Regional Injuries - 2 Chapter Notes | Forensic Medicine and Toxicology (FMT) - NEET PG PDF Download
Brain Injuries/Traumatic Brain Injury (TBI)
Types of Brain Damage
At the moment of a head injury, three primary types of brain damage may occur, either individually or in combination: diffuse neuronal injury, contusion, and laceration. Secondary effects, such as brain edema or intracerebral hemorrhage, may develop soon after the injury but are not primary damage.
Traumatic Brain Injury (TBI)
Traumatic brain injury (TBI) is a leading cause of death among individuals under 45 years old. Severe TBI can occur without direct mechanical impact, such as a blow or fall to the head. For instance, intracranial hemorrhage can result from mere shaking, as seen in Shaken Baby Syndrome in infants. Brain injury can occur with or without a skull fracture, and skull fractures may occur without brain damage.
Etiology of TBI
The primary causes of TBI include:
Relative Movement of Brain and Skull: The falx cerebri and tentorium cerebelli divide the cranial cavity into three compartments. These rigid structures, like the skull, restrict brain movement, potentially causing injury.
Penetrating Wounds of the Skull: Objects such as knives, bullets, or skull fragments from a depressed fracture can penetrate the brain, causing direct injury.
Skull Fracture and Distortion: Localized deformation or indentation of the skull can create shear strains in the underlying brain tissue, leading to contusions on the brain's surface. Fracture fragments may also penetrate the dura, resulting in brain laceration.
Mechanisms of Traumatic Brain Injury (TBI)
Biomechanics of TBI
The biomechanics of traumatic brain injury (TBI) focuses on the mechanical factors that lead to initial brain damage, which is essential for understanding the underlying processes of TBI.
Linear Acceleration Theory
- Proposed almost a century ago, this theory explains the movements and secondary impacts that occur between the skull and brain during a head impact.
- During a head impact, the linear acceleration of the head increases the pressure in the brain areas beneath the impact site.
- This theory primarily accounts for the formation of superficial brain injuries.
Holbourn's Hypothesis of Rotational Movement
- Proposed by Holbourn in 1943, this hypothesis suggests that TBI, especially deep brain injuries, occurs due to tensile strains between the superficial and deep brain structures during rotational head movements.
- Research by Thibault and Gennarelli has strongly supported the idea that rotational movements play a significant role in causing deep brain contusions and diffuse axonal injury (DAI).
Pressure Gradient and Tissue Strains
- TBI results from the varying pressure inside the brain during head trauma.
- The distribution of this pressure gradient affects tissue strains, including compression, tensile, and shear strains.
- It also influences the location of brain injuries and the resulting neurological symptoms.
Common Mechanisms of Traumatic Brain Injury
- Accelerating Injury: Injury that occurs due to rapid acceleration forces.
- Decelerating Injury: Injury resulting from rapid deceleration forces.
- Shear Strain/Rotational Injury: Injury caused by shear strains or rotational forces acting on the brain.
- Coup and Contrecoup Injury: Injury occurring at the site of impact (coup) and on the opposite side of the impact (contrecoup).
Accelerating Injury
- In an accelerating injury, when a moving object hits a stationary head, the skull initially gains momentum.
- The brain stays still for a short moment before it also starts moving.
- This kind of injury is called a coup injury.
- For example, if someone is struck on the head with a hockey stick, it can lead to a brain injury.
Decelerating Injury
- In a decelerating injury, when a stationary object suddenly stops a moving head, the skull loses momentum before the brain does.
- The brain then hits the inner surface of the skull before coming to a stop.
- This type of injury is known as a decelerating injury.
- For instance, a scooter or motorcycle rider colliding head-on with a pole or tree can suffer potential brain damage in such a scenario.
Shear Strain/Rotational Injury
- This type of injury occurs when there is side-to-side or rotational movement of the head.
- During such movement, the brain can shift and hit the sharp edges of the tentorial attachments and the bony buttresses located at the base of the skull.
- This impact can lead to injury.
