2500 grams (<2.5 kg), which includes both pre-term (<37 weeks POG) and full-term (>37 weeks POG) babies.
- Global and National Prevalence: LBW occurs in 15% of births globally and 28%in India.
- Lowering LBW Cutoff: If the LBW cutoff is lowered to 2.0 kg, the expected prevalence in India would be 5.5%.
- Gestational Age:LBW is not related to gestational age.
- Measurement Guidelines: LBW percentages should be based on measurements of at least 500 babies.
- Risk Factors for LBW:
- Malnutrition
- Infection
- Unregulated fertility
- Historical Goal: The National Health Policy of 1983 aimed to reduce LBW to less than <10% by the year 2000.
Babies by Gestational Age:
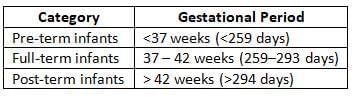
- Reduced infant mass: Under 2500 grams regardless of development stage
- Early-born infants: Delivered prior to 37 weeks of pregnancy
- Premature infants: Arrived before 37 weeks of gestation
- Small-for-Date (SFD) Babies:
- Definition: Small-for-Date (SFD) babies are those born at term or post-term, weighing less than the 10th percentile for their gestational age.
- Cause: SFD is often due to intrauterine growth restriction (IUGR).
- Risk: SFD babies have a high risk of dying during the neonatal and infancy periods.
MCH Indicators
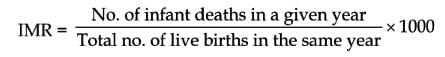
Infant Mortality Rate (IMR)
- IMR is a critical measure of a country's socio-economic development and community health.
- It is calculated as the number of infant deaths in a year per 1000 live births in the same year:
- Child death percentage (CDR) ranks as the PENULTIMATE measure of societal advancement for a nation²
- Top measure of societal progress: Early childhood mortality percentage (ECMR)
- CDR serves as the primary gauge of
- Wellness condition of a population
- Standard of existence:
- Efficacy of maternal-child healthcare services overall
- The child death percentage stands among the finest indicators of governmental collapse
- Child death percentage (CDR):
- Child demise proportion (CDR) reflects a ratio
- Child loss accounts for 18% of total fatalities in India
- Main contributors to CDR in India: Reduced birth weight and early delivery
- Key factors of CDR globally: Lung infection
- IMR (India): 42 per 1000 live births (MP: 56; Goa: 10) [2013]
- IMR (Global): 42 per 1000 live births (Monaco: 1.8; Afghanistan: 122) [2012]
- Target in National Population Plan 2000: 30 per 1000 live births by 2010
- Target in National Wellness Strategy 2002: 30 per 1000 live births by 2010
Factors Influencing IMR
- Various factors affect the Infant Mortality Rate (IMR), including:
- Biological Factors:
- Birth Weight: Infants weighing less than 2.5 kg or more than 4.0 kg have higher IMR.
- Age of Mother: Mothers under 19 or over 35 years old have higher IMR.
- Birth Order: Firstborns have the highest IMR, which decreases for the second child and then increases from the third child onwards.
- Birth Spacing: Wider birth spacing reduces IMR.
- Multiple Births: IMR increases with multiple births (twins, triplets, etc.).
- Family Size: Larger families tend to have higher IMR.
- High Fertility: Higher fertility rates are associated with increased IMR.
- Economic Factors: IMR is generally higher in lower socio-economic status (SES) groups.
- Cultural and Social Factors:
- Earlier weaning and bottle-feeding in poor conditions contribute to higher IMR.
- Care practices influenced by religion and caste can affect IMR.
- Teenage pregnancies are associated with higher IMR.
- Other Factors:
- IMR is higher for girls compared to boys.
- Good quality mothering is linked to lower IMR.
- Poor healthcare significantly increases IMR.
- Higher maternal education is associated with lower IMR.
- Broken families and illegitimacy can lead to increased IMR.
- Unhealthy practices, such as not feeding colostrum or applying cow dung to the newborn, raise IMR.
- Untrained midwives can contribute to higher IMR.
- Poor environmental sanitation is linked to higher IMR.
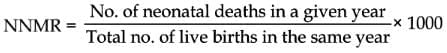
Neonatal Mortality Rate (NNMR)
- NNMR is calculated as the number of neonatal deaths (within 28 days of birth) per 1000 live births in a given year.