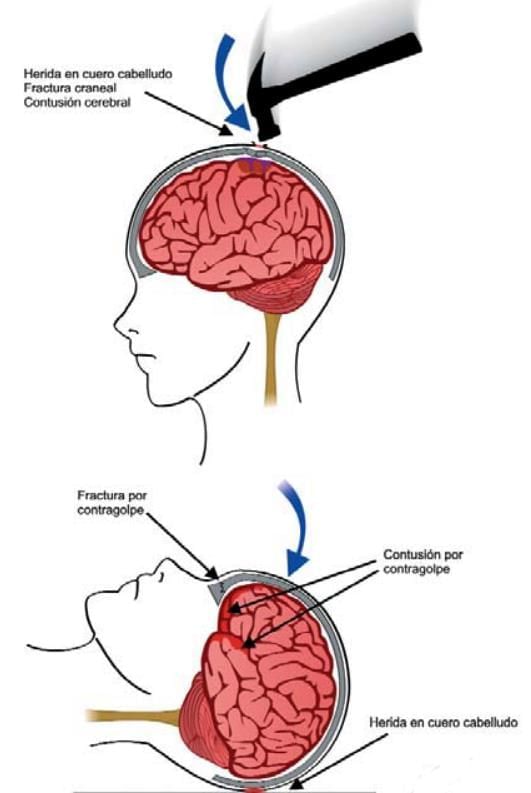
Coup Injury
- In a coup injury, both the skull and brain are injured at the site of impact.
- This type of injury is more likely to occur with blunt force blows to the head.
Contrecoup Injury
- A contrecoup injury involves damage to the skull and brain on the side opposite to where the impact occurs.
- This type of injury is more commonly seen in falls rather than direct blows to the head.
Role of Meninges and CSF in Preventing Traumatic Brain Injury (TBI)
- The meningeal layers cover the brain almost completely due to their normal attachments, helping to prevent side-to-side movement of the brain.
- The cerebrospinal fluid (CSF) acts as a flotation medium, providing a water cushioning effect that reduces the impact of forces acting on the brain from all directions.
- However, there are no anatomical structures to limit anteroposterior movement, making both ends of the brain susceptible to injury.
- As a result, traumatic brain injuries (TBI) can manifest as:
- cerebral concussion
- diffuse neuronal injury
- diffuse axonal injury (DAI)
- cerebral contusion
- cerebral laceration
- In real-life head trauma, all these conditions can occur simultaneously.
- Additionally, DAI and brain concussion can also happen in purely linear acceleration head-trauma experiments.
- Currently, the linear acceleration theory does not explain how injuries can occur in deeper brain structures while superficial structures remain unharmed. The emerging stereotactical theory aims to clarify these types of injuries.
Stereotactic Theory
- This is a newer method that examines the shape of the interface between the skull and the brain.
- It takes into account how the skull and brain interact during movements and the propagation of pressure waves.
- The interface between the skull and brain is approximately spherical in shape.
- Movements of the skull, whether due to linear or rotational acceleration and vibrations, generate secondary pressure waves with a spherical wavefront.
- Brain tissue is isotropic on concentric planes, meaning that the speed of wave propagation towards deeper brain structures is consistent.
C= (E/r) 0.5 , - Where C represents wave propagation speed, E denotes resilience, and r indicates density.
- The spherical shape of the wave front is preserved.
- However, its size and surface area gradually diminish.
- Despite energy loss, in accordance with the law of energy conservation, the strength of the pressure waves—and consequently the pressure difference—gradually increases towards deeper brain structures.
- This pressure is expected to be highest at the geometric centre of the affected skull segment, particularly if there has not been significant energy loss in the superficial brain areas.
- Stereotactical phenomena can provide insights into common post-traumatic neurological symptoms and brain injuries.
- These observations align with other biomechanical theories and have the potential to unify the understanding of traumatic brain injury (TBI) biomechanics.
- This understanding may also contribute to insights into TBI pathophysiology and related conditions such as chronic encephalopathy in boxers and Alzheimer's disease.
- Further experimental and observational research in the field of TBI biomechanics is crucial for advancing this understanding.
Cerebral Concussion (Commotio Cerebri)
Cerebral concussion refers to a condition characterized by a temporary or permanent disruption of nerve activity in the brain without any visible damage. This disruption can occur due to trauma to the brain, particularly from sudden stops or impacts. There are two types of cerebral concussion: reversible, which results from mild trauma, and irreversible, which is caused by severe trauma.
Reversible Cerebral Concussion
- In cases of reversible cerebral concussion, the patient may initially lose consciousness and experience muscle weakness, followed by a temporary return to consciousness. This period of regained consciousness, known as a lucid interval, can be misleading as the individual may later lose consciousness again. During the lucid interval, the person appears normal, fully aware of their surroundings, including time, place, and identity.
- However, signs of brain irritation may be present during this interval, often due to swelling in the brain. These signs can include small pupils and changes in blood pressure and breathing patterns.
- Medicolegal Importance: It is crucial to monitor individuals with head injuries for at least 24 hours, as they may develop extradural bleeding gradually, which can be life-threatening.
- Postconcussion Syndrome: After recovering from a concussion, individuals may experience postconcussion syndrome, which is characterized by symptoms such as headaches, dizziness, anxiety, emotional disturbances, and increased nervousness.
- Epilepsy: Severe head injuries can lead to post-traumatic seizures, which are important to consider in legal contexts. Electroencephalograms (EEGs) can be used to confirm whether a person is feigning this condition for personal gain.
- Retrograde Amnesia: Victims of head injuries may struggle to remember the circumstances surrounding the injury, including how it happened. This retrograde amnesia can last anywhere from two weeks to a month, and the duration of this amnesic period can indicate the severity of the injury.
- Punch-Drunk Syndrome:This syndrome involves confusion and physical impairment resembling Parkinson's disease and is caused by repeated head injuries. It is commonly seen in professional boxers and is known by various names, including dementia pugilistica. There are three stages of punch-drunk syndrome:
- First Stage: Mild coordination issues and emotional disturbances.
- Second Stage: Increased psychiatric symptoms, paranoia, and mild speech difficulties.
- Third Stage: Significant cognitive decline, memory issues, impaired hearing, and coordination problems.
- Drunkenness:. head injury can sometimes mimic the signs of being intoxicated, complicating the assessment of the individual's condition, especially in situations where they are taken into police custody.
- Alcohol and Head Injuries: If an individual has been consuming alcohol before sustaining a head injury, it can make the assessment more challenging. Additionally, recovery from a head injury may lead to confusion that resembles alcohol intoxication.
Differences between Drunkenness and Concussion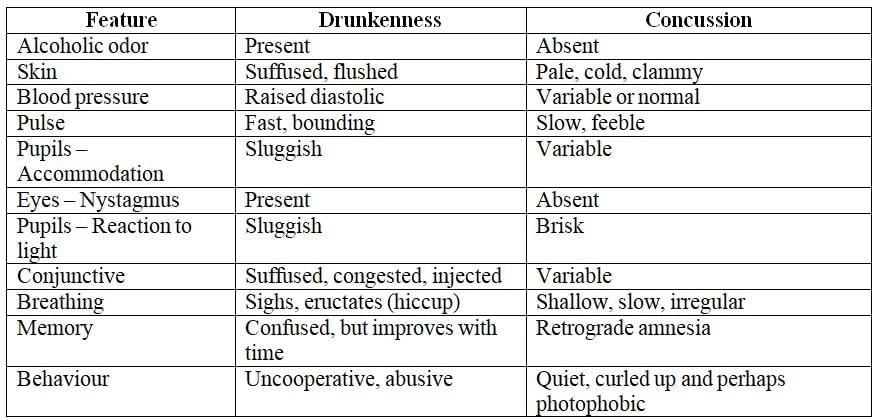
Note: Uncertainty prevails the patient should be hospitalised and kept under continuous neurological observation.
Irreversible Concussion
- Severe trauma can cause damage to the brainstem, which is vital for life, and this can lead to death.
- Post-mortem findings may not be very specific but often reveal small areas of bleeding in the brain.
Diffuse Neuronal Injury
- A strong impact can cause widespread injury to neurons and nerve fibres.
- This type of injury may be completely or partially reversible.
- Diffuse neuronal injury is likely caused by shear strains resulting from rotational movements.
Diffuse Axonal Injury (DAI)
- Diffuse axonal injury (DAI) is a severe type of brain injury and is among the most prevalent forms of brain trauma.
- DAI is seen in almost half of all cases of severe head trauma.
- This condition is categorized as a diffuse brain injury, indicating that the damage impacts a larger area of the brain compared to a focal brain injury.
- DAI usually involves extensive harm to white matter tracts in the brain and is a primary cause of unconsciousness and long-term vegetative states following head injuries.
- The majority of DAI cases result from traffic accidents, but it can also occur due to falls or physical assaults.
- In instances of DAI, there is an immediate loss of consciousness, often leading to a coma that lasts for more than six hours.
- The brain is made up of billions of nerve cells located in the grey matter, which communicate with each other through long nerve fibres known as axons found in the white matter.
- In DAI, the damage occurs due to shear strains that disrupt these axons and blood vessels at the moment of impact.
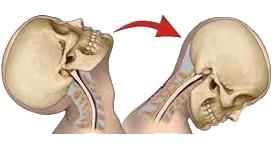
- Severe twisting or acceleration, such as what happens in whiplash injuries, can stretch and harm these fragile axonal fibres.
- On a microscopic level, this damage is termed Diffuse Axonal Injury.
- Although DAI commonly results from severe whiplash that leads to coma, research has indicated that it can also occur with a brief loss of consciousness.
- One of the challenges with DAI is that it is not detectable on CT or MRI scans because the injury is at a microscopic level.