- Initial newborn demise (IND): Infant loss within initial seven days of existence
- Subsequent newborn demise (SND): Infant loss within second to fourth week (8–28 days of life)
- NNMR (calculated as ratio per 1000 live births and gestational period)
- MCC of NNMR in India: Early delivery
- MCC of NNMR: Prematurity and related conditions
- Reasons for NNMR:
- Reduced birth mass and premature arrival
- Wound infection
- Congenital disorders
- Issues with placenta and umbilical connection
- Acute respiratory illnesses
- Pneumonia
Maternal Mortality Rate (MMR)
- MMR measures the number of maternal deaths per 100,000 live births. A maternal death is defined as the death of a woman during pregnancy, delivery, or within 42 days of the end of a pregnancy, due to any cause related to the pregnancy.
- MMR is expressed per 100,000 live births to provide clearer values and to account for variations in birth rates.
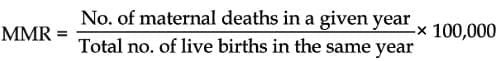
- Worldwide MMR: 251 per 100,000 live births
- MMR in India (2011): 212 per 100,000 live births
- Causes of Maternal Mortality
- Globally:
- Hemorrhage: 25%
- Indirect causes: 20%
- Infection: 15%
- Unsafe abortion: 13%
- Eclampsia: 12%
- Obstructed labour: 8%
- In India (SRS 2001-03):
- Hemorrhage: 38%
- Other conditions: 34%
- Sepsis: 11%
- Abortion: 8%
- Obstructed labour: 5%
- Hypertensive disorders: 5%
- Millennium Development Goal (MDG): The MDG aimed to reduce maternal mortality by three-fourths by 2015.
- RHIME Method:
- RHIME (Representative, re-sampled, routine household interview of mortality, with medical evaluation) is an improved method for estimating MMR in India, introduced in the 2003 Sample Registration System (SRS).
- It is a more refined version of verbal autopsy, enhancing the accuracy of maternal mortality data collection.
Child Mortality Rate, Child Mortality Rate (CMR)
- CMR, also known as Under 5 Mortality Rate (USMR), is calculated as:
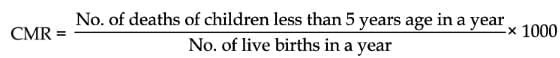
- USMR (India): 59 per 1000 live births (2010)
- U5MR (World): 51 per 1000 live births (2011)
- Leading Causes of U5MR or CMR:
- Pneumonia: 19%
- Diarrhoea: 17%
- Malaria: 8%
- Neonatal Conditions:
- Infections: Most common neonatal condition leading to U5MR
- Preterm births
- Asphyxia
Child Death Rate (CDR)
- CDR is calculated as:
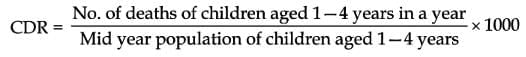
- CDR (India): 3.6% of total deaths (2010)
- MMC CDR Developing Countries: Diarrhoeal diseases and respiratory infections
- MMC CDR Developed Countries: Accidents
- Millennium Development Goal (MDC) 4:
- The goal was to reduce child mortality by two-thirds by 2015.
- UNICEF considers U5MR or CMR as the single best indicator of socio-economic development and well-being.
Child Survival Rate (CSR) Child Survival Index
- Also known as the Child Survival Index, is calculated as:
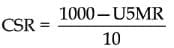
CSR (India): 93.7 [2010]
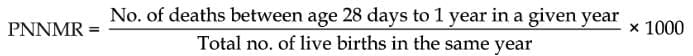
Post Neonatal Mortality Rate (PNNMR)
- Post Neonatal Mortality Rate (PNNMR) measures the number of neonatal deaths (deaths within 28 days after birth) per 1000 live births in a given year.
- It is calculated as:
Perinatal Mortality Rate
- Perinatal Mortality rate (PNMR) includes late fetal deaths (stillbirths) and early neonatal deaths.
- It is calculated as:
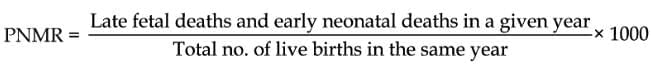
- The perinatal period is defined as 28 weeks of gestation to the 7th completed day of life, although the WHO definition is from 22 completed weeks of gestation to the 7th completed day of life.
- PNMR is the sum of fetal mortality and neonatal mortality and is a key indicator for assessing healthcare quality.