Mild DAI
- In mild cases, axons in the white matter of the cerebral hemispheres, corpus callosum, and upper brain stem may be affected.
- Focal hemorrhages can be observed in the corpus callosum and dorsolateral rostral brainstem.
- Coma duration ranges from 6 to 25 hours.
Moderate DAI
- Coma lasts over 24 hours.
- There are no signs of brain stem dysfunction.
Severe DAI
- Coma lasts over 24 hours.
- There are signs of brain stem dysfunction.
Microscopic Examination Findings of Diffuse Axonal Injury (DAI)
- Microscopic examination does not reveal any signs of axonal injuries.
- 12 Hours to Days Post-Injury: Axons start to show changes:
- Dilated: Axons appear swollen.
- Club-Shaped: Axons take on a club-like shape.
- Retraction Balls: Round structures indicating cut axons begin to form.
- 2 to 3 Weeks Post-Injury: The number of retraction balls decreases.
- Microglial Cells: Clusters of these cells begin to appear.
- Astrocytosis and Demyelination: These processes start to occur.
- Electron Microscopy: Axonal injury can usually only be observed through this technique during the early stages following a closed head injury.
Understanding Diffuse Axonal Injury (DAI) and Biochemical Cascades
- Diffuse Axonal Injury (DAI) occurs when axons in the brain are stretched and torn, leading to the degradation of the axon beyond the site of the tear.
- Initially, it was thought that DAI was primarily caused by mechanical forces during trauma. However, it is now understood that secondary biochemical cascades, triggered by the initial injury, play a major role in axonal damage.
- These biochemical processes occur hours to days after the primary injury and are still not fully understood.
- During an injury, axonal stretching disrupts and breaks down the cytoskeleton, which is crucial for maintaining the axon's structure. This stretching also opens sodium channels in the axolemma (the axon's membrane), leading to the opening of voltage-gated calcium channels and an influx of calcium ions (Ca2+) into the cell.
- The increase of intracellular Ca2+ activates various pathways, including:
- Phospholipases
- Proteolytic enzymes
- These activated pathways cause damage to mitochondria and the cytoskeleton and activate secondary messengers, which can result in axonal separation and cell death.
- DAI typically presents with three main features:
- Gross focal lesions, such as haemorrhages and/or lacerations in the corpus callosum and brain stem.
- Microscopic evidence of axonal damage.
- Presence of retraction balls, which are indicative of axonal injury.
Cerebral Contusions
Cerebral contusions refer to the bruising of cerebral tissue within the brain. This type of injury may not always be accompanied by visible damage to the scalp or skull on the outside.
Cerebral contusions can result from various types of traumatic incidents, including:
- Coup and contrecoup injuries: These injuries occur when the brain strikes the inside of the skull (coup) and then rebounds to strike the opposite side (contrecoup).
- Shear strain injuries: These injuries result from the brain being subjected to rapid acceleration or deceleration, causing shear forces that lead to contusion.
- Blast injuries: Explosive forces can cause sudden changes in pressure and impact the brain, leading to contusions.
- Skull fractures:. fracture in the skull can directly impact the brain and cause contusions.
Common Sites of Cerebral Contusions
- Frontal Lobe: Contusions in the frontal lobe are common due to the brain's movement within the skull during trauma.
- Cerebellar and Medullary Contusions: These are often observed in cases of brain herniation, where the brain tissue is displaced and herniates through the foramen magnum.
Complications of Cerebral Contusions
- Cortical Atrophy: Over time, affected areas of the brain may undergo atrophy, leading to a reduction in brain tissue volume.
- Infection: There is a risk of infection following a cerebral contusion, which can lead to the formation of a brain abscess.
Cerebral Laceration
Cerebral laceration involves the tearing of brain tissue and is often associated with varying degrees of cerebral contusion.
- Affected Areas: Commonly impacts the frontal and temporal lobes of the brain.
- Types of Laceration:
- Superficial: Only the grey matter is affected.
- Deep: Only the white matter is affected.
- Critical Locations: Lacerations may occur in vital areas, including essential brain centres or within the brain's ventricles.
- Symptoms:. key symptom of cerebral laceration is the loss of consciousness.
Consequences of Cerebral Laceration
- Bleeding: Tearing of pial blood vessels can lead to significant bleeding.
- Swelling: The affected brain tissue may swell, exacerbating the condition.
- Increased Intracranial Pressure: The swelling and bleeding can result in increased intracranial pressure, which is a serious medical concern.
- Fatal Risk: If not treated promptly and effectively, cerebral lacerations can be potentially fatal.
Healing Process
Healing from cerebral laceration occurs through a process called gliosis, where glial cells proliferate and repair the damaged tissue.
Cerebral Irritation
- Cerebral irritation is a group of symptoms that can happen after a cerebral concussion.
- When someone experiences cerebral irritation, they often curl up in bed, covering their face with the blankets. They dislike being interrupted and are sensitive to bright light.
- Although they are aware of what is happening around them, they might react with aggression if someone disturbs them.
- These symptoms can either go away after a while, leading to a full recovery, or they might develop into post-concussion syndrome.
Cerebral Compression
- Cerebral compression occurs when there is increased pressure inside the skull, which interferes with normal brain function.
- This increased pressure on the brain stem can be caused by:
- Depressed skull fractures
- Foreign objects in the skull
- Swelling (edema)
- Bleeding (haemorrhage)
Pathology and Pathogenesis
- Generalized edema or space-occupying lesions that increase brain size lead to brain compression.
- The brain's inability to compress reduces the amount of cerebrospinal fluid (CSF) in the subarachnoid space and ventricles.
- Continued rise in intracranial pressure disrupts blood supply to the brain.
- If pressure exceeds the tentorium, it can push the uncus or inner edge of the temporal lobe into the midbrain.
- This can occur on one or both sides, causing lateral displacement and stretching of the midbrain.
- Stretching may rupture paramedian and nigral vessels, causing fatal hemorrhages in the midline and along the substantia nigra.
- Rarely, hemorrhagic infarction of the medial cortex of one occipital lobe may occur due to herniation affecting the posterior cerebral artery.
- The posterior cerebral artery can twist around the edge of the tentorium.
- Increase in pressure below the tentorium forces parts of the cerebellar lobes and tonsils through the foramen magnum, compressing the medulla oblongata.
- This compression can lead to respiratory failure.
- Uncal grooving and foraminal indentation of the cerebellar tonsils are common post-mortem findings.
- These should not be mistaken for evidence of uncinate herniation and cerebellar coning.
- Cerebral compression is suggested by unconsciousness following a head injury.
- Immediate unconsciousness indicates concussion, followed by a potential gradual regain of consciousness and subsequent loss due to compression.
- A "lucid interval" may occur between these stages of unconsciousness.
- In some cases, there may be no lucid interval, or initial consciousness may gradually decline due to compression.
- A large extradural hemorrhage can cause rapid compression within hours post-injury.
- A large subdural hemorrhage results in slower compression, requiring several days for sufficient blood accumulation.
- Delayed death after a head injury may occur due to a chronic subdural hematoma.
- Patients with head injuries should be monitored in hospital for at least 24 to 36 hours.
Autopsy Findings in Cerebral Compression
- Flattening of Gyri: The surface of the brain shows a flattening of the gyri, which are the raised folds of brain tissue.
- Narrowing of Sulci: The sulci, which are the grooves between the gyri, appear narrowed.
- Decrease of Cerebrospinal Fluid (CSF): There is an apparent decrease in the amount of cerebrospinal fluid.
- Deep Grooved Marking: There are deep grooved markings around the uncus of the temporal lobe and the cerebellar pressure cone.
Mechanism of Sleep and Unconsciousness
The reticular system in the brain stem plays a crucial role in maintaining an individual’s arousal and consciousness by receiving impulses from all parts of the body. Sleep occurs when there is reduced stimulation to this system. Irresistible sleep happens when the enzymes necessary for the reticular system's functions are depleted. Factors leading to sleep and unconsciousness include:
- Damage to the reticular system
- Reduction in afferent activity to the reticular system
- Action of toxic agents on the enzyme system of the reticular system
Injury to the brain stem can occur due to:
- Stretching of peduncles when the brain hemispheres shift
- Deceleration against the basisphenoid and dorsum sellae
- Lateral shift of the peduncle against the tentorial margin
- Stretching or avulsion of cranial nerves from the brainstem
- Traction on the vascular supply of the brain stem
- Pontine hemorrhage
Medicolegal Importance of Cerebral Compression
The diagnosis of cerebral compression is critical from a clinical and medicolegal perspective. Prompt identification of the underlying cause allows for surgical intervention, which can relieve the compression and is often a life-saving procedure.
Intracranial Hemorrhage
- Intracranial hemorrhage refers to bleeding within the cranial cavity. While skull fractures are a common cause, hemorrhage can occur without them, often due to underlying medical conditions.
- A detailed medical history and autopsy can clarify issues in cases of death from head injuries.
Causes and Features
- Trauma: Hemorrhage from trauma usually occurs on the brain's surface.
- Deep Bleeding: Trauma can also cause deep bleeding in the cerebrum, cerebellum, or brain stem.