- PNMR (India): 32 per 1000 live births (2010)
- P Catalog (ICD 10): 100 factors of prenatal death and illness
Breast Feeding
WHO Guidelines for India
- The World Health Organization (WHO) recommends exclusive breastfeeding for the first six months of life in developing countries.
- The WHO also advises continuing breastfeeding for at least two years in developing countries.
Nutritional Importance of Breast-milk
- Energy content of breast milk: 60-70 Kcal/100 ml.
- Protein content of breast milk: 1.1 grams/100 ml.
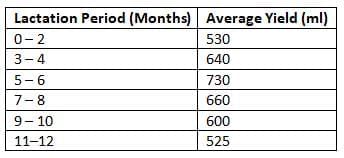
- Mean Output of Breast Milk per Day (ml):
Nutritive Values of Milk (per 100 g):
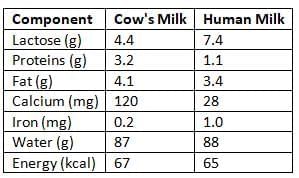
- Human milk has more carbohydrates (lactose), iron, and water, while cow's milk is higher in fat, protein, calcium, and energy.
- Human milk proteins contain more cystine and taurine, less methionine, and are easier to digest than cow's milk proteins.
- Human milk fats have higher levels of PUFAs, especially linoleic acid and alpha-linoleic acid, making them easier to digest and absorb.
- Human milk is richer in vitamins A, C, and contains more copper, cobalt, and selenium.
- It has a higher bioavailability of iron and a better calcium/phosphorus ratio, with lower sodium content.
- Comparative Contents of Nutrients in Different Types of Milk:
- Fat content: Buffalo > Goat > Cow > Human
- Protein content: Buffalo > Goat > Cow > Human
- Energy content: Buffalo > Goat > Cow > Human
- Lactose content: Human > Buffalo > Goat > Cow
Colostrum
- Colostrum is the best food for a newborn, with regular milk arriving 3-6 days after birth.
- Also called 'Beestings', 'First milk', or 'Immune Milk'.
- It is high in carbohydrates, protein, and antibodies, but low in fat.
- Contains all five immunoglobulins: IgA, IgD, IgE, IgG, and IgM.
When Breast feeding Might Harm the Infant:
- Infants with classic galactosemia.
- Mother has untreated pulmonary tuberculosis.
- Mother is on certain medications that suppress the immune system.
- Mother has had excessive exposure to heavy metals like mercury.
- Mother is HIV positive.
- Mother uses harmful substances like cocaine, heroin, and amphetamines.
- Infants classified as 'Underweight' due to acute or chronic malnutrition.
Growth and Development
Indicators of Malnutrition
- Indicators of malnutrition include:
- The best way to assess physical growth is through weight and the rate of weight gain.
- The most sensitive measure of growth is weight.
- The most reliable measure of health and nutrition status is also weight.
- Weight for height is more important than just weight for measuring physical growth.
- Height provides a stable measure of growth, unlike body weight.
- Weight reflects only current health status.
- Height indicates past growth events.
- Acute and Chronic Malnutrition:
- Low weight for age is termed as 'Underweight' (Acute + Chronic Malnutrition).
- Low weight for height is called 'Nutritional wasting' or 'Emaciation' (Acute Malnutrition).
- Low height for age is known as 'Nutritional stunting' or 'Dwarfing' (Chronic Malnutrition).
- Age Independent Parameters for Growth Assessment:
- Mid arm circumference ( MAC ).
- Thickness of subcutaneous fat.
- Body ratios.
- Weight: Height.
- MAC: Head circumference.
Gomez Classification of Malnutrition:
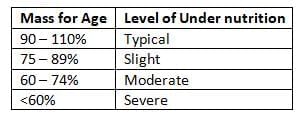
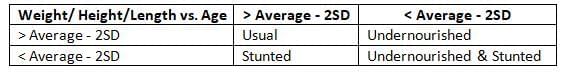
Waterlow Classification:
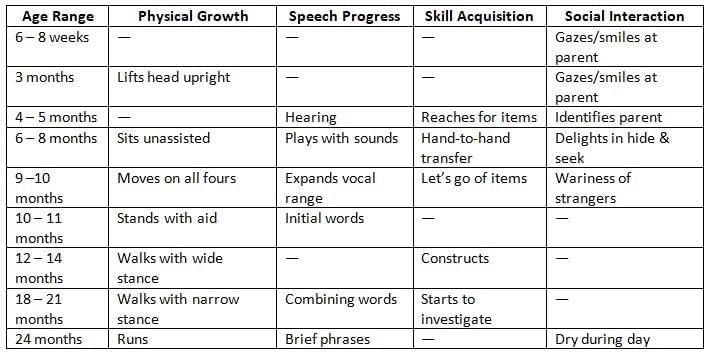
Milestones of Development:
Growth and Weight Patterns
- In India, 2.8 Kg (2.7 - 2.9 Kg).
- Low Birth Weight (LBW): BW < 2.5 Kg
- LBW in India: 28%
- Body weight doubles by 5 months, triples by 1 year, and quadruples by 2 years of age.
- Expected minimum weight gain per month: 500 grams.

Height Increase Patterns in Children
- Average birth length in India: 50 cms.
- Birth length doubles at: 4 years of age.
- Height increments:

- Final Height Attainment:
- Indian boys reach 98% of their final height by 17.75 years.
- Indian girls reach 98% of their final height by 16.5 years.
Growth Charts
- A Growth Chart (Road-to-health chart) displays a child's physical growth and development.
- Developed by: David Morley.
- Designed for: Long-term monitoring of a child's growth.
- Typically plotted between: Weight and Age.
- Provides information on:
- Identification and registration.
- Birth date and weight.
- Chronological age.
- Weight-for-age.
- Developmental milestones.
- History of sibling health.
- Immunisation procedures.
- Introduction of supplementary foods.
- Episodes of illness.
- Child spacing methods used.
- Reasons for requiring special care.
WHO Home Based Growth Chart
- Includes2 reference curves:
- Upper Reference Curve (URC): 50th percentile for boys.
- Lower Reference Curve (LRC): 3rd percentile for girls.
- Road to Health:The space between the two growth curves (weight channel).
- Includes the normality zone for most populations, where 95% of healthy normal children fall.
- Based on NCHS Standards (USA):
- The 3rd percentile corresponds to approximately 2 SD below the median of weight-for-age reference value (URC).
WHO Service Growth Chart
- Contains 5 reference curves:
- 97th percentile of standard reference population.
- 50th percentile of standard reference population.
- 3rd percentile of standard reference population.
- 3rd SD value of standard median population.
- 4th SD value of standard median population.
Government of India Recommended Growth Chart
- Includes 4 reference curves:
- 80% of the median (50th percentile or URC) of the WHO reference standard
- 70% of the median (50th percentile or URC) of the WHO reference standard
- 60% of the median (50th percentile or URC) of the WHO reference standard
- 50%of the median (50th percentile or URC) of the WHO reference standard
- The 80% of the median corresponds to approximately 2 standard deviations (SD) below the median of the weight-for-age reference value (i.e., URC).
Understanding Growth Charts:
- 80% to 70% lines: Indicates 1st degree or Mild malnutrition
- 70% to 60% lines: Indicates 2nd degree or Moderate malnutrition
- 60% to 50% lines: Indicates 3rd degree or Severe malnutrition
- Below 50% line: Indicates 4th degree or IV grade malnutrition
ICDS Growth Chart (Based on the WHO MGRS Child Growth Standards 2006)
- The ICDS Growth chart includes 3 reference curves:
- Reference standard
- 2 SD below the reference standard
- 3 SD below the reference standard
Important Facts about Growth Charts
- The growth chart was initially created by David Morley and later improved by WHO.
- The best growth standards come from NCHS standards.
- Growth direction on a chart is more important than the exact position of the dots.
- Regular weight records are more helpful than a single weight measurement.
- The goal in child care is to maintain suitable growth based on individual health evaluations.
- A flat plot for a child suggests malnutrition.
- During malnutrition, the order of growth impact is weight, height, and then brain growth.
- There are 49 different types of growth charts used in India:
- Tool for Growth Monitoring
- Diagnostic tool for identifying high-risk children
- Planning and policy making
- Educational tool
- Tool for action
- Evaluation of corrective measures and impact of a programme
- Tool for teaching
- Growth Reference Values:
- Harvard (Boston) standards
- NCHS standards (WHO reference values)
- Indian standards (ICMR values)
Under Fives Clinic Concept
- The Under Fives clinic concept focuses on providing comprehensive health care for young children at a dedicated facility, utilizing the resources available within the country.