- Accompaniments: Intracranial hemorrhage often accompanies brain contusions or lacerations from coup or contrecoup injuries.
- Intracerebral Hemorrhage:. single area of deep-seated intracerebral hemorrhage is typically associated with a disease process rather than trauma.
- Vulnerable Individuals: In people with arteriosclerosis or hypertension, emotional stress or intense physical activity can trigger intracerebral hemorrhage.
- Misleading Trauma: If such individuals fall and suffer a scalp injury, the hemorrhage may appear traumatic but could be due to underlying health issues.
Forensic Anatomy of Brain Membranes
The brain is protected by three membranes within the skull: the dura mater, arachnoid mater, and pia mater. These membranes play a crucial role in safeguarding the brain and are involved in various forensic considerations.
The dura mater is the tough outer layer of the membranes. It has bridging veins on its upper surface and contains arachnoid granulations, which are polyp-like projections extending into venous sinuses, particularly the sagittal sinus. These granulations facilitate the drainage of cerebrospinal fluid (CSF) into the bloodstream.
Beneath the dura mater is the arachnoid mater, a delicate and vascular membrane. The pia mater is not a true membrane but a network of glial fibers closely attached to the brain's surface. The subarachnoid space, located between the arachnoid and pia mater, contains CSF, which acts as a cushion for the brain. The width of this space can vary, being less than a millimeter in younger individuals and exceeding a centimeter in older adults with cerebral atrophy. This variation affects the length of the bridging vessels, making them more susceptible to damage from shearing and twisting forces.
Intracranial hemorrhages (ICHs) can occur due to various factors, including:
- Aneurysms, arteritis, blood disorders, and neoplasms.
- Injuries to the skull, brain, or their membranes.
- Effects of injuries on pre-existing conditions.
Graham and Gennareli classify intracranial hemorrhages into two categories:
- Intra-axial. Bleeding occurs within the brain tissue.
- Extra-axial. Bleeding happens outside the brain tissue.
I. Intra-axial Haemorrhage
Intra-axial haemorrhage refers to bleeding within the brain tissue itself. This category includes:
Intraparenchymal Haemorrhage: Bleeding directly within the brain tissue.
Intraventricular Haemorrhage: Bleeding into the brain's ventricles, often seen in premature infants.
II. Extra-axial Haemorrhage
Extra-axial haemorrhage involves bleeding inside the skull but outside the brain tissue. It is divided into three subtypes:
Extradural/Epidural Haemorrhage: Typically caused by trauma, often involving a laceration of the middle meningeal artery. This high-pressure bleed can rapidly increase intracranial pressure, making it life-threatening. Patients may experience loss of consciousness (LOC), followed by a lucid interval, then rapid deterioration with symptoms like vomiting, restlessness, and LOC. A head CT showing a lenticular (convex) shape is diagnostic.
Subdural Haemorrhage: Occurs due to tearing of bridging veins in the subdural space between the dura and arachnoid mater. A crescent-shaped deformity is visible on head CT.
Subarachnoid Haemorrhage: May result from trauma, aneurysm rupture, or arteriovenous malformations. Blood pools in the sulci, fissures, or cisterns (commonly the suprasellar cistern due to the Circle of Willis). It typically presents with a sudden, severe headache and requires urgent neurosurgical evaluation, often necessitating immediate intervention.
Extradural Hemorrhage (EDH)
Extradural hemorrhage, also known as epidural hemorrhage, is a form of intracranial bleeding that takes place outside the dura mater.
Incidence
- Adults: Commonly seen.
- Young Adults: In this age group, the meningeal arteries are situated close to the skull bone. As a result, fractures in the skull near these arteries can lead to their injury.
Common Causes Encountered in Routine Medicolegal Practice
- Fracture of the Temporal Bone: Particularly in the squamous part, this type of fracture can rupture the middle meningeal artery or vein, causing significant bleeding into the temporal fossa.
- Fracture of the Frontal Bone: This fracture may rupture the anterior meningeal artery or vein, leading to bleeding in the anterior cranial fossa and potential compression of the frontal lobe.
- Fracture of the Occipital Bone: Such a fracture can rupture the posterior meningeal artery or vein, resulting in bleeding in the posterior cranial fossa. This can create a large hematoma that exerts pressure on the cerebellum and occipital lobes. Hematomas thicker than 2 cm are particularly concerning as they can compress vital centres (medulla and pons), potentially leading to immediate death.
- Fracture of the Vault: This type of fracture can rupture the superior sagittal sinus or diploic veins, leading to hematoma formation.