- Emblem for UF Clinic features Five Components:
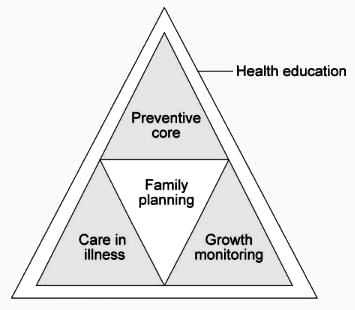 Under Five Clinic
Under Five Clinic
- Most effective workers in Under-Five Clinics: Mothers
School Health
Health Disorders among School Children
- Common health issues found in school children (listed by decreasing frequency):
- Dental defects: (180.3 per 1000)
- Goiter: (123.8 per 1000)
- Malnutrition: (123.5 per 1000)
School Health Examination
- In 1961, the Rennuka Roy School Health Committee established a comprehensive health programme for schools in India.
- Recommendation: Medical examination of children at entry and then every 4 years.
- NRHM [New Guidelines] suggests: Once every 6 months.
- School Eye Screening Programme:
- This programme focuses on middle schools (Classes V-VIII: ages 10-14 years):
- Teachers conduct screenings: 1 teacher for every 150 students (training or certification is recommended).
- Visual acuity cutoff for referral to PHC: <6/9
Healthful School Environment
- Minimum standards for sanitation in schools and their environments in India include:
- Location: Away from noisy areas; should be fenced.
- Site: Acres for primary schools; 10 acres for higher elementary schools.
- Structure: Exterior walls should be 10 inches thick and heat resistant.
- Classroom: Classroom for a maximum of 40 students.
- Per capita space: Greater than 10 sq. feet.
- Furniture: Single desks of 'minus (-) type.'
- Doors and windows: Area should be greater than 25% of the floor area.
- Colour: Inside wall colour should be white.
- Lighting: Natural light should come from the left side.
- Water supply: Safe, drinkable, and continuous supply through taps.
- Lavatory: Urinal per 60 students and 1 latrine per 100 students.
ICDS, IMNCI, BFHI
Baby-Friendly Hospital Initiative (BFHI)
- The Baby-Friendly Hospital Initiative (BFHI) aims to encourage and support breastfeeding in healthcare settings. The BFHI has established the Ten Steps to Successful Breastfeeding to guide hospitals and maternity facilities in implementing effective breastfeeding practices.
- Ten Steps to Successful Breastfeeding
- Written Policy: Every maternity care facility should have a written breastfeeding policy that is regularly shared with all healthcare staff.
- Staff Training: Train all healthcare staff in the skills needed to implement this policy.
- Information for Pregnant Women: Inform all pregnant women about the advantages and management of breastfeeding.
- Early Initiation: Assist mothers in starting breastfeeding within half an hour after birth.
- Breastfeeding Support: Show mothers how to breastfeed and maintain milk supply, even if they are separated from their babies.
- Exclusive Breastfeeding: Give newborns no food or drink other than breast milk, unless there are medical reasons.
- Rooming-in: Practice Rooming-in: Mothers and infants should stay together 24 hours a day.
- Breastfeeding on Demand: Encourage breastfeeding whenever the baby wants.
- Support Groups: Support the establishment of breastfeeding support groups and refer mothers to them when they leave the hospital or clinic.
- No Commercial Support: Stop any support from manufacturers of infant formula, baby food, or feeding bottl
- Desks of 'minus (-) type. Doors and windows area > 25% of floor area.
- 1 urinal per 60 students and 1 latrine per 100 students.
- The Anganwadi is at the center of the ICDS system.
- Prohibit the distribution of free or low-cost breast milk supplies.
- Provide extra lactation support to mothers with special circumstances, such as low birth weight or caesarean sections.
- Ensure a safe, healthy, and positive birthing experience for both mother and baby.
Integrated Management of Neonatal and Childhood Illness (IMNCI)
- IMNCI: IMNCI is a strategy aimed at reducing child mortality and morbidity by improving the management of common childhood illnesses. It integrates curative and preventive interventions for newborns and children up to 59 months of age.
- Objectives of IMNCI:The main objectives include:
- Reducing neonatal and childhood mortality rates.
- Improving the quality of healthcare services for children.
- Strengthening the health system to support effective implementation.
- Components of IMNCI:IMNCI consists of three main components:
- Improved Case Management: Training healthcare providers in the effective management of childhood illnesses based on updated guidelines.
- Health System Strengthening: Ensuring the availability of essential drugs, diagnostic tools, and guidelines at all levels of healthcare.
- Community and Family Involvement: Engaging families and communities in the care of sick children and promoting preventive measures.