Blood accumulation in the extradural space can exert pressure on the brain and increase intracranial tension. These factors may result in loss of consciousness. Over the course of a few hours or days, the patient may enter a coma, exhibiting symptoms similar to intoxication. Without appropriate treatment, death may occur rapidly.
Clinical Findings
- Dilated pupil on the same side (ipsilateral)
- Weakness on the opposite side (contralateral)
- Period of clarity (lucid interval)
- Involuntary movements (automatic movements)
Autopsy Finding
- Blood clot in the extradural space, which may require surgical removal.
- Possible volitional activities immediately after injury or before death.
- Potential for a lucid interval.
- Risk of being mistaken for alcohol intoxication, leading to false charges of drunkenness.
Subdural Haemorrhage (SDH)
Subdural haemorrhage is a type of bleeding that occurs inside the skull, specifically beneath the dura mater, which is one of the protective membranes covering the brain. This condition is commonly observed in children and older adults, and it rarely occurs in isolation. It is often associated with another type of bleeding called subarachnoid haemorrhage.
Causes:
- Vein Stretching and Tearing: Subdural haemorrhage can occur when there is movement between the dura and arachnoid mater, leading to the stretching and tearing of veins in the subdural space.
- Brain Injuries: Bruises or cuts to the brain can also cause subdural bleeding.
- Minor Head Trauma in Older Adults: In older individuals, even minor head trauma from sudden movements can result in bilateral subdural haemorrhages.
- Spontaneous Reasons: There are also spontaneous causes for subdural haemorrhage, although these are less common.
Symptoms:
- Early Symptoms: Initially, symptoms may be subtle and include slight confusion, forgetfulness, and mood changes. These early symptoms can be mistaken for conditions like schizophrenia in young patients or dementia in older patients.
- Chronic Subdural Hematoma: If the condition progresses, it can lead to the formation of a chronic subdural hematoma, which is a blood cyst on the brain's surface. This occurs because the subdural space lacks a mesothelial lining, making it difficult for the bleeding to resolve.
- Asymptomatic Cases: In some cases, the blood cyst may be asymptomatic and go unnoticed, potentially until an autopsy. In rare instances, this can lead to sudden death.
Affected Areas:
- Subdural haemorrhages can affect various regions of the brain, including the: Frontal RegionParietal RegionTemporal RegionBasal Region
- Unilateral or Bilateral: The haemorrhage can be unilateral (affecting one side) or bilateral (affecting both sides) of the brain.
Types of Subdural Haemorrhage:
- Acute Type: This type is usually identified only during autopsy.
- Subacute Type: Symptoms of this type appear within 2 to 14 days after the haemorrhage.
- Chronic Type: In this type, symptoms are delayed and may appear after a few weeks or more.
Symptoms by Type:
- Acute Type: Unconsciousness is a common symptom.
- Subacute Type: Symptoms may include mild headache, speech difficulties, and urinary issues.
- Chronic Type: Symptoms may include speech difficulties and urinary issues.
Autopsy Observations
- Acute Cases: During autopsy of acute cases, a blood clot in the subdural space is observed, which cannot be washed out.
- Chronic Cases: In chronic cases, a blood cyst may be present. Chronic conditions can also elevate the risk of sudden natural death.
- Clinical Confusions:The clinical symptoms of these conditions may sometimes be mistaken for:
- Schizophrenia in young individuals.
- Presenile or senile dementia in older individuals.
- Instances of lucid intervals.
Subarachnoid Hemorrhage (SAH)
Subarachnoid hemorrhage is a type of intracranial bleeding that occurs in the subarachnoid space, the area between the brain and the thin tissues covering it (see Fig. 17.12D, Fig. 17.13C).
Causes and Mechanisms: SAH can arise from two primary mechanisms: traumatic and spontaneous origins.
- Traumatic SAH: Prolonged neck hyperextension, such as during procedures like bronchoscopy, may cause tears in the basal vertebral arteries, leading to SAH.
- Spontaneous SAH: This can result from:
- Conditions such as atherosclerosis, hypertension, or leukemia.
- Congenital defects, such as berry aneurysms or miliary aneurysms in the basilar arteries, which may rupture with minimal trauma.
Location: SAH may initially present as a unilateral or bilateral lesion, either at the site of impact (coup) or opposite it (contrecoup). However, the blood typically spreads across the brain soon after.
Pathology: Unlike other hemorrhages, SAH does not typically form a hematoma. The blood is cleared through lysis or phagocytosis, allowing for potential full recovery in some cases.
Clinical Presentation: The hallmark symptom is a sudden loss of consciousness. Patients may also experience a "thunderclap headache," described as the most severe headache ever, developing rapidly over seconds to minutes.