- Training and Capacity Building: Capacity building of healthcare staff at various levels is crucial for the success of IMNCI. Training programs should focus on the latest evidence-based practices for managing childhood illnesses.
- Monitoring and Evaluation: Regular monitoring and evaluation of IMNCI implementation are essential to assess the impact and identify areas for improvement. This can include tracking health outcomes, service delivery indicators, and feedback from healthcare providers.
- IMNCI is a comprehensive approach that addresses the multifaceted challenges of neonatal and childhood illnesses through improved case management, health system strengthening, and community involvement.
Background of Integrated Child Development Services (ICDS)
- Establishment: ICDS was established in 1975 as a government initiative to provide integrated services for the growth and development of preschool children.
- Target Areas:The program primarily focuses on rural, tribal, and urban slum areas where children are at a higher risk of malnutrition and developmental issues.
- Global Recognition: ICDS is recognized as one of the largest and most comprehensive programs for early childhood development in the world.
- Central Government Funding: ICDS is centrally funded by the Government of India, ensuring uniformity and adequacy of resources across states.
- State Implementation:The program is implemented by state governments, with flexibility to adapt to local needs while adhering to national guidelines.
- Supplementary Nutrition: Providing additional nutrition to children and mothers to meet their dietary needs and prevent malnutrition.
- Health Check-ups: Regular health check-ups for children to monitor growth, development, and early detection of health issues.
- Medical Referral Services: Facilitating referrals to higher health facilities for children needing specialized medical care.
- Nutrition and Health Education: Educating women about nutrition, health practices, and childcare to empower them with knowledge for better family health.
- Non-formal Education: Providing non-formal education to children aged 3-6 years to prepare them for formal schooling and enhance their cognitive skills.
- Beneficiaries of ICDS
- Children aged 0-6 years: The primary beneficiaries who receive nutrition, health care, and education services.
- Pregnant and lactating mothers: Receiving nutritional support and health care services to ensure their well-being and that of their infants.
- Women of reproductive age: Targeted for nutrition and health education to improve their health status and prepare for motherhood.
- Adolescent girls aged 11-18 years: Benefiting from nutrition and health education to enhance their health and prepare for future roles.
- Anganwadi Centre
- Anganwadi Centres are the primary delivery points for ICDS services, with each centre catering to a specific population.
- Staff: Each Anganwadi centre is staffed by one Anganwadi Worker and one helper, who are responsible for implementing the program at the grassroots level.
- Coverage: Anganwadi centres are established at the ratio of 1 centre for every 400-800 people in rural and urban areas, and 1 centre for every 300-800 people in tribal areas. Mini-Anganwadi centres serve smaller populations of around 150 people.
- Supplemental Nutrition: Provided through ICDS with 300 feeding days per year, ensuring regular and adequate nutrition for beneficiaries. [New Gudilines 2013]
- Administrative Structure of ICDS:
- Administrative Unit:The Community Development Block serves as the administrative unit for ICDS, with each project covering a population of 100,000 in rural and urban areas, and 35,000 in tribal areas.
- Project Oversight: The Community Development Project Officer (CDPO) supervises the implementation of ICDS in the project area, overseeing 4 supervisors (Mukhyasevikas) and 100 Anganwadis.
- Each supervisor manages 25 Anganwadis, ensuring effective service delivery at the grassroots level.
- Kishori Shakti Yojana: Program for teenage females in ICDS
- ICDS in Bharat:Execution by Department of Female and Youth Welfare
- ICDS initiatives approved: 5422
- ICDS efforts operational: 5671
- Community centers active: 578,457
Kishori Shakti Yojana (KSY)
- Overview: KSY is a scheme under ICDS aimed at improving the nutrition and health status of adolescent girls.
- To enhance the nutritional and health status of adolescent girls, promote self-development, and raise awareness about various health and hygiene issues.
- Implementation: The scheme is implemented by the Ministry of Women and Child Development, covering 2000 ICDS projects.
- Under KSY:

Neonatal Screening
- Neonatal Screening: This is a secondary level of preventionaimed at identifying potential health issues in newborns.
- Main Disorder Screened: Neonatal Hypothyroidism (NNH)
- Disorders Screened in Neonates:
- Phenylketonuria (PKU)
- Sickle Cell Anemia
- Thalassemia
- Congenital Dislocation of the Hip
- G6PD Deficiency
- Phenylketonuria (PKU) and the Guthrie Test:
- PKU is an inherited disorder caused by a deficiency in the enzyme phenylalanine hydroxylase, leading to the accumulation of phenylalanine in the body.
- It is an autosomal recessive condition, occurring in approximately 1 in 10,000 births.
- Treatment for PKU: The primary treatment involves restricting or eliminating foods high in phenylalanine from the diet,
- Including such has:
- Breast milk
- Meat
- Chicken
- Fish
- Nuts
- Cheese
- Legumes
- Other dairy products
- Guthrie Test for PKU Screening:
- The Guthrie Test is a screening method used to detect PKU in newborns.
- It was the first test used for mass screening of neonates and involves collecting a blood sample from the baby by heel prick 7 to 10 days after birth.
- The test is negative in the first 2 to 3 days of life.
- Other Conditions Screened: While primarily used for PKU, the Guthrie Test may also screen for conditions.
- Including such as:
- Galactosemia
- Maple Syrup Urine Disease
- Chemicals Detected:
- The test detects levels of phenylalanine, phenylpyruvate, and phenyllactate in the blood.
- It is a semi-quantitative test, providing an estimate of the levels present.
- Current Practices: The Guthrie Test has been largely replaced by Tandem Mass Spectrometry, a more advanced and accurate screening method.
Neonatal Hypothyroidism
- Neonatal hypothyroidism (NNH) is the most frequently screened disorder in newborns, with an occurrence rate of about 1 in 4000 births.
- A primary cause of congenital hypothyroidism is iodine deficiency.
- Blood samples for screening are taken from cord blood, and the test measures T4 and TSH levels simultaneously.
- For a single test, T4 is more effective due to its better precision and reproducibility.
- Treatment for neonatal hypothyroidism involves a daily dose of thyroid hormone (thyroxine) taken by mouth.
Geriatrics
- The geriatric population in India constitutes 8.1% of the total population, with the age range for geriatrics being 60 years and above.
- The most prevalent health issue among Indian geriatrics is visual impairment, particularly cataracts.
- Cardiovascular disorders are the leading cause of death for Indian geriatrics over 70 years of age.
Miscellaneous
Sperm analysis [New WHO guidelines (2013]
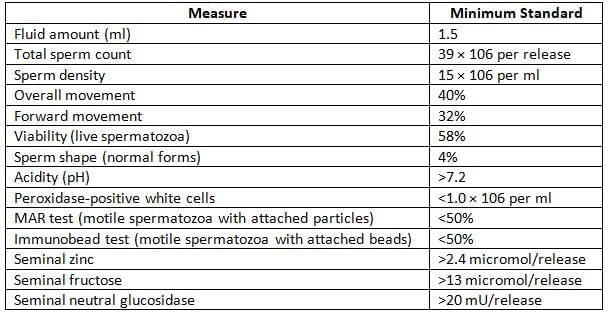
- Grading of sperm motility:
- Grade I: Immotile sperm (no movement at all)
- Grade II: Non-progressive motility (sperm tails move, but there is no forward movement)
- Grade III: Non-linear motility (curved or crooked movement)
- Grade IV: Linear progressive motility (straight-line movement)
Child Placement
- Orphanages: Institutions for children who lack a home or whose parents are unable to care for them.
- Foster Homes: Various forms of facilities designed to raise children outside of their biological families.
- Adoption: The legal process of adoption confers rights and responsibilities on the child and adoptive parents similar to those of natural parents.
- Borstals: Institutions for boys over 16 years old who are deemed too challenging for certified schools or who have exhibited misconduct there.
- Borstal sentence:. sentence usually lasting three years focused on the training and rehabilitation of young offenders.
- Remand Homes: Facilities where children are cared for by medical and trained personnel with the aim of enhancing their mental and physical health.
Borstals in India
- Borstal: Youths above 16 who are challenging to manage in an approved educational setting may be placed in a Borstal facility.
- Main aim of a Borstal: To ensure support, welfare, and recovery of young lawbreakers.
- Focus is placed on the learning process, training environment, and ethical guidance, creating a nurturing transformation setting.
- A Borstal sentence typically lasts for three years and is viewed as an approach for correction and renewal.
- Primary objective: To ensure the care, welfare, and rehabilitation of young offenders while keeping them away from harmful prison environments.
- Emphasis: On education, training, and moral guidance to promote reformation and prevent future criminal activities.