Autopsy Findings: At autopsy, the arachnoid mater often shows a characteristic yellowish-brown discoloration due to the presence of blood.
Medicolegal Significance: Determining whether trauma caused the rupture of an aneurysm is critical. This is often supported by a history of persistent or severe headache (thunderclap headache) following trauma, which continues until the aneurysm ruptures.
Intracerebral Hemorrhage (Parenchymatous Hemorrhage)
Intracerebral hemorrhage involves bleeding within the cerebral tissue itself. This condition can arise due to trauma or various medical issues affecting the blood vessels in the brain.
- Rupture of Berry Aneurysms: These are small, bulging areas in the blood vessel wall that can burst, leading to bleeding in the brain.
- Intracerebral Stress or Impact: Forceful impact to the brain can cause tears in the blood vessels, resulting in hemorrhage.
- Frontal Impact:. strong blow to the front of the skull can cause the skull to expand and the brain ventricles to separate, potentially leading to bleeding.
- Cerebral Contusion: Intracerebral hemorrhage is often associated with bruising of the brain tissue, known as cerebral contusion.
- Displacement of the Falx Cerebri: This refers to the shifting of a membrane that separates the two hemispheres of the brain, which can occur during severe trauma and contribute to bleeding.
- Skull Fracture:. fracture in the skull can damage blood vessels and lead to intracerebral hemorrhage.
Size
- Petechial haemorrhage is less than 2 mm, while haematoma is larger.
- Occurs at the boundary between grey and white matter in the brain.
- Involves the collection of nuclei in the brain.
- During an autopsy, it is crucial to determine whether the haemorrhage is post-traumatic or spontaneous (apoplexy).
Intraventricular Haemorrhage
- Occurs when there is bleeding in the brain ventricles.
- Isolated cases are extremely rare.
- Typically occurs alongside more extensive intracranial bleeding due to a vascular malformation in the choroid plexus.
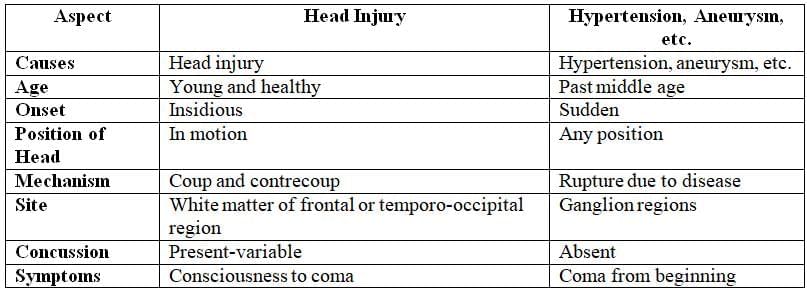
Differences between haemorrhage due to head injuries and diseases
Pontine Haemorrhage
Pontine haemorrhage refers to a specific kind of intracranial bleeding that occurs within the pons, a part of the brain stem. This condition is often associated with individuals who have high blood pressure. In some cases, such as following an accidental fall or a traffic accident, a pontine haemorrhage can be mistakenly identified, complicating the diagnosis.
Types of Pontine Haemorrhage
- Spontaneous Pontine Haemorrhage: In this type, bleeding occurs spontaneously in a single area of the pons, which can occupy one-third to half of the pons.
- Traumatic Pontine Haemorrhage: This type involves multiple separate areas of bleeding that may eventually merge into a larger area if the individual survives long enough. Both spontaneous and traumatic haemorrhages can involve bleeding into the fourth ventricle.
Primary haemorrhages in the brain stem are typically small and located near the walls of the third and fourth ventricles, as well as the aqueduct.
- Rostral Brain Stem: Haemorrhages in the rostral brain stem are generally more numerous and severe compared to those in the medulla.
- Medulla: Injuries in the medulla often result in rapid fatal outcomes.
Many individuals who die after prolonged unconsciousness exhibit signs of brain stem injuries, indicating the severity of such conditions.
|
68 docs|3 tests
|
FAQs on Regional Injuries - 2 Chapter Notes - Forensic Medicine and Toxicology (FMT) - NEET PG
| 1. What are the different types of traumatic brain injuries (TBI) and how do they differ from one another? |  |
| 2. What are the common causes and risk factors associated with intracranial hemorrhage? |  |
| 3. How do symptoms differ between extradural and subdural hemorrhages? |  |
| 4. What role does imaging play in the diagnosis of intracranial hemorrhages? |  |
| 5. What are the potential long-term effects of traumatic brain injury and intracranial hemorrhage? |  |