- Total inmate capacity: 2260
- Total inmate population: 1106 (Boys: 970; Girls: 136)
- Bombay Borstal School Act of 1929:This act empowers First Class Magistrates and Superior Courts to order detention in a borstal school instead of imprisonment for periods ranging from three to five years, applicable to young offenders.
- Boys: Age range of 16 to 21 years
- Girls: Age range of 18 to 21 years
Congenital Disorders in Newborns
- Congenital disorders are conditions that are primarily determined before or during birth and can typically be identified early in an infant's life.
- Global Incidence: Congenital disorders occur in 30 to 70 per 1000 live births worldwide.
- Affected Systems: The most frequently impacted systems are the cardiovascular and nervous systems.
- Incidence in India: Birth defects are present in 2.5% of newborns in India, rising to 4% by age 5.
- North India: The most prevalent birth defect is neural tube defects, such as spina bifida.
- Other Parts of India: The most common birth defect is musculoskeletal disorders.
Children in Challenging Situations
- Homeless children without a stable place to live.
- Children unable to be cared for by their parents.
- Children who have been separated from their parents.
- Migrant or refugee children facing displacement.
- Street children residing on the streets.
- Trafficked children being exploited for various purposes.
- Working children involved in labor.
- Children engaged in prostitution for survival.
- Children in bondage or forced labor situations.
- Children of sex workers facing societal challenges.
- Children with incarcerated parents experiencing family disruption.
- Children affected by armed conflicts and violence.
- Children impacted by natural disasters and their aftermath.
- Children living with HIV/AIDS and related stigma.
- Children suffering from terminal illnesses and their families.
- Girl children facing specific societal challenges.
- Children with disabilities and special needs requiring support.
- Children from minority groups including Scheduled Castes (SC) and Scheduled Tribes (ST).
- Children in institutional care and their living conditions.
- Children in conflict with the law and the justice system.
- Children who are victims of crime and their recovery.
- Birth defects in Indian newborns and their prevalence.
The document Preventive Obstetrics, Paediatrics and Geriatrics Chapter Notes | Preventive and Social Medicine (PSM) - NEET PG is a part of the NEET PG Course Preventive and Social Medicine (PSM).
All you need of NEET PG at this link: NEET PG
|
40 docs|6 tests
|
FAQs on Preventive Obstetrics, Paediatrics and Geriatrics Chapter Notes - Preventive and Social Medicine (PSM) - NEET PG
| 1. What is the Infant Mortality Rate (IMR) and how is it calculated? |  |
Ans. The Infant Mortality Rate (IMR) refers to the number of deaths of infants under one year of age per 1,000 live births in a given year. It is calculated using the formula: IMR = (Number of infant deaths / Number of live births) × 1,000. This rate is a critical indicator of the overall health of a population, reflecting the quality of maternal and child health services.
| 2. What are the main factors affecting the Infant Mortality Rate (IMR)? |  |
Ans. Several factors influence the Infant Mortality Rate, including socioeconomic status, access to healthcare, maternal education, nutrition, environmental conditions, and the prevalence of infectious diseases. Other factors such as maternal age, prenatal care, and the presence of skilled birth attendants also play significant roles in determining IMR.
| 3. How does the Neonatal Mortality Rate (NNMR) differ from the Infant Mortality Rate (IMR)? |  |
Ans. The Neonatal Mortality Rate (NNMR) specifically measures the deaths of infants within the first 28 days of life, while the Infant Mortality Rate (IMR) includes all deaths of infants under one year of age. NNMR is calculated using the formula: NNMR = (Number of neonatal deaths / Number of live births) × 1,000, making it a more focused indicator of early neonatal health issues.
| 4. What is the significance of the Maternal Mortality Rate (MMR) in public health? |  |
Ans. The Maternal Mortality Rate (MMR) is a crucial indicator of the quality of maternal healthcare services in a population. It measures the number of maternal deaths per 100,000 live births and reflects the risks associated with pregnancy and childbirth. A high MMR indicates deficiencies in healthcare access, quality of care, and the need for improvements in maternal health services.
| 5. What is the Child Survival Rate (CSR) and why is it important? |  |
Ans. The Child Survival Rate (CSR), also known as the Child Survival Index, represents the proportion of children who survive to a specific age, typically five years. It is important because it provides insights into the effectiveness of health interventions, nutrition, and overall living conditions for children. A high CSR indicates better health and survival prospects for children in a population, guiding policy and resource allocation.
Related Searches



















